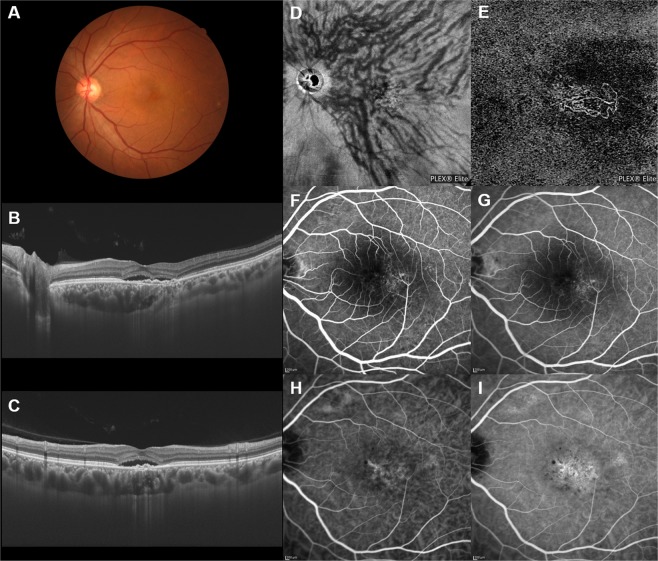
Figure 3.
Images of an eye with pachychoroid neovasculopathy in a 54-year-old man. The refraction in the left eye was −1.00 diopter. Best-corrected visual acuity in the left eye was 0.22 logarithm of the minimum angle of resolution unit. (A) Color fundus photograph shows a retinal pigment epithelium (RPE) abnormality at the macular area. (B,C) 12 mm horizontal and vertical B-mode OCT images through the fovea show pachychoroid with dilated outer choroidal vessels (vortex veins). Dilated vortex veins are notable between the papilla and subfovea in the horizontal B-mode OCT image. A shallow irregular RPE detachment accompanied by serous retinal detachment is observed at the fovea. The central choroidal thickness is 386 µm. (D) En face OCT image (12 mm × 12 mm) showing dilated vortex veins in the deep layer of the choroid. Superior and inferior vortex veins are symmetrical. The horizontal watershed zone has disappeared, with collateral veins due to anastomoses between the superior and inferior vortex veins instead being observed in the peripapillary area. (E) OCT angiography (3 mm × 3 mm) shows network vessels of choroidal neovascularization (CNV) between the detached RPE and Bruch’s membrane. CNV was detected over the dilated vortex veins. (F,G) Fluorescein angiography (early and late phases) shows window defects and some oozing at the macular area. (H,I) Indocyanine green angiography (early and late phases) shows suspected CNV at the fovea and choroidal vascular hyperpermeability around the fovea.