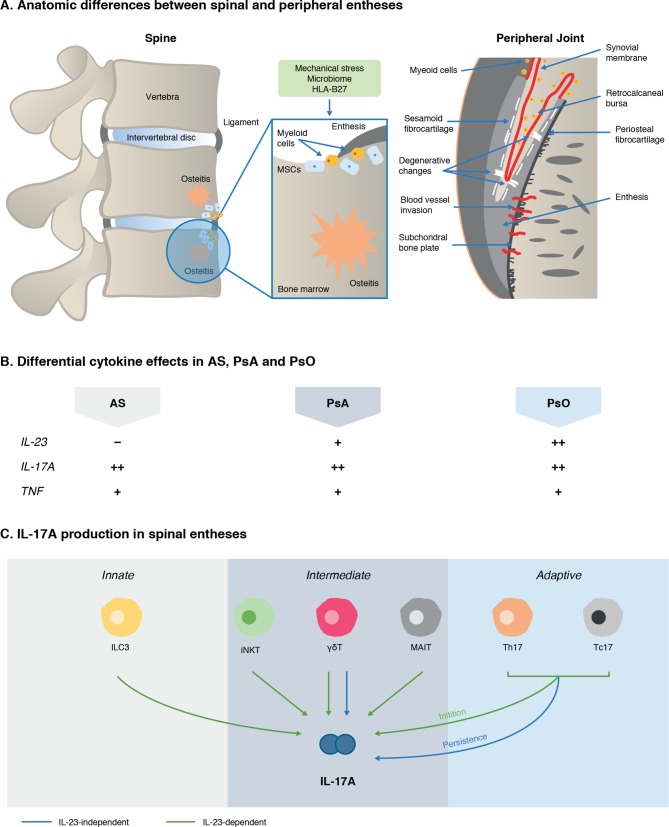
Figure 5.
Emergent scheme to explain IL-23/–17 axis pathway divergence in PsA and AS. IL-23 pathway blockade is highly effective in psoriasis but not in AS, which is unexpected given the IL-23 SNPs and related gene SNPs associated with AS. Anatomical differences between entheses in the spine versus peripheral joints could play a role (A). The peripheral skeleton has numerous synovio-entheseal complexes,173 which contain abundant myeloid cells, while these cells are rare in the spine. Spinal enthesitis is also associated with peri-entheseal bone disease and osteitis.59 173 238 The role of inflammatory cytokines, namely IL-23, IL-17A and TNFα, also differs across the spondyloarthritidies (B).12 14–16 167 168 172 239–248 IL-17A can be produced by several different sources in spinal entheses (C).56–59 74 75 81 82 99 100 158 175 249 Emerging evidence supports the cellular basis for IL-17 production that is independent of IL-23.56 57 158 175 Animal models also show that IL-23 has a redundant role once adaptive immunity is primed.175 Where ++, strong involvement; +, involvement; –, no involvement. AS, ankylosing spondylitis; γδT, gamma delta T cells; HLA-B27, human leucocyte antigen B27; IL-17A, interleukin 17A; IL-23, interleukin 23; ILC3, Type three innate lymphoid cells; iNKT, innate natural killer T cell; MAIT, mucosal associated invariant T cell; MSCs, mesenchymal stem cells; PsA, psoriatic arthritis; PsO, psoriasis; Tc17, CD8+T cells; Th17, T helper 17 cells; TNF, tumour necrosis factor α.