Abstract
Objective
To explore healthcare providers’ perspective on non-communicable disease (NCD) prevention and management services provided through the NCD corners in Bangladesh and to examine challenges and opportunities for strengthening NCD services delivery at the primary healthcare level.
Design
We used a grounded theory approach involving in-depth qualitative interviews with healthcare providers. We also used a health facility observation checklist to assess the NCD corners’ service readiness. Furthermore, a stakeholder meeting with participants from the government, non-government organisations (NGOs), private sector, universities and news media was conducted.
Setting
Twelve subdistrict health facilities, locally known as upazila health complex (UHC), across four administrative divisions.
Participants
Participants for the in-depth qualitative interviews were health service providers, namely upazila health and family planning officers (n=4), resident medical officers (n=6), medical doctors (n=4) and civil surgeons (n=1). Participants for the stakeholder meeting were health policy makers, health programme managers, researchers, academicians, NGO workers, private health practitioners and news media reporters.
Results
Participants reported that diabetes, hypertension and chronic obstructive pulmonary disease were the major NCD-related problems. All participants acknowledged the governments’ initiative to establish the NCD corners to support NCD service delivery. Participants thought the NCD corners have contributed substantially to increase NCD awareness, deliver NCD care and provide referral services. However, participants identified challenges including lack of specific guidelines and standard operating procedures; lack of trained human resources; inadequate laboratory facilities, logistics and medications; and poor recording and reporting systems.
Conclusion
The initiative taken by the Government of Bangladesh to set up the NCD corners at the primary healthcare level is appreciative. However, the NCD corners are still at nascent stage to provide prevention and management services for common NCDs. These findings need to be taken into consideration while expanding the NCD corners in other UHCs throughout the country.
Keywords: public health, health policy, organisation of health services, service delivery, non-communicable disease, health services administration & management
Strengths and limitations of this study.
This study is the first to assess the non-communicable disease (NCD) services provided through the government-led NCD corners in Bangladesh and to identify challenges and opportunities to strengthening NCD services at the primary healthcare level.
We conducted 15 in-depth qualitative interviews with the public sector healthcare providers, collected data on the NCD service readiness using a health facility observation checklist and conducted a stakeholder meeting.
Findings of this study are supportive of the national policy to expand NCD corners for improving NCD prevention and management services at the primary healthcare level.
This study was unable to capture information beyond four administrative divisions, hence limiting the generalisability of our findings, and we did not collect data from patients, which could have added additional insights from the consumers’ perspective.
Introduction
Like other low-income and middle-income countries, Bangladesh is experiencing rapid demographic and epidemiological transitions1–3 and subsequent rise in ageing population and the burden of non-communicable diseases (NCDs).2–4 The Global Burden of Disease study estimated that the proportion of deaths due to NCDs in Bangladesh increased from 43.4% in 2000 to 66.9% in 2015.5 This increasing trends of NCDs poses a major challenge for the Bangladesh’s existing healthcare systems, which are mainly geared towards addressing communicable diseases.6 7 The impact of NCDs on national economy, communities, families and individuals is unbearable,8 9 and this is likely to be more serious in coming years, as the number of people with the risk of developing NCDs increases.10–12 Recent studies have shown that NCD risk factors such as overweight, underweight, hypertension, dyslipidaemia, physical inactivity, tobacco smoking and low consumption of vegetables were common among adults living in urban13–15 as well as rural areas14 16 including adults of all economic quintiles.8
In recent years, the government of Bangladesh has taken initiatives to combat NCDs at system, institutional and service delivery levels.17 18 A national NCD plan has been developed; and a dedicated NCD control unit housed within the Directorate General of Health Services (DGHS), Ministry of Health and Family Welfare, was established in 2011.18 19 In 2012, the government initiated a new initiative, NCD corner at Upazila (subdistrict) health complexes (UHCs) for addressing NCDs. These NCD corners are dedicated to providing prevention and care services for common NCDs and related conditions such as cardiovascular diseases (CVDs), diabetes and chronic respiratory diseases (asthma and chronic obstructive pulmonary disease (COPD)) and screening for certain cancers.6
Though the national guidelines for NCD surveillance have been developed, the implementation of these guideline has remained weak.7 NCD prevention and management services are not yet systematically offered at the union level and all upazilas, where the medical doctors are posted.20 While the government plans to expand the NCD corners to other upazilas, to date, no robust information is available to explain the current situation of these NCD corners. It is important to determine how these NCD corners are functioning, what are the challenges and gaps along the implementation process and service delivery and how these NCD corners could be strengthened and institutionalised at the primary healthcare level. Thus, the aims of the study were twofold: (1) to explore healthcare providers’ perspective on NCD prevention and management services provided through the NCD corners in Bangladesh and (2) to examine challenges and opportunities for strengthening NCD delivery services at the primary healthcare level.
Methods
Setting
Bangladesh currently has seven administrative divisions, which are divided into 65 districts, called as Zila, and 493 subdistricts, called as upazila. In each upazila, there is one health complex, named as upazila health complex (UHC). In this study, 12 purposively selected NCD corners located at 12 UHCs (one NCD corner per UHC) of four administrative divisions—namely, Dhaka, Sylhet, Khulna and Chittagong—were included.
Study design
We used a grounded theory approach21 22 involving in-depth qualitative interviews with healthcare providers. Grounded theory has considerable significance to qualitative research involving participants from the diverse background. This approach provides explicit, sequential guidelines for conducting qualitative research; offers specific strategies for handling the analytic phases of inquiry; streamlines and integrates data collection and analysis process; and advances conceptual analysis.21 Participants’ perceptions on and awareness of the current situation of NCDs and approaches to address them were explored through in-depth qualitative interviews and a stakeholder meeting with healthcare providers. An NCD corner facility checklist was developed and was used to audit NCD corners. During the stakeholder meeting, we presented preliminary study’s findings and gathered feedback, comments and suggestion from participants to supplement and verify the information from in-depth interviews and the observation checklist. Participants for the stakeholder meeting were representatives from the government, NGOs, private sector, universities and news media.
Sampling strategy
A multistage sampling strategy was used (See figure 1). A list of UHCs and NCD corners according to the administrative divisions and the respective districts was prepared. Twelve NCD corners of four administrative divisions were selected using convenience sampling and ensuring representation of diverse geographical areas including haor (wetland area), coastal, rural and hill tract. Participants for in-depth interviews were the Upazila Health and Family Planning Officer (UH&FPO) in-charge of the UHC and medical officers responsible for managing NCD services through NCD corners. An inventory of staff responsible for providing NCD services through the NCD corners was undertaken, then the participants were purposefully selected to achieve diversity in terms of experience, level of appointment and field of training.
Figure 1.
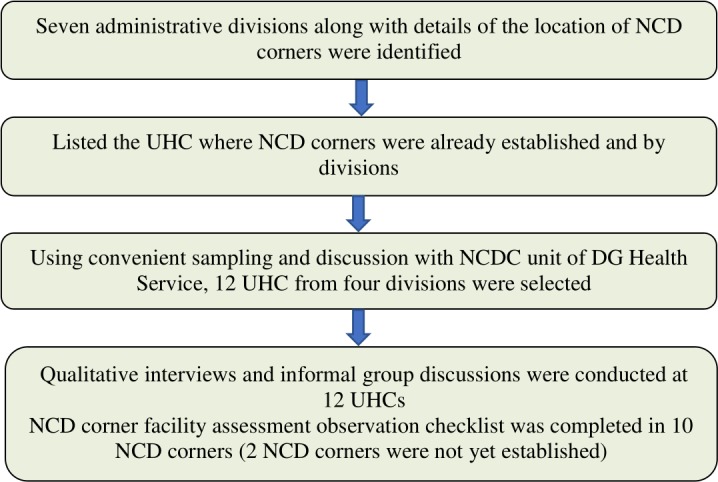
Flow chart describing sampling strategy and data collection process in the study. DG, director general of health services; KII, key informant interviews; NCD, non-communicable disease; NCDC, NCD control unit; UHC, upazila health complex
Study tools development
An in-depth interview guide was developed and informed by an extensive review of relevant literature, government reports and guidelines, available relevant tools and consultation with government officials at DG health services and the Ministry of Health and Family Welfare. The study team and NCD experts reviewed the in-depth interview guide for clarity and comprehensiveness to suit the different levels of NCD service provision. A health facility checklist was developed based on the review of available tools and relevant studies in Bangladesh, particularly the Bangladesh Health Facility Survey (2014),23 and a list of essential and NCD drugs and supplies by DGHS.
Ethics approval and consent to participate
Prior to interviews, participants were fully informed about the study objectives and how obtained data will be used. All interviews were audio-recorded; hence, informed written consent was obtained prior to the interview as well as for audio recording.
Data collection
Data were collected from 12 NCD corners of four administrative divisions. An NCD corner facility checklist was not used in Ramu and Teknaf UHCs as NCD corners were established in these locations during the data collection period. Three main approaches were used for data collection: (1) in-depth qualitative interviews, (2) an NCD services facility checklist and (3) a stakeholder meeting. Fifteen key informant interviews were conducted. Given the language proficiency of healthcare providers, all interviews were conducted in English by the principal investigator (LBR) of the study. The investigator was trained in qualitative research and had no prior relationship with any of the participants. The interviews were audio-recorded, and detailed notes were taken during the interview. We achieved the data saturation with 10 participants but kept the recruitment process continuing to ensure the participants were well representative from all geographical areas including haor (wetland area), coastal, rural and hill tract. The health facility checklist with major areas of: (A) availability of basic infrastructure, (B) equipment and supplies, (C) laboratory facility, (D) human resources for health and (E) NCD essential drugs and other relevant medications was used. A stakeholder meeting with participants from government, non-government organisations (NGOs), private sector, universities and news media was conducted, and their feedback, comments and suggestions were incorporated.
Patient and public involvement
No patient or public was involved.
Data processing and analysis
The audio-recordings of the interviews were transcribed verbatim by one of the research team members (TB). Coding of the transcripts and the identification of emerging themes were carried out using a thematic approach as recommended by Nowell et al.24 The conceptual mapping of the themes emerging from the data was achieved by careful reading and rereading of transcripts against the research question. The process of coding involved an inductive approach, and the common themes were identified by comparing and contrasting the patterns and meanings as expressed by participants. Two researchers (LBR and TB) independently read the transcripts, did the coding and analysed the qualitative data, and these were further checked by another two researchers (KK and MIT) for accuracy. All team members reviewed the final themes, and a consensus was achieved resolving the discrepancies through discussion. A final set of six major themes were identified, and the qualitative findings are presented, accordingly. Participants were deidentified throughout the transcription to ensure the confidentiality and anonymity, and the pseudonyms (such as MO, UH&FPO, RMO and CS) were used when illustrating participants’ voice.
The collection and analysis of data from 15 in-depth interviews adhered to the Standards for Reporting Qualitative Research (SRQR),25 and strategies were employed to enhance the trustworthiness (credibility, transferability, dependability, and confirmability) of the study findings.26 27 This included checking the data for accuracy, organising debriefings for completeness of data (KK and MIT), using team meeting for coding consensus and providing adequate information about the participants, study settings and data collection as well as use of direct quotes of the participants to support the findings (see Appendix A, SRQR Checklist as online supplementary document).
bmjopen-2019-029562supp001.pdf (103.9KB, pdf)
Results
Participants
Participants for the qualitative interviews (n=15) included upazila health and family planning officers (n=4), resident medical officers (n=6), medical doctors (n=4) and civil surgeons (n=1). Of the 15 participants, 12 were men and 3 were women, and their duration of employment ranged from 18 months (for resident medical officers) to the 15 years (for civil surgeon). All participants, except civil surgeon, were based at the UHC and were responsible for the provision of clinical and preventive health services. Civil surgeon was based at the district hospital and was responsible for the overall management of health service delivery in its catchment area. Participants for the stakeholder meeting were government health managers and health policy makers working at the DGHS, Ministry of Health and Family Welfare; researchers and academicians from different research institutes and universities; representatives from international and national non-governmental organisations; private health practitioners; and representatives of news media.
Participants noted that the burden of NCDs in Bangladesh is increasing rapidly, and the government’s initiative to establish NCD corners at the UHC level was timely. Participants also highlighted several challenges including the shortage of human resources, inadequate capacity building in NCD prevention and management, limited supplies of drugs and logistics and poor monitoring of service delivery and coordination mechanisms. The findings are presented in following themes.
NCDs’ current scenario
Participants remarked that, in Bangladesh, the burden of NCDs and number of patients experiencing NCD-related problems are increasing rapidly in both urban and rural settings. The most common reasons for patients’ visit to NCD corners were diabetes, CVDs and COPD, followed by other associated non-communicable conditions such as mental health, cancers and road traffic accidents. Participants noted that, in most cases, patients visit health facilities not knowing that they have developed NCD conditions. As one participant explained:
It is somehow difficult to identify patients with NCDs as people do not usually come to treat NCDs. Rather, the patients come with general sickness and sometime even hide or forget to mention symptoms that might help us identify NCD cases. MO, Ramu UHC, Chittagong
NCDs’ service readiness (physical and human resources, equipment, logistics and drugs)
Despite the increasing burden of NCDs in Bangladesh, the readiness in terms of access to and utilisation of NCD services has remained one of the major challenges. Participants noted that NCD corners have basic equipment required to provide basic NCD services sphygmomanometers, weighing scales and height measurement boards. One NCD corner had a glucometer set available, but the supplies were inadequate, and in most cases glucometer strips and batteries were out of stock, making the available glucometer test set unusable. As one participant note:
BP machine and glucometer set along with other measuring tools are available in our NCD corner. But the problem is that we don’t have enough glucose measuring strips. MO, Munshiganj, Dhaka
Participants stressed the importance of developing a dedicated NCD team that could provide comprehensive NCD services more effectively. However, they highlighted the challenges associated with running NCD corners, noting that there are no designated positions such as medical officers, paramedics or nurses specifically attached to NCD corners. In general, medical officers and other staff are assigned locally and attached to the health facility in charge.
There is no such team working here at the NCD corner. Only the NCD MO is working for NCD corner. The senior nurse and a paramedic are involved but not dedicated to NCD corner, they are responsible to overall OPD services. MO Devbhata, Khulna
Adequate and regular supply of logistic services and drugs is essential for the provision of NCD services. However, participants remarked that logistic services and monthly drug supplies from the district health office were deficient and not actioned on a regular basis.
We always try to provide whatever medicines are available at the dispensary, but in most cases, we have a stock-out of NCD drugs, so patients are advised to purchase medicines from the private drug shops. UH&FPO, Jhikorgacha, Khulna
In order to supplement information concerning NCDs service readiness, we also collected data using NCD health facility observation checklist (table 1). The findings supplement the expression and concerns shared by participants. All NCD corners had availability of basic equipment; however, other essential equipment and supplies were not available. The shortages of laboratory facilities in all UHCs were reported. All UHCs had the MO and paramedics locally assigned. NCD drugs were unavailable in almost all UHCs, except few UHCs of Khulna division and one UHC of Dhaka division.
Table 1.
Service readiness (availability of basic infrastructure, equipment, diagnostic services, supplies and medication)
| Physical infrastructure | Khulna division | Dhaka division | Sylhet division | |||||||
| UHCs code ⇒ | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 |
| Basic infrastructure | ||||||||||
| Adequate lighting | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Water and sanitation facilities | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Space, cleanliness, ventilation | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Storage facility/refrigeration | × | × | × | × | × | × | × | × | × | × |
| Furniture (patient examination bed, chairs and table) | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Basic equipment and supplies | ||||||||||
| Weighting scale | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Measuring tape | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Height measure | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Stethoscope | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| BP measurement set | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| NCD patient register book | × | × | × | × | × | × | × | × | × | × |
| Clinical protocol for NCDs | × | × | × | × | × | × | × | × | × | × |
| NCDs-related IEC materials | × | × | × | × | × | × | × | × | × | × |
| Investigation and laboratory facilities | ||||||||||
| Glucometer set | × | × | × | × | × | × | × | × | × | × |
| ECG set | × | × | × | × | × | × | × | × | × | × |
| Urine protein test by strips | √* | √ | √ | √* | √ | √* | √ | √* | √* | √* |
| Urine ketone test by strips | √ | √* | √ | √ | √* | √ | √* | √* | √* | √ |
| Blood cholesterol assay | √ | × | √ | × | √ | × | × | × | × | √ |
| Lipid profile | √ | √ | √ | × | √ | × | √ | √ | × | √ |
| Serum creatinine assay | √ | × | √ | × | × | × | √* | × | × | × |
| Troponin test by strips | × | × | × | × | × | × | × | × | × | × |
| Urine test strips | √ | × | √ | × | √ | × | × | × | × | × |
| Fasting blood sugar test | √ | √* | √ | √* | √* | √* | √* | √* | √* | √* |
| Blood sugar 2 hours after meal | √ | √* | √ | × | √* | × | √* | × | √* | √* |
| HbA1c test | × | × | × | × | × | × | × | × | × | × |
| Human resources | ||||||||||
| Medical officer | √ | √ | √ | √ | √ | √ | √ | √ | √ | √ |
| Nurse | √ | √ | √ | √ | √ | √ | √ | √ | × | √ |
| Others support staff | √ | √ | √ | √ | √ | × | √ | × | √ | × |
| Availability of NCD drugs | ||||||||||
| Metformin | √ | √ | × | × | √ | × | × | × | × | × |
| Insulin | × | × | × | × | × | × | × | × | × | × |
| Glibenclamide | × | × | × | × | × | × | × | × | × | × |
| Amlodipine (Tab. Amdocal) | √ | √ | × | × | √ | × | × | × | × | × |
| Tab Nifedipine | × | × | × | × | × | × | × | × | × | × |
| Hydrochlorothiazide | × | √ | × | × | × | × | × | × | × | × |
| Propranolol | × | × | × | × | × | × | × | × | × | × |
| Atenolol | × | × | × | × | × | × | × | × | × | × |
| Furosemide | × | × | × | × | × | × | × | × | × | × |
| Spironolactone | × | × | × | × | × | × | × | × | × | × |
UHC codes=1: Chowgacha UHC; 2: Zhigorgacha UHC; 3: Kaligong UHC; 4: Devhata UHC; 5: Munshigong UHC; 6: Hazigong UHC; 7: Golapgong UHC; 8: Balagong UHC; 9: Fenchugong UHC; 10: Chatok UHC.
√ denotes availability of services; × denotes unavailability of services.
*Reagent/lab technician was not available during the period of data collection.
BP, Blood pressure; ECG, Electrocardiogram;; HbA1c, Hypoglycaeted heamoglobin; IEC, Information, education and communication; NCD, non-communicable disease; UHC, upazila health complex;.
NCDs’ screening, diagnosis, treatment, follow-up and referral
Participants reported that the services available in the NCD corners were limited to general consultation, health education and counselling. Patients with possible NCD problems were advised from the OPD registration booth to visit the NCD corners and to undergo necessary medical investigations when required. Those requiring further attention were referred to the specialists such as cardiologists, endocrinologists and pulmonologists. However, in most cases, these specialists were not available in the UHCs. One MO stated:
The patients generally receive basic NCD services including consultation, basic investigation, and treatment and advice from us. In case, the case is not manageable or too serious, we refer the patients to the district hospital where the specialists are available. UH&FPO Teknaf, Chittagong
Another MO told about the follow-up process:
We do not have formal system in place to follow-up the patients, but I always tell the patients for follow-up visit after a certain duration and also I suggest them to bring the old OPD card during the next visit. MO, Munshiganj, Dhaka
In contrast, another participant mentioned that:
Among the patients, who come for follow-up, the diabetes patients are very much aware and regular, but the hypertension patients sometimes miss their appointments for follow-up and also forget to bring their old OPD cards. RMO, Balaganj, Sylhet
Record keeping and reporting
During the field data collection, in each NCD corner, we physically inspected if they had a separate registry for NCD patients. We found that most of the NCD corners had no separate registry for record keeping. Only three NCD corners that had had a separate register available for NCD patients shared their concern regarding the duplicate recording and reporting. One participant stated:
We do have a separate register for record keeping and reporting for NCD cases. But the problem is the NCD cases are reported both in the regular register book and NCD corner register book, so there is always a risk for duplication in reporting. RMO, Chowgacha, Khulna
Challenges to strengthening the NCD services: at systems level
The main concern shared by all UH&FPOs was the lack of proper communication and coordination between respective UHCs and the NCDC unit at DG Health Services when establishing NCD corners and determining NCD services. The gap existed in terms of the availability and the use of standard operating procedure as well as basic logistic services and essentials, the functional modality of NCD corners, human resources management and monitoring and reporting systems. As one participant put it:
We did receive a letter from the NCDC unit of DG health services last year, suggesting us to establish an NCD corner, however no detailed guidelines, standard operating procedure, logistics and supplies were provided. RMO, Balaganj, Sylhet
There has not been any supervision and monitoring from the NCDC unit, nor we have communicated with them regarding the NCD corner and its’ service delivery mechanism. UH&FPO, Jhikorgacha, Khulna
We already have human resource crisis, there are not enough paramedics or doctors. Over that the rapid and frequent transfer of the trained NCD corner MO makes it even more challenging to keep the NCD corner fully functional. UH&FPO, Jhikorgacha Khulna
At service delivery level
The basic essential medicines that are available for NCDs at UHC were limited to the common NCDs condition such as, diabetes and hypertension. In most cases, the MOs were busy in providing OPD consultations thus, did not have adequate time for providing counselling and health education. At the same time, paramedics in the Outpatient door (OPD) either did not find enough time or had limited knowledge to provide proper counselling and health education for NCD prevention and management.
Participants also raised concern about the lack of regular laboratory facilities in the UHCs, which compelled patients to visit private laboratory. One UH&FPO stated:
… when the lab service is not available at UHC, we have no choice than sending them to the private lab, where the patients are compelled to pay high cost. Even patients sometime do not perform investigation as they can’t afford the cost. UH&FPO, Munshiganj Dhaka
Other challenges identified were patients’ poor awareness of their own NCD conditions and negligence in bringing previous visits’ prescriptions during the follow-up visits. All of these were the added challenges for the Medical Officer (MO) working in the NCD corner. One Resident Medical Officer (RMO) expressed:
People are not even aware that they need to bring their past prescriptions during the follow-up visit, that makes MO’s job even harder for proper investigation, diagnosis and quality care. RMO, Chowgacha, Khulna
Perceived solutions to addressing the NCD challenges
Participants in the qualitative interviews and a stakeholder meeting identified several challenges and suggested several possible measures to address them. Few majors of them are as below:
Communication and coordination: all participants recommended the needs for effective communication and coordination between respective UHCs and the NCDC unit of DGHS.
Infrastructure, logistics, equipment and medicine: participants identified the needs for adequate physical infrastructure, essential equipment such as glucometer, strips for random blood glucose test, ECG machine and batteries to operate the equipment. Furthermore, a need for regular supply of NCD medicines and having availability of the IEC and BCC materials was suggested.
Trained human resources: participants strongly recommended a need for a dedicated NCD corner team, which may comprise a trained MO, paramedics such as medical assistant, a nurse and a supporting staff.
Discussion
This study provided an overview on the current status of NCD corners and highlighted the challenges and opportunities to strengthen the NCD services provided through the NCD corners in Bangladesh. Given the increasing burden of NCDs in the country, there has been a greater need for developing a feasible mechanism that addresses the problems of NCDs, meets the service delivery needs and ensures the services are provided at the grassroot level with affordable cost. The initiative taken by the Bangladesh government to establish NCD corners in UHCs is vital to prevention and control of NCDs. The findings of this study describe the current challenges that NCD corners are facing, which should guide the policy makers to take measures in strengthening NCD services, delivered through NCD corners.
NCDs’ current scenario
The findings related to the common NCD problems such as CVD, diabetes and COPD corroborate existing literature. According to WHO, over two-third (67%) or estimated 550 000 people in Bangladesh die every year due to NCDs and related conditions including CVD, diabetes, COPD, cancer and mental health problems.28 Over the past 20 years, there has been a ninefold increase of deaths from the NCDs,29 and this is likely to increase if no appropriate actions are taken seriously.3 8 16
Service readiness
We identified the lack of service readiness to address the problem of NCDs at the primary care level. The shortages of trained healthcare providers align with the overall shortages of trained HRH in Bangladesh, particularly in rural areas.30–32 These shortages of trained human resources do not meet the WHO recommended ratio or healthcare providers (1:3:5) for providing basic healthcare at the primary care level.33 The trained healthcare providers play a vital role in the efforts of prevention and control of NCDs.32 A recently conducted multicountry study in selected countries of Asia and Pacific reported that the community health workers (CHWs) play a key role in the delivery of health services, and capitalising on their experiences could deliver more NCD-related services. Furthermore, the study emphasised a need for building the capacity of CHWs to deliver quality NCD-related services.32 Studies in sub-Saharan Africa have reported that poor knowledge and experience of front-line health workers were major barriers to care and services for NCDs.34 35
Alternatively, studies in selected countries of Africa36 37 and Asia38 39 have established proper training and supervision of non-medical doctor clinicians or nurse-led clinics could provide effective primary care for NCDs. However, in the context of Bangladesh, such provisions of task shifting for NCDs services for non-medical health workforce is still unavailable.39 Studies reported lack of different aspects of care at UHC,6 7 40 which range from basic equipment to logistics, supplies, diagnostic services, medicines and specialised care, recording, reporting and referral. Study also identified lack of/poor quality of medicines as cause of patient dissatisfaction in government health facilities in Bangladesh. A study in India reported discordance in availability of recommended class of drug for CVDs at primary healthcare levels.41
NCD services
The findings of this study show that the NCD corners currently lack the facilities and equipment essential for NCDs screening and early diagnosis. NCDs’ early screening and diagnosis are crucial to the NCDs prevention and control efforts, particularly in countries like Bangladesh, where the cost of treatment and medication are so expensive that most of the people could not afford these services. These findings corroborate to the findings of a study conducted in a low-resource neighbouring country, Nepal.42 Mishra et al reported that lack of infrastructure, basic supplies, equipment and mechanism are major issues to combat issues of NCDs at primary healthcare levels in Nepal. People with NCDs often travel to the secondary or tertiary level hospitals, generally located in urban areas and using the NCD services from these urban hospitals is often geographically inaccessible with high cost.
Challenges to NCD service strengthening
The findings of this study also highlighted some key challenges that exist at systems and service delivery levels. Other studies in Bangladesh suggested that the health systems of Bangladesh are not yet well prepared to combat problem of NCDs.7 20 43 For example, Roman et al., 43 using a scorecard for tracking actions to NCDs, reported low performance scores in three out of four domains of score card including risk factor surveillance, research and health system response, and the governance component received moderate performance scores. Similarly, Bangladesh Health Watch Report 2016 documented that government’s role has been very limited to providing NCDs and related services to combat the growing burden of NCDs in Bangladesh.7 17 However, developing a functional team and a service delivery system in resource poor setting is possible and has been highlighted by several studies but needs to be translated into action.32 44
Limitations
One of the key limitations of this study was that we were unable to include beyond four administrative divisions. Having additional subdistricts included in this study could have added additional insights to make the findings more generalisable. However, we believe that our findings are generalisable considering that the results are consistent with other studies in Bangladesh. Furthermore, we were unable to collect data from the patients, which could have added insights from the service recipients’ perspective but was out of the scope of this study.
Conclusion
The findings provide current insights about the situation and the challenges faced by NCD corners located in different UHCs across four divisions in Bangladesh. The findings suggest that the NCD corners remain poorly functioning with many challenges at systems and service delivery levels. These include: (A) lack of trained human resources, (B) inadequate equipment and laboratory facilities, (C) inadequate logistics and drug supplies, (D) lack of proper recording and reporting, (E) coordination/communication between NCD corners and NCDC unit of DGHS and (F) lack of proper guidelines and standard operating procedure.
Although the NCD corners are still at a nascent stage, there are needs to improve capacity of NCD corners to screen for NCDs and facilitate the subsequent investigation, treatment, referral, recording and reporting and follow-up. These will require upgrading of physical infrastructure, ensure supply of basic equipment and logistics, availability of trained human resources team for NCD corner and ensure proper communication and coordination between NCD control unit of DGHS and respective UHCs, along with expert advice for long-term systems strengthening. All these findings need to be taken into consideration prior to expanding these NCD corners to other UHCs.
Supplementary Material
Footnotes
Contributors: LBR, KK, TB, MIT and SMA contributed in conceptualising the study, drafting the manuscript and finalisation. LBR, TB and MIT contributed in data analyses and results write up. PP, ASA, AMNR, SMSI, KK and SMA thoroughly reviewed the manuscript and contributed substantially for necessary revision. LBR, KK, TB, ASA, AMNR and SMA final reviewed the manuscript and prepared for submission.
Funding: This study received seed funding support from the Centre of Excellence for Universal Health Coverage (CoE-UHC), BRAC University, Bangladesh.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: The ethics approval of this study was obtained from the Ethics Review Committee of International Centre for Diarrhoeal Disease Research, Bangladesh (Protocol approval no. PR-16068).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: All data relevant to the study are included in the article. Any additional data to this study can be available from the corresponding author (LR) up on reasonable request.
References
- 1. Department of Economic and Social Affairs Population Division United Nations World Population Ageing 2015 - Highlights. New York: United Nations, 2015. [Google Scholar]
- 2. Bangladesh Bureau of Statistics Population & Housing Census Report 2011. Bangladesh. Dhaka: Statistics Division Bangladesh Bureau of Statistics, 2012. [Google Scholar]
- 3. World Health Organization Global status report on noncommunicable diseases. Geneva: World Health Organization, 2014. [Google Scholar]
- 4. Low W-Y, Lee Y-K, Samy AL. Non-Communicable diseases in the Asia-Pacific region: prevalence, risk factors and community-based prevention. Int J Occup Med Environ Health 2015;28:20–6. 10.2478/s13382-014-0326-0 [DOI] [PubMed] [Google Scholar]
- 5. The World Bank Cause of death, by non-communicable diseases (% of total) New York the world bank, 2016. Available: https://data.worldbank.org/indicator/SH.DTH.NCOM.ZS?end=2015&locations=BD&start=2000&view=chart [Accessed 07 Nov 2017].
- 6. Alam D, Robinson H, Kanungo A, et al. Health systems preparedness for responding to the growing burden of non-communicable disease-a case study of Bangladesh. Health Policy & Health Finance knowledge Hub The Nossal Institute for Global Health The University of Melbourne 2013:1–25. [Google Scholar]
- 7. Zaman MM, Nieveras O, Talukder HK, et al. Current health system scenario for addressing non-communicable diseases in Bangladesh: Bangladesh health Watch report, 2016. non-communicable diseases in Bangladesh current scenario and future directions. Dhaka: James P Grant School of Public Health BRAC University, 2016: 43–55. [Google Scholar]
- 8. Biswas T, Islam MS, Linton N, et al. Socio-Economic inequality of chronic non-communicable diseases in Bangladesh. PLoS One 2016;11:e0167140 10.1371/journal.pone.0167140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Beaglehole R, Bonita R, Alleyne G, et al. Un high-level meeting on non-communicable diseases: addressing four questions. The Lancet 2011;378:449–55. 10.1016/S0140-6736(11)60879-9 [DOI] [PubMed] [Google Scholar]
- 10. Rawal LB, Kanda K, Mahumud RA, et al. Prevalence of underweight, overweight and obesity and their associated risk factors in Nepalese adults: data from a nationwide survey, 2016. PLoS One 2018;13:e0205912 10.1371/journal.pone.0205912 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Biswas T, Islam A, Islam MS, et al. Overweight and obesity among children and adolescents in Bangladesh: a systematic review and meta-analysis. Public Health 2017;142:94–101. 10.1016/j.puhe.2016.10.010 [DOI] [PubMed] [Google Scholar]
- 12. Sarker M, Hossain MD, Rawal LB, et al. Epidemiology of non-communicable diseases in Bangladesh: Bangladesh Health Watch Report 2016 : Ahmed SM, Non-Communicable diseases in Bangladesh current scenario and future directions. Dhaka: James P Grant School of Public Health BRAC University, 2016: 07–18. [Google Scholar]
- 13. Rawal LB, Biswas T, Khandker NN, et al. Non-Communicable disease (Ncd) risk factors and diabetes among adults living in slum areas of Dhaka, Bangladesh. PLoS One 2017;12:e0184967 10.1371/journal.pone.0184967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Khalequzzaman M, Chiang C, Choudhury SR, et al. Prevalence of non-communicable disease risk factors among poor shantytown residents in Dhaka, Bangladesh: a community-based cross-sectional survey. BMJ Open 2017;7:e014710 10.1136/bmjopen-2016-014710 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Khandker NN, Biswas T, Khan ANS, et al. Socio-Demographic characteristics and tobacco use among the adults in urban slums of Dhaka, Bangladesh. Tob Induc Dis 2017;15:26 10.1186/s12971-017-0131-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Biswas T, Garnett SP, Pervin S, et al. The prevalence of underweight, overweight and obesity in Bangladeshi adults: data from a national survey. PLoS One 2017;12:e0177395 10.1371/journal.pone.0177395 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bangladesh Health Watch Bangladesh health Watch report 2016: non-communicable diseases in Bangladesh current scenario and future directions. Dhaka Bangladesh: James P Grant School of Public Health BRAC University, 2016. [Google Scholar]
- 18. Directorate General of Health Services Ministry of Health and Family Welfare Health Bulletin, 2017. Dhaka, Bangladesh: Management Information System, Directorate General of Health Services, 2018. [Google Scholar]
- 19. Biswas T, Pervin S, Tanim MIA, et al. Bangladesh policy on prevention and control of non-communicable diseases: a policy analysis. BMC Public Health 2017;17:582 10.1186/s12889-017-4494-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Zaman MM, Ullah A, Bhuiyan MR, et al. Noncommunicable disease prevention and control situation in a primary health care setting of Bangladesh: design and baseline findings of an intervention. Chronic Diseases International 2016;3. [Google Scholar]
- 21. Charmaz K. Grounded Theory : Lewis-Beck MS, Bryman A, Liao TF, The SAGE encyclopedia of social science research methods. Thousand Oaks, California: Sage Publications, Inc, 2011: 441–4. [Google Scholar]
- 22. Chun Tie Y, Birks M, Francis K. Grounded theory research: a design framework for novice researchers. SAGE Open Med 2019;7:205031211882292–27. 10.1177/2050312118822927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. National Institute of Population Research and Training (NIPORT), Associates for Community Population Research (ACPR), ICF International Bangladesh health facility survey, 2014. Dhaka, Bangladesh: NIPORT, ACPR, and ICF International, 2016. [Google Scholar]
- 24. Nowell LS, Norris JM, White DE, et al. Thematic analysis:Striving to meet the trustworthiness criteria. Int J Qual 2017;16. [Google Scholar]
- 25. O’Brien BC, Harris IB, Beckman TJ, et al. Standards for reporting qualitative research: a synthesis of recommendations 2014;89:1245–51. [DOI] [PubMed] [Google Scholar]
- 26. Shenton AK. Strategies for ensuring trustworthiness in qualitative research projects. Education for Information 2004;22:63–75. 10.3233/EFI-2004-22201 [DOI] [Google Scholar]
- 27. Houghton C, Casey D, Shaw D, et al. Rigour in qualitative case-study research. Nurse Res 2013;20:12–17. 10.7748/nr2013.03.20.4.12.e326 [DOI] [PubMed] [Google Scholar]
- 28. World Health Organization Noncommunicable diseases progress monitor 2017. Geneva: World Health Organization, 2017. [Google Scholar]
- 29. Islam SMS, Purnat TD, Phuong NTA, et al. Non‐Communicable diseases (NCDS) in developing countries: a symposium report. Global Health 2014;10:1 10.1186/s12992-014-0081-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Rawal LB, Joarder T, Islam SMS, et al. Developing effective policy strategies to retain health workers in rural Bangladesh: a policy analysis. Hum Resour Health 2015;13:36 10.1186/s12960-015-0030-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Ahmed SM, Hossain MA, RajaChowdhury AM, et al. The health workforce crisis in Bangladesh: shortage, inappropriate skill-mix and inequitable distribution. Hum Resour Health 2011;9:3 10.1186/1478-4491-9-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Abdullah AS, Rawal LB, Choudhury SR, et al. Use of community health workers to manage and prevent noncommunicable diseases: policy options based on the findings of the coach study. Delhi: World Health Organization, 2019. [Google Scholar]
- 33. Ahmed SM AB, Anwar I, Begum T, et al. Bangladesh health system review, 2015. [Google Scholar]
- 34. Mendis S, Abegunde D, Oladapo O, et al. Barriers to management of cardiovascular risk in a low-resource setting using hypertension as an entry point. J Hypertens 2004;22:59–64. 10.1097/00004872-200401000-00013 [DOI] [PubMed] [Google Scholar]
- 35. Sengwana MJ, Puoane T. Knowledge, beliefs and attitudes of community health workers about hypertension in the Cape Peninsula, South Africa. Curationis 2004;27:65–71. 10.4102/curationis.v27i1.958 [DOI] [PubMed] [Google Scholar]
- 36. Mamo Y, Seid E, Adams S, et al. A primary healthcare approach to the management of chronic disease in Ethiopia: an example for other countries. Clin Med 2007;7:228–31. 10.7861/clinmedicine.7-3-228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Kengne AP, Awah PK, Fezeu LL, et al. Primary health care for hypertension by nurses in rural and urban sub-Saharan Africa. J Clin Hypertens 2009;11:564–72. 10.1111/j.1751-7176.2009.00165.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Neupane D, Kallestrup P, McLachlan CS, et al. Community health workers for non-communicable diseases. Lancet Glob Health 2014;2 10.1016/S2214-109X(14)70303-1 [DOI] [PubMed] [Google Scholar]
- 39. Rawal LB, Mahmud K, Islam SMS, et al. Training mid-level health cadres to improve health service delivery in rural Bangladesh. Prim Health Care Res Dev 2016;17:503–13. 10.1017/S1463423616000104 [DOI] [PubMed] [Google Scholar]
- 40. Zaman M, Ullah A, Bhuiyan M, et al. Moniruzzaman and Rahman SMA noncommunicable disease prevention and control situation in a primary health care setting of Bangladesh: design and baseline findings of an intervention. Chronic Dis Int 2016;3. [Google Scholar]
- 41. Pakhare A, Kumar S, Goyal S, et al. Assessment of primary care facilities for cardiovascular disease preparedness in Madhya Pradesh, India. BMC Health Serv Res 2015;15:408 10.1186/s12913-015-1075-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Mishra SR, Kallestrup P, Neupane D. Country in focus: confronting the challenge of NCDS in Nepal. Lancet Diabetes Endocrinol 2016;4:979–80. 10.1016/S2213-8587(16)30331-X [DOI] [PubMed] [Google Scholar]
- 43. Roman AV, Perez W, Smith R. A scorecard for tracking actions to reduce the burden of non-communicable diseases. The Lancet 2015;386:1131–2. 10.1016/S0140-6736(15)00197-X [DOI] [PubMed] [Google Scholar]
- 44. Rawal LB, Tapp RJ, Williams ED, et al. Prevention of type 2 diabetes and its complications in developing countries: a review. Int J Behav Med 2012;19:121–33. 10.1007/s12529-011-9162-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2019-029562supp001.pdf (103.9KB, pdf)


