Abstract
Introduction
This systematic review aims to determine if combination HIV prevention programmes include outcome measures for empowerment, inclusion and agency to demand equal rights and measure the relationship between empowerment and HIV prevention outcomes.
Methods
An electronic literature search of PubMed, POPLINE, Index Medicus and Google Scholar was conducted between August and October 2018. We included studies that evaluated combination prevention programmes that had all three types of intervention components and that specifically serve members of populations disproportionately affected by HIV published from 2008 to 2018. The selected studies were screened for inclusion, and relevant data abstracted, assessed for bias and synthesised.
Results
This review included a total of 15 studies. Findings indicate that combination HIV prevention programmes for marginalised populations have delivered a variety of theory-based behavioural and structural interventions that support improvements in empowerment, inclusion and agency. However, empowerment, inclusion and least of all agency are not measured consistently or in a standardised way. In addition, analysis of their relationships with HIV prevention outcomes is rare. Out of our 15 included studies, only two measured a relationship between an empowerment, inclusion or agency outcome and an HIV prevention outcome.
Conclusion
These findings suggest that policy-makers, programme planners and researchers might need to consider the intermediate steps on the pathway to increased condom use and HIV testing so as to explain the ‘how’ of their achievements and inform future investments in HIV prevention. This will support replication and expansion of programmes and ensure sustainability of the programmes.
PROSPERO registration number
CRD42018106909
Keywords: HIV, human rights, intervention, key and marginalised populations, prevention, low-and middle-income countries
Key questions.
What is already known?
Combination HIV prevention programmes have demonstrated improved effects on HIV prevention outcomes for marginalised populations.
However, intermediate outcomes of these programs are not always measured in the evaluations.
What are the new findings?
Findings of this review indicate that combination HIV prevention programmes for marginalised populations have delivered a variety of theory-based behavioural and structural interventions that support improvements in empowerment, inclusion and agency.
Empowerment, inclusion and least of all agency are not measured consistently or in a standardised way; and the analysis of their relationships with HIV prevention outcomes is rare.
What do the new findings imply?
Policy-makers, programme planners and researchers need to consider the intermediate steps on the pathway to increased condom use and HIV testing so as to explain the ‘how’ of their achievements and inform future investments in HIV prevention.
Introduction
Understanding the role of empowerment, inclusion and agency in health has been a growing area of interest globally over the past decade.1 For example, the evidence supports association between women’s agency and contraceptive use or women’s empowerment and maternal and child health outcomes.1–3 As a result, women’s empowerment was included as one of the 17 Sustainable Development Goals (SDGs), and is acknowledged to be integral to achieving all of the SDGs.4 As more evidence suggests the links between empowerment and health, global health programming is responded by moving away from strictly biomedical models and towards comprehensive approaches that include components, which aim to affect empowerment, inclusion and agency.5–7 But because measuring these changes is lagging behind innovative programming,1 5 we may be continuing to invest in programmes without knowing how they actually work.
This shift in approaches can clearly be seen in HIV prevention programming in low-income and middle-income countries. HIV prevention programming has shifted from vertical single-focused interventions such as voluntary confidential counselling and testing (VCCT) to combination prevention programmes. Combination prevention programmes are HIV prevention programmes that rely on the evidence-informed, strategic, simultaneous use of biomedical, behavioural and structural prevention strategies.8 An example of a combination HIV prevention programme would be a VCCT programme for female sex workers (FSWs) that has peer-based outreach, childcare and microcredit along with policy or legal reforms to create more enabling environments for accessing healthcare.9
Combination prevention programme should be, by design, ‘rights-based, evidence-informed and community-owned programme’.8 Combination prevention programmes primarily aim to serve marginalised populations, which we define as those populations that are at higher risk of HIV as well as particularly vulnerable to social, political and legal discrimination and exclusion. While these programmes can serve all populations, they are often focused on key populations such as FSWs, men who have sex with men (MSM), transgender people (TG), people who inject drugs (PWIDs), adolescent girls and young women, pregnant and postpartum HIV-infected mothers and their babies, and people in prisons and other closed settings. They are increasingly considered the standard of care.10 Combination prevention programmes, as compared with vertical approaches, have demonstrated improved effects on HIV prevention outcomes for the marginalised populations.11 12
Combination prevention programmes aim to improve HIV prevention by affecting empowerment, inclusion and agency of participants. However, these important intermediate outcomes are not always measured in the evaluations of combination prevention programmes, which limit our understanding of how and why they work.6 10 One reason may be that it can be more challenging to measure empowerment, for example, than to measure traditional HIV prevention outcome such as HIV incidence, protected intercourse and recent HIV testing.11 13–19 Besides, there are no widely accepted or standardised methods to measure broad concepts such as improved agency to demand human rights and increased experiences of inclusion despite being core components of a programme’s overall strategy.18 19 Without measurements, we cannot determine the relationships between these concepts and HIV prevention outcomes or HIV service access.
Our review looks to identify the variety of measures that are being used to capture empowerment, inclusion and agency for combination HIV prevention programmes to determine to what extent existing studies measure the relationship between these broad outcomes and HIV outcomes. We also want to determine if there is sufficient evidence to support that improved agency to demand rights leads to improved combination HIV prevention service access.
This review fills an important gap in the literature. Past systematic reviews have summarised the effectiveness of specific types of HIV prevention interventions. Examples include reviews of programmes that reduce stigma,20 that synthesise factors associated with programme success such as adherence,21 and that catalogue common measures for indicators such as stigma,22 condom use23 or HIV clinical care.24 Two other reviews have looked at the effectiveness of community empowerment programmes on HIV prevention with marginalised populations.6 25 To date, there have been no published reviews that examine the role of individuals’ empowerment, inclusion and agency in the effectiveness of combination HIV prevention programmes.
Theory of change underlying the review
Over the past decade, the HIV prevention community has focused on developing evidence-based, community-led, person-centred and human rights-based programming with the assumption that such programming will result in reduced self-stigma, established advocacy agendas, enhanced capacity to capture evidence and engaged stakeholders.26 The assumption is that individuals from marginalised populations will be respectfully included in society, have the agency to advocate for their rights and feel empowered to demand high-quality, respectful health services. Increased empowerment, inclusion and agency for marginalised populations will result in improved access to health services, more comprehensive coverage, enabling environments and more sustainable community-based services.27 In theory, these results will lead to long-term outcomes that members of marginalised populations are healthier and enjoy equal and full rights to HIV prevention services, which will all lead to the ultimate goal of preventing HIV and ending AIDS among the marginalised populations.
Practical rationale for the review
Results of this review can potentially help inform policy and academic debates and discussion, programme interventions and planning as well as the development of more suitable measures of key outcomes by providing a comprehensive synthesis on current measures used to assess combination HIV prevention programming. Future programme evaluators will be able to identify specific measures beyond traditional HIV outcomes that they can include in their results frameworks and study designs. When researchers begin to use standard measures for new areas of evaluation, we can begin to compare outcomes between studies and over time, as well as determine whether combination prevention programmes result in empowerment, inclusion and agency—in what context, for whom and as a result of which types of programme features.
Understanding the mechanisms through which interventions operate is critical for planning programmes and evaluations. This review will provide a basis for decision-making and priority-setting for policy-makers and donors including how they support the role of the non-governmental organisations (NGOs) and civil society organisations, including the affected communities, more broadly, in low-income and middle-income countries in their role as HIV advocates. It may also provide important evidence for community organisations working with marginalised populations and implementing combination HIV prevention programmes.
Objectives of the review
The primary objective of this review is to answer the following three research questions: (1) does the current body of evidence from evaluations of combination HIV prevention programming for marginalised populations in low-income and middle income countries include outcome measures for empowerment, inclusion and agency to demand equal rights?; (2) to what extent do these evaluations measure the relationship between empowerment outcomes (including inclusion and agency to demand rights) and HIV prevention outcomes? and (3) is there sufficient evidence to support that improved agency to demand rights leads to improved combination HIV prevention outcomes? A secondary objective of this review is to provide recommendations for future research that aims to measure the impact of HIV programming for HIV marginalised populations on empowerment, inclusion and agency to demand equal rights in low-income and middle-income countries.
Methods
Reporting and protocol registration
This review follows Preferred Reporting Items for Systematic Reviews and Meta-Analyses guidelines (see online supplementary file 1). A protocol for this review has been registered with PROSPERO International Prospective Register of Systematic Reviews and is available at: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=106909
bmjgh-2019-001560supp001.pdf (208.5KB, pdf)
Eligibility criteria
Inclusion criteria
Participants
We included studies that evaluate programmes specifically serving members of populations disproportionately affected by HIV, which include FSWs, MSM, TG people, PWID, adolescent girls and young women (ages 10–24), and people in prisons and other closed settings. We also included studies on prevention of mother-to-child transmission.
Types of HIV programming
We included studies that evaluate combination prevention HIV programmes, which are programmes that include biomedical, behavioural and structural interventions as defined by United Nations Programme on HIV/AIDS (UNAIDS).8 Programmes must have included a component of all three types if interventions to be considered combination programmes, as recommended by UNAIDS (2010).
Study types
We included all observational, quasi-experimental and experimental evaluations as long as there is a documented and predetermined methodology guiding the evaluation. To be included, the quantitative studies needed to collect data at baseline and endline (longitudinal) and/or cross-sectional (endline) data from treatment and comparison groups. Qualitative studies must have had reported data from the perspectives of participants in the programmes using methodologies such as in-depth interviews, participant observation and focus group discussions that draw on phenomenological analyses, grounded theory, ethnography, narrative research and/or pragmatic inquiry. We also included detailed protocols or baseline reports from studies that have not released final evaluation data in order to capture the most recent data on what outcomes are being measured in ongoing programmes.
Outcomes
We included studies that had all types of outcomes including all traditional HIV prevention outcomes (eg, condom use, number of sexual partners and recent HIV testing) as well as any outcomes on empowerment (eg, self-efficacy or agency, feelings of autonomy, sense of self-worth, self-confidence, self-esteem and income generation), inclusion (eg, experiences of stigma or discrimination, freedom from violence, negotiations and discussion around sex and inclusivity of local policy) and agency to demand equal rights (eg, awareness of rights or laws and political participation such as voting).
Time period
We examined studies and research protocols published in the last 10 years (2008–2018). This covers the period of time starting with when the UNAIDS Prevention Reference Group agreed on the definition of combination prevention programmes and called for a scale-up of these types of programmes until the current day (UNAIDS 2010).
Exclusion criteria
Participants
We excluded evaluations of programmes that service the general population or vulnerable people such as the general population of adolescents or general migrants unless they are also members of one of the marginalised population groups listed above.
Types of HIV programming
We excluded studies that evaluated programmes that provided less than three types of intervention components even if they reported themselves as combination programmes.
Study types: We excluded qualitative studies that did not employ the defined methodologies listed above or that do not draw from direct observation or direct reports from programme participants. We also excluded any studies that employed mathematical modelling.
Outcomes
We did not exclude any studies based on types of outcomes in order to include the full range of outcomes. All types of biomedical, behavioural and structural outcomes can be included in the review.
Time period
We excluded studies that were published inside of our time period but were reporting on data collected earlier than 2008.
Information sources
The literature search occurred in three phases:
Phase 1: database searches
The first phase involved searching the following three main databases:
PubMed (http://www.pubmed.gov).
POPLINE (http://www.popline.org/).
Index Medicus for WHO (http://www.globalhealthlibrary.net).
Phase 2: keyword searches
The second phase consisted of reviewing reference lists of included studies and searching through studies that have cited the included studies for additional resources and conducting supplemental keyword searches using identified program names and locations.
We also conducted a supplemental keyword search in google.com based on leads generated by the search described above. For example, if a search identified an article mentioning (but not evaluating) an HIV programme for key and vulnerable populations through an NGO called the Stepping Stones Programme, which reported an increase in women’s sense of power as a result of an HIV programme, a search of google.com and google.scholar would use a search of ‘The Stepping Stones Programme’ and several related keywords to determine whether there was additional information on the programme that may include evaluation information relevant to the analyses.
Phase 3: grey literature searches
We searched the grey literature for dissertations, theses, government reports, NGO reports and funder reports using Google/Google Scholar and limiting to the first 10 pages, which is 100 hits ordered by relevance. A search diary was maintained describing the databases searched, the date of the search, the keywords used, the number of studies in initial search results, the number of ‘hits’ and the number of duplicates.
Search
A search strategy described below was used to search all databases and was adjusted to fit the diversity of search options available for each database. We included general keywords around ‘Combination HIV Prevention Programming’ and ‘Marginalised, Key and Vulnerable Populations’ in our search strategy.
Keywords group #1: population
“key populations”, “marginalised populations”, “marginalized populations”, “iv drug users”, “injecting drug users’’, “people who inject drugs”, “men who have sex with men”, “msm”, “homosexual*”, “transgender*”, “transsexual*”, “transvestite”, “sex work*”, “female sex workers”, “female entertainment workers”, “prostitute*”, “prostitution”, “vulnerable women”, “prisoners”, “incarcerated”, “inmate”.
Keyword group #2: programming
“combination”, “multilevel”, + “HIV*”, “AIDS*”, “HIV/AIDS*” + “service*”, “programme*”, “prevention”, “care”, “intervention”, “evaluation”, “implementation science”, “implementation research”.
Keyword group #3: location
All low-income and middle-income countries as defined by the World Bank.
See the search strategy (online supplementary file 2) for additional information.
bmjgh-2019-001560supp002.pdf (207.2KB, pdf)
Selection of studies
In step 1, two team members independently read titles of search hits and excluded all references that were obviously irrelevant. Duplicate references were also excluded. Disagreements about inclusion were resolved through discussion via email. In step 2, two team members applied the specified inclusion/exclusion criteria outlined above to the remaining abstracts and determined whether the study should be included for analyses. In the case of a discrepancy between the two reviewers’ assessments, the case was discussed via email with a third team member for a decision.
Data collection process
A data extraction form was developed during the protocol stage. It was then turned into an online form, piloted and refined once the included studies were identified. Two team members read the full text of all included studies and extracted information from each study using an online data extraction form (Google Forms, see online supplementary file 3), which populated a result table. Disagreements in coding were resolved through email discussion.
bmjgh-2019-001560supp003.pdf (163.4KB, pdf)
Data items
Data items extracted included: authors, publication date, funder, name of programme, location of programme, region of programme, target populations, type of marginalised population, study design, sample size, type of sampling, types of intervention components, description of intervention, whether empowerment, inclusion and agency were measured, association/relationships measured, brief description of results, direction of effects and if effect was statistically significant.
We categorised intervention components into three groups using the following definitions: (1) biomedical strategies are those that reduce exposure, transmission and/or infection such as condom provision, male circumcision, sexually transmitted infection (STIs) services, postexposure prophylaxis and pre-exposure prophylaxis (PrEP); (2) behavioural strategies are those that promote risk reduction such as HIV testing and counselling, behavioural change communication to promote risk reduction, HIV education, social marketing and cash incentives; and (3) structural strategies are those that address the social, cultural, political, legal, economic and physical environmental context of HIV risk such as stigma reduction programmes, advocacy and coalition building, human rights programming, stigma and discrimination training or sensitisation workshops for police, housing policy and infrastructure development.8
We categorised outcome variables into the following four outcome groups based on well-established definitions in the literature:
Traditional HIV prevention outcomes: knowledge, attitude, behavioural and biological measures that were commonly measured in non-combination HIV prevention programme evaluations including, but not limited to, condom use, number of sexual partners and recent HIV testing and treatment.8
Empowerment: We grounded our categorisation in a widely cited definition of empowerment first described by Kabeer (p. 437)28 as ‘the expansion in people’s ability to make strategic life choices in a context where this ability was previously denied to them.’ In the included studies, we looked for a variety of measures including self-efficacy; sense of self-worth; self-confidence; critical thinking on such issues as gender, violence and social norms; disclosure of sexual orientation and reporting of violence and education level.29
Social inclusion: We used a broad definition of social inclusion supported by the World Bank (p. 3, 4),30 which states that ‘social inclusion is the process of improving the terms on which individuals and groups take part in society—improving the ability, opportunity and dignity of those disadvantaged on the basis of their identity.’ In the included studies, we looked for measures such as experiences of stigma or discrimination, perception of having social support, increased social networks and social cohesion, inclusion in the workforce, political processes and national HIV response.
Agency: We used a definition of agency from Markham that defined agency as ‘the ability to have a voice in society and influence policy’.31 We looked for measures of agency in the included studies including the ability to have a voice in society, the ability to demand equal rights, awareness of rights or laws, community-level action, political or civic participation and acceptance by local officials.
Risk of bias in individual studies
The study team assessed quantitative study rigour using the ROBINS-risk of bias tool for non-randomised studies of interventions and the Cochrane Risk of Bias Tool for the included randomised studies and presented the assessment for each individual study in a table.32 33
Synthesis of results
In response to our first research question, we performed a synthesis of all outcomes for marginalised populations reported in the included studies. Two researchers reviewed the extracted data and assigned a category to each extracted outcome measure. In response to our second and third research questions, a separate analysis was performed using all those studies that examine relationships between traditional HIV outcomes and any empowerment, inclusion or agency outcomes. For all studies, we reported whether a relationship was measured and if so, the direction of the effect. Due to the heterogeneity of interventions and outcomes reported in the included studies and after reviewing relevant literature on decision-making around pooling effects,34 35 we decided that our review was too broad to make use of a meta-analysis.
Deviations from protocol
This report deviated from the research protocol on a number of counts. First, we added the term ‘multilevel’ and ‘marginalised population’ to the search terms after the initial literature search to broaden the scope of our search. Second, we excluded mathematical modelling studies during screening because the primary goal of modelling studies was to be predictive of results to influence programme planning and were based on historical HIV prevention data. Therefore, these studies did not yield insights into current data collected from real individuals experiencing empowerment, inclusion and agency changes. Third, we decided to include study protocols and baseline studies to reflect the latest or upcoming measurement trends despite not having results. Finally, we were not able to conduct a synthesis of effect sizes or a meta-analysis, given the heterogeneity of the interventions and outcomes and the limited data on our outcomes of interest.
Patient and public involvement statement
No patient data were considered in this study.
Results
Study selection
The search was conducted between August and October 2018. We included a total of 15 studies and protocols. Figure 1 details the flow diagram of the filtering process used to identify the final included studies. Initially, we reviewed 1048 abstracts from the electronic database searches and 30 abstracts from keywords searches after excluding 19 duplicates. Of these, we excluded 922 irrelevant studies. We retrieved and reviewed 154 full-text studies using the predetermined criteria for inclusion.
Figure 1.
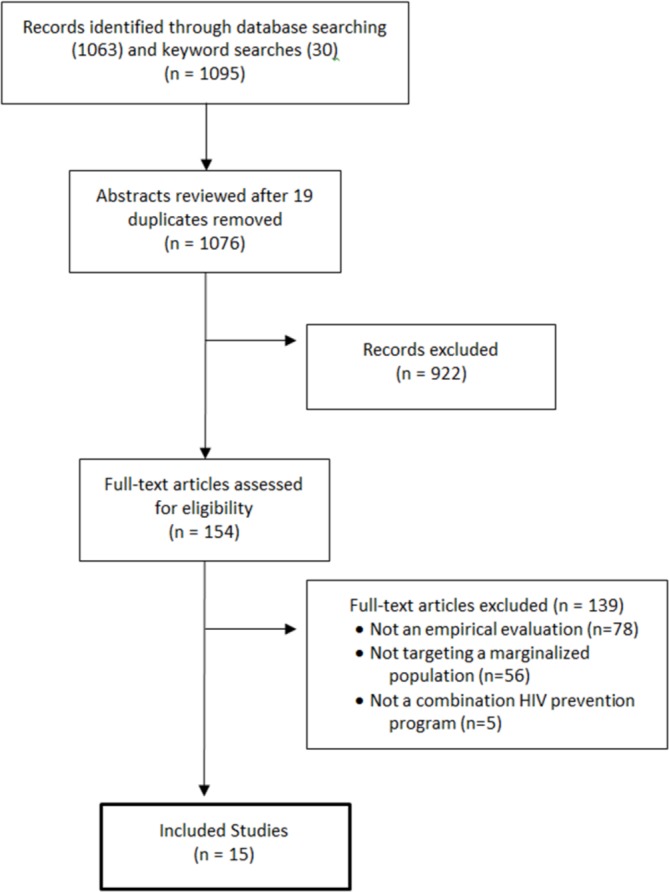
Search results of studies in the systematic review.
Based on the full-text review of the 154 studies, we excluded 139 studies when applying the criteria. There was 85% agreement between the reviewers. The following were the main reasons for exclusion: (1) the paper did not meet our criteria of an empirical evaluation (n=78); (2) the intervention was not targeting a marginalised population in a low-income or middle-income country (n=56) and (3) the study did not evaluate a combination HIV prevention programme (n=5). The remaining 15 full-text studies were included and used as the basis of the analysis that follows. Included studies were identified through PubMed (n=7), POPLINE (n=4) and Keyword searches (n=4). All were peer-reviewed journal articles except one unpublished report.36
There were no qualitative studies included in the final review. Of the 154 full texts we reviewed, 19 were qualitative studies. They were excluded because they were not evaluation studies (n=9), not focused on a key population (n=8), and not writing about a combination prevention programme by our definition or focusing on HIV (n=2).
Study characteristics
Geographical distribution
Table 1 summarises data on the publication date, programme name, location, region, target population, study design and sample size of each study included in this systematic review. The 15 included studies ranged in publication dates from 2009 to 2018 with over half published in the last 3 years. From the 15 studies, there were programmes that were active in 23 countries. There were six studies evaluating seven programmes in Africa (two in South Africa, one in Zimbabwe, one in Tanzania, one in Malawi, one in Kenya and one in Zimbabwe). There were six studies evaluating six programmes in Asia (one in Vietnam, three in India, one in the Philippines and one in Kazakhstan). There were three studies evaluating seven programmes in Central America (two in Mexico and one in Guatemala, El Salvador, Nicaragua, Costa Rica and Panama).
Table 1.
Description of 15 studies included in the systematic review in alphabetical order
| Authors | Year of publication | Name of Programme | Location | Region | Target population | Study design | Sample size |
| Arantxa Colchero et al41 | 2016 | MSM-targeted Combination Prevention Programme Initiative | Mexico | Central America | MSM | Quasi-experimental | 24 (cities) |
| Beattie et al37 | 2016 | Samvedana Plus | India | Asia | FSW | Cluster randomised controlled trial | 800 |
| Buttolph et al47 | 2017 | MP3 Youth Study | Kenya | Africa | FSW | Mixed-methods, cross-sectional, longitudinal cohort pilot study | 1000 |
| Chiao et al42 | 2009 | Multilevel Social Action-based Theory Intervention | Philippines | Asia | Pregnant and postpartum women | Randomised quasi-experimental, pre/post | 980 |
| Cowan et al38 | 2017 | Sisters Antiretroviral Prevention Programme—an Integrated Response | Zimbabwe | Africa | PWID | Cluster randomised control trial | 2883 |
| Fatti et al48 | 2017 | Community-based Combination HIV Prevention Intervention | South Africa | Africa | Pregnant and postpartum women | Cohort study | 1356 |
| Firestone et al19 | 2014 | PASMO | Guatemal, El Salvador, Nicaragua, Costa Rica, and Panama | Central America | MSM | Quasi-experimental using statistical matching technique | 3531 |
| Futterman et al43 | 2010 | Mamekhaya Programme | South Africa | Africa | Pregnant women | Pre/post with comparison | 160 |
| Go et al39 | 2015 | Sexual and Injecting Risk Reduction among HIV-infected PWID | Vietnam | Asia | MSM | Randomised controlled trial | 810 |
| Kerrigan et al46 | 2017 | Project Shikamana | Tanzania | Africa | FSW | Community-randomised controlled trial | 496 |
| Mergenova et al40 | 2018 | Project Nova | Kazakhstan | Central Asia | FSW, PWID | Cluster-randomised controlled trial | 354 |
| Ramakrishnan et al49 | 2011 | Avahan Initiative | India | Asia | FSW | Cross-sectional | 9667 |
| Souverein et al44 | 2012 | Pragati | India | Asia | FSW | Observational study | 17 092 |
| USAID36 | 2014 | PrevenSida | Nicaragua | Central America | FSW, MSM, transgender | Pre/Post | 1393 |
| Wirtz et al45 | 2015 | Comprehension HIV Prevention Intervention | Malawi | Africa | MSM | Prospective pre/post | 103 |
FSW, female sex workers; MSM, men who have sex with men;PASMO, The Pan-American Social Marketing Organization; PWID, people who inject drugs; USAID, United States Agency for International Development.
Target populations
Studies with FSW (n=7), MSM (n=5), pregnant or postpartum young women (n=2), PWID (n=2) and young women in a high burden settings (n=1) were identified.
Study designs
All studies had quantitative study designs. Four studies employed a cluster or individual-level randomised controlled trial design.37–40 Five studies used a pre/post design,36 41–45 and one reported baseline data from a pre/post study.46 Two studies used a cohort study design,47 48 and two used a cross-sectional design with statistical matching.19 49
Risk of bias within studies
The risk of bias assessment was conducted for all studies excluding the two protocols. The 13 remaining studies were separated into two categories: non-randomised and randomised studies. The appropriate assessment tool was used for each group and the results are presented below. The risk of bias assessment of the eight quantitative non-randomised studies was performed based on the ROBINS-I risk of bias tool, which specifies four categories or levels of risk of bias: low, moderate, serious and critical. The results are presented in table 2.
Table 2.
Risk of bias assessment of non-randomised studies
| Arantxa Colchero et al36 | Fatti et al43 | Firestones et al14 | Futterman et al38 | Ramakrishnan et al44 | Souverein et al39 | Wirtz et al40 | USAID31 | |
| Assessment domain | Judgement | |||||||
| Bias due to confounding | Moderate | Low | Low | Moderate | Serious | Low | Moderate | Low |
| Bias in selection of participants into the study | Low | Low | Low | Low | Moderate | Low | Low | Low |
| Bias in classification of interventions | Low | Low | Low | Moderate | Low | Low | Low | Low |
| Bias due to deviations from intended interventions | Moderate | Low | Low | Low | Low | Low | Moderate | Low |
| Bias due to missing data | Moderate | Moderate | Low | Serious | Moderate | Moderate | Low | Moderate |
| Bias in measurement of outcomes | Moderate | Low | Low | Low | Low | Low | Low | Low |
| Bias in selection of the reported result | Low | Low | Low | Low | Low | Low | Low | Low |
| Overall bias | Moderate | Moderate | Low | Serious | Serious | Moderate | Moderate | Moderate |
USAID, United States Agency for International Development.
The study by Colchero et al41 had a moderate risk of bias due to confounding and measurement of outcomes because of its measurement of stigma and discrimination experience as an encounter with healthcare providers in day-to-day healthcare settings rather than a specific instance related to HIV prevention service uptake; moderate bias due to deviations from the intended intervention because of the delay in project intervention and study evaluation, and moderate bias due to missing data because of the absence in reporting of missing data and significantly large loss of participants in the follow-up survey. The research by Fatti et al,48 Souverein et al44 and United States Agency for International Development (USAID, 2014)36 had a moderate risk of bias due to missing data, that is, high lost to follow-up (9%) and rather high rate of participation refusal (139 out of 1583 potential participants) for the former, and the lack of record of missing data and exclusion and lost to follow-up for the last two studies. The article by Wirtz et al had a moderate risk of bias due to deviations from intended interventions because of the delay in the first follow-up given the security threat towards the participants (or MSM in general), that is, crackdown on MSM from the authorities.45 The research by Futterman et al had a serious risk of bias due to missing data given its 66% lost to follow-up,43 and the one by Ramakrishnan et al had a serious bias due to confounding because of the lack of appropriate control over impact from ‘other interventions’ on the outcomes.49
The Cochrane risk of bias tool was used to assess the five randomised controlled trial studies. The tool categorises risks of bias into low, unclear and high. Table 3 indicates that the studies had either low or unclear risk of bias for almost all domains. High risk of bias was found in two domains in two studies: selective reporting and other bias. The research by Mergenova et al had a high reporting bias and other bias given that it did not report the concerned quantitative results, but the study was meant to describe the project execution and its challenges.40 In this regard, the risk assessment of the blinding of outcome assessment was not applicable. The article by Go et al had a high risk of other bias due in part to the research design, that is, long memory recall for people who use drugs (up to 3 months for recall for many primary and secondary outcomes measured) and nature of the participants (people who use drugs).39
Table 3.
Risk of bias assessment of randomised controlled studies
| Cowan et al33 | Chiao et al37 | Mergenova et al35 | Go et al34 | Kerrigan et al41 | |
| Domain | Judgement | ||||
| Random sequence generation (selection bias) | Low | Low | Unclear | Low | Unclear |
| Allocation concealment (selection bias) | Low | Unclear | Unclear | Low | Unclear |
| Blinding of participants and personnel (performance bias) | Low | Unclear | Unclear | Unclear | Low |
| Blinding of outcome assessment (detection bias) (self-reported outcomes) | Unclear | Low | (N/A) | Unclear | Low |
| Blinding of outcome assessment (detection bias) (objective measures) | Low | Low | (N/A) | Low | Low |
| Incomplete outcome data addressed (attrition bias) | Low | Low | Unclear | Low | Unclear |
| Selective reporting (reporting bias) | Unclear | Low | High | Low | Low |
| Other bias | Unclear | Low | High | High | Unclear |
N/A, not applicable.
Results of individual studies
All studies described biomedical, behavioural and structural components of their programmes using the categories defined by the Joint UNAIDS.8 We have outlined these interventions in table 1. The included studies described similar biomedical components that included HIV testing and counselling, condom distribution and linkages to other health services. Unique components included PrEP delivered to youths through mobile health events and voluntary medical male circumcision and family planning.47
Behavioural interventions in all studies had similar elements based on a peer outreach and education model, and some included individual and group counselling sessions as well as using different approaches to counselling such as motivational interviewing, integrated behavioural change communication and cognitive behavioural change, development of a personal safety plan for FSWs and sexual negotiation with clients.19 37 41–43 Unique elements of behavioural interventions included texts to promote rights awareness and group solidarity46; a 24-hour crisis management services with an on-call violence response team and links to medical and legal support for FSWs experiencing violence38; financial literacy and vocational training40; and support for alcohol deaddiction and provision of rest place.44
Structural interventions were more varied but generally included community-wide awareness raising and capacity building components, sensitivity training for stakeholders and support network strengthening activities, and stigma and discrimination reduction activities. Two programmes included microcredit in the forms of a conditional cash transfer and a microfinance with matched-savings programme,40 47 one provided support to access social security grants48 and three programmes offered legal service assistance/support.19 40 44 One programme relied on mass media training in its interventions.19 One study defined its structural component as ‘assessment, counselling and referral for gender-based violence as required and discussion regarding gender identities and roles,’ which better fits with our definition of a behavioural component as it is primarily a counselling and referral strategy.48 No studies focusing on legal reform were identified.
Synthesis of results
Within the 15 included studies, we identified a total of 73 outcomes: 47 traditional HIV prevention outcomes, 24 empowerment outcomes, 17 inclusion outcomes and 2 agency outcomes being measured (or planned to be measured per the protocols). We have provided details about these outcomes in table 4 for types of intervention components and table 5 for outcomes measures in studies included in the review.
Table 4.
Description of types of intervention components
| Authors | Target population | Biomedical | Behavioural | Structural |
| Colchero et al41 | MSM | Prevention kits (condoms, lubricants and prevention information) distribution | HIV testing and counselling, peer outreach and education, motivational interviewing and group sessions | Stigma and discrimination workshops for public servants (healthcare providers and police officers) |
| Beattie et al37 | FSW | Condom distribution and 24 hours crisis management | HIV/STI testing and counselling, group reflection workshops and intensive support for FSWs and their partners, development of safety plans, one-on-one session with intimate partners, group reflection sessions for intimate partners, training of intimate partner champions, couple events, couple counselling, training of community-based organisation members, strengthening of crisis management teams | Capacity building workshops for FSW community based organisations to respond to and reduce intimate partner violence (IPV), training prominent local leaders to speak against IPV, leadership building, staging public performances that promote intolerance for IPV, community events |
| Buttolph et al47 | Youth in high-burden settings | Condom distribution, voluntary medical male circumcision, family planning and contraception, PrEP delivered through mobile health events, HIV care and treatment as prevention | HIV testing and counselling | Conditional cash transfers for HIV-negative, in-school females |
| Chiao et al42 | FSW | Regular health examinations at social hygiene clinic, STI services | HIV testing and counselling, peer outreach and education, support with relationships between client and sex worker, sexual negotiation | Manager training on HIV and STI education, relationships between clients and sex workers, sexual negotiation, and social influence role, condom use policy, condom availability at workplace |
| Cowan et al38 | FSW | Condom distribution, STI services, contraception services | HIV testing and counselling, peer outreach and education, legal advice | Strengthening support networks, community mobilisation to raise awareness of the benefits of ART and PrEP, building leadership skills |
| Fatti et al48 | Pregnant and postpartum women | Condom distribution | HIV testing and counselling, individual counselling and education for women and their male partners on alcohol and substance abuse support, mental health referrals and group HIV prevention education | Assessment and counselling and referral for gender-based violence, discussion regarding gender identities and roles, support to access social security grants by patient advocates |
| Firestone et al19 | MSM | STI services | HIV testing and counselling, peer and online outreach and education using integrated behavioural change communication | Referrals to designated service providers for support groups, drug and alcohol treatment, legal support, and violence prevention services; sensitisation training of healthcare providers, media training, and mobilisation of civil society leaders to foster public dialogue on homophobia and discrimination |
| Futterman et al43 | Pregnant women | Standard PMTCT care | Cognitive behavioural intervention by peer mentors | Support network of trained mentor mothers who were coping well who were trained to provide support through pregnancy and in the weeks following delivery |
| Go et al39 | PWID | Condom provision | HIV counselling and testing, partner testing, individual and group counselling on stigma, social support and disclosure, dyad session with ‘person important to me’ | Community-wide video and HIV education sessions delivered by a trained community mobilizer, standard message via loudspeakers and educational pamphlets |
| Kerrigan et al46 | FSW | Condom distribution | HIV counselling and testing, peer outreach and education, texts to promote awareness, solidarity, and adherence | Sensitivity training for healthcare providers, drop-in centre with activities that promote social cohesion and community mobilisation to address stigma, discrimination, violence prevention, and financial insecurity |
| Mergenova et al40 | FSW, PWID | HIV and STI treatment | HIV and STI testing, HIV-risk reduction sessions, financial-literacy training, vocational training | Microfinance and a matched-savings programme, connection to necessary medical, legal and social assistance |
| Ramakrishnan et al49 | FSW | Condom distribution, STI services | HIV testing and counselling, peer outreach and education | Community mobilisation for greater ownership among high risk groups |
| Souverein et al44 | FSW | STI services, condom use demonstration and distribution | HIV and STI testing and treatment, peer educators and outreach, support for alcohol deaddiction and provision of rest place | Saving and credit service, options for alternative and diversified livelihoods, sensitising activities for brothel owners, pimps, and the police; support for group action and a collective of sex worker, provision of relevant legal information |
| USAID36 | MSM, FSW, TG | Condom use and distribution, STI services | HIV testing and counselling, peer educators and outreach, interpersonal communication, group sessions | Strengthening institutional capacity of NGOs serving at risk communities and improving participation of NGOs representing MARPs and PLHIV in the HIV/AIDS national response |
| Wirtz et al45 | MSM | STI services | Peer outreach and education | Training of healthcare providers on risk reduction counselling and equitable service delivery and peer educators to provide epidemiological evidence to support decriminalisation of homosexuality and advocate for great inclusion |
ART, antiretroviral therapy; FSWs, female sex workers; MARP, most at risk population; MSM, men who have sex with men; NGO, non-governmental organisation; PLHIV, people living with HIV; PMTCT, prevention of mother-to-child transmission; PrEP, pre-exposure prophylaxis; PWID, people who inject drugs; STI, sexually transmitted infection; TG, transgender; USAID, United States Agency for International Development.
Table 5.
Outcomes measures in studies included in the systematic review
| Authors | Target population | Direction of effect of findings | Traditional HIV prevention outcomes | Empowerment outcomes | Inclusion outcomes | Agency outcomes |
| Colchero et al41 | MSM | Effect favours intervention | (1) HIV testing, (2) no of sexual partners, (3) awareness of HIV status, (4) HIV positive on treatment, (5) condom use at last sex | None | (1) Self-reported perception of stigma and discrimination from healthcare providers | None |
| Beattie et al37 | FSW | N/A | (6) Consistent condom use in the past 6 months | (1) Self-efficacy to negotiate condom use and HIV/STI testing, (2) increased disclosure of IPV, (3) decreased acceptance of violence by partner, (4) increased knowledge of self-protection strategies and sources of support for IPV | (2) Increased solidarity among FSWs around IPV | None |
| Buttolph et al47 | Youth in high-burden settings | N/A | (7) Adherence (PrEP and ART), (8) voluntary medical male circumcision, (9) contraceptive use, (10) HIV rapid test (11) HIV knowledge | None | (3) Keeping girls in school (school attendance) | None |
| Chiao et al42 | Pregnant and postpartum women | Effect favours intervention | (12) HIV testing, (13) six-item consistent condom use scale | (5) HIV perceived control and severity | (4) Social support, employer’s supportive attitude, (5) can talk to employer about condoms | None |
| Cowan et al38 | PWID | Effect favours intervention | (14) Knowledge of HIV status, (15) reported condomless sex with client in past month, (16) HIV positive on treatment | (6) Reporting good relationship with other FSW | None | None |
| Fatti et al48 | FSW | Effect favours intervention | (17) HIV incidence, (18) HIV testing | (7) Receiving support to access social security grants | None | None |
| Firestone et al19 | MSM | Effect favours intervention | (19) Condom and lubricant use at last sex, (20) consistent condom use in past 30 days, (21) HIV test in past 12 months, (22) seeking treatment for STI past 12 months | (8) Friends’ knowing the respondents’ sexual orientation, (9) being out with friends, (10) participating in gay or TG events, (11) ever visited a gay bar/disco | None | None |
| Futterman et al43 | Pregnant women | Effect favours intervention | (23) Adherence to PMTCT practices, (24) HIV knowledge score | (12) Emotional functioning, (13) HIV discomfort score, (14) depression scale, (15) COPE Inventory, (16) interaction and bonding score, (17) disclosing status to partner or family member | (6) Social support (availability and satisfaction) | None |
| Go et al39 | MSM | Effect favours neither | (25) HIV Incidence, (26) direct/indirect sharing of needles, injecting drugs, solution and distilled water in past 3 months, (27) frequency of injecting, (28) unprotected sex in past 3 months, (29) HIV knowledge | (18) Depression, (19) HIV status disclosure | (7) HIV-related stigma scale, (8) IDU-related stigma scale, (9) social support scale, (10) injecting network size | None |
| Kerrigan et al46 | FSW | N/A | (30) HIV incidence, (31) consistent condom use in past 30 days per partner type | (20) Gender-based violence experience | (11) Experiences of stigma and discrimination, (12) sex work stigma in community, (13) social cohesion, (14) participation in community mobilisation | None |
| Mergenova et al40 | FSW, PWID | N/A | (32) Biologically confirmed STI and (33) HIV rate, (34) unprotected sexual acts, (35) unsafe injection | (21) Condom use self-efficacy, (22) sexual communication skills, (23) savings | (15) Perceived stigma, (16) social norms score, (17) social support | None |
| Ramakrishnan et al49 | FSW | Effect favours intervention | (36) HIV prevalence, (37) consistent condom use with occasional and regular clients, (38) treatment for HIV and STIs, (39) knowledge of HIV transmission | None | None | None |
| Souverein et al44 | FSW | Effect favours intervention | (40) STI incidence rate, (41) condom use at last paid sex | None | None | None |
| USAID36 | FSW, MSM, TG | Effect favours intervention | (42) HIV testing, (43) no of sex partners, (44) consistent condom use in last relationship | (24) Trust in service/social support networks | None | (1)Recognition of unmet rights, (2) participation in political organisations, HIV association, including peer group socialisation, and government |
| Wirtz et al45 | MSM | Effect favours intervention | (45) Condom use at last sex, (46) use of lubricants, (47) casual male partners | (25) Disclosure of sexual orientation to family and healthcare providers | None | None |
For protocols, we reported outcomes the authors plan to measure in the coming study but have not yet measured.
ART, antiretroviral therapy; FSW, female sex workers; IDU, injecting drug users; IPV, intimate partner violence; MSM, men who have sex with men;N/A, not applicable; PMTCT, prevention of mother-to-child transmission; PrEP, pre-exposure prophylaxis; PWID, people who inject drugs; STI, sexually transmitted infection;TG, transgender; USAID, United States Agency for International Development.
The most commonly reported traditional prevention outcome was condom use with 12 out of 15 studies reporting some measures of condom use. Condom use was measured in a wide variety of ways including frequency of consistent condom use in last relationship,36 consistent condom use in the past 6 months,37 unprotected sex in the past 3 months,39 consistent condom use in the past 30 days per partner type,19 38 46 condom use at last sex,19 36 42 45 condom use at last paid sex44 and a six-item consistent condom use scale.42 Some did not report a time period for their measurement including: number of unprotected sexual acts40 and consistent condom use with occasional and regular clients.49 Other traditional prevention outcomes measures included HIV and STI incidence/rate, testing and treatment, knowledge about HIV and treatment, and prevention adherence. Only one study measured male circumcision and contraceptive use.47
Very few empowerment outcomes were repeated between studies. Four studies did not measure empowerment outcomes at all.42 44 47 49 Two studies reported measuring MSM sexual orientation disclosure status,19 45 and two studies reported measuring HIV disclosure status.39 43 The two protocol/implementation studies reported planning to measure condom use self-efficacy.37 40 Two studies reported measuring trust in support networks in the following ways: reporting good relationship with other FSWs38 and trust in service/social support networks.36 Two studies measured or planned to measure financial security-related outcomes.40 48
Inclusion outcomes were similarly diverse. Almost half of the studies (7 out of 15) did not measure inclusion outcomes. The most measured outcome was social support measured as employers’ supportive attitudes,42 social support availability scale and social support satisfaction scale,43 Medical Outcomes Study social support scale39 and social cohesion scale,40 46 also measured as solidarity among FSWs on intimate partner violence.37 The next most measured outcome was perceptions of stigma and discrimination measured as self-reported perceptions of stigma and discrimination from healthcare providers,41 perceived stigma40 and sex work stigma.46 One study measured keeping girls in school.47
Only one study (the sole non-academic paper in this review) measured agency. Two agency outcomes, that is, recognition of unmet rights and participation in political organisations, HIV association and government were measured in the USAID study.36
Relationships between traditional HIV prevention and empowerment outcomes
In order to determine to what extent the included evaluations measured the relationship between HIV prevention outcomes and empowerment, inclusion and agency outcomes, we examined what relationships in these two categories were measured, and we documented the direction of the relationship. The results are presented in table 6.
Table 6.
Relationships between HIV and empowerment outcomes
| Authors | Target population | Traditional HIV prevention outcomes (outcome 1) | Empowerment, inclusion and agency outcomes (outcome 2) | Relationship between outcomes 1 and 2 measured or not | List of relationships measured | Direction of relationship |
| Colchero et al41 | MSM | (1) HIV testing, (2) no of sexual partners, (3) awareness of HIV status, (4) HIV positive on treatment, (5) condom use at last sex | (1) Self-reported perception of stigma and discrimination from healthcare providers | Not measured | (NA) | (NA) |
| Beattie et al37 | FSW | (6) Consistent condom use | (2) Self-efficacy to negotiate condom use and HIV/STI testing, (3) increased disclosure of IPV, (4) decreased acceptance of violence by partner, (5) increased knowledge of self-protection strategies and sources of support for IPV, (6) Increased solidarity among FSWs around IPV | (NA) | (NA) | (NA) |
| Buttolph et al47 | Youth in high-burden settings | (7) Adherence (PrEP and ART), (8) voluntary medical male circumcision, (9) condom and contraceptive use, (10) HIV rapid test | (7) Keeping girls in school (school attendance) | (NA) | (NA) | (NA) |
| Chiao et al42 | FSW | (11) HIV testing, (12) consistent condom use | (8) HIV perceived control and severity, (9) social support, employer’s supportive attitude, (10) can talk to employer about condoms | Measured | (1) HIV testing, employers' supportive attitude; (2) consistent condom use, employer's supportive attitude, can talk to employer about condoms; (3) HIV testing, employer's supportive attitude, HIV perceived control and severity; (4) consistent condom use, employer's supportive attitude, can talk to employer about condoms, HIV perceived control and severity | Positive |
| Cowan et al38 | FSW | (13) Knowledge of HIV status, (14) reported condomless sex with client in past month, (15) HIV positive on treatment | (11) Reporting good relationship with other FSW | Not measured | (NA) | (NA) |
| Fatti et al48 | Pregnant and postpartum women | (16) HIV incidence, (17) HIV testing | (12) Receiving support to access social security grants | Not measured | (NA) | (NA) |
| Firestone et al19 | MSM | (18) Condom and lubricant use at last sex, (19) consistent condom use in past 30 days, (20) HIV test in past 12 months, (21) seeking treatment for STI past 12 months | (13) Friends’ knowing the respondents’ sexual orientation, (14) being out with friends, (15) participating in gay or TG events, (16) ever visited a gay bar/disco | Not measured | (NA) | (NA) |
| Futterman et al43 | Pregnant women | (22) Adherence to PMTCT practices, (23) HIV knowledge score | (17) Emotional functioning, (18) HIV discomfort score, (19) depression scale, (20) COPE scale, (21) interaction and bonding score, (22) disclosing status to partner or family member, (23) social support (availability and satisfaction) | Not measured | (NA) | (NA) |
| Go et al39 | MSM | (24) HIV Incidence, (25) direct/indirect sharing of needles, injecting drugs, solution and distilled water in past 3 months, (26) frequency of injecting, (27) unprotected sex in past 3 months, (28) HIV knowledge | (24) Depression, HIV status disclosure, (25) HIV-related stigma scale, (26) IDU-related stigma scale, (27) social support scale, (28) injecting network size | Not measured | (NA) | (NA) |
| Kerrigan et al46 | FSW | (29) HIV incidence, (30) consistent condom use | (29) Experiences of stigma and discrimination, (30) sex work stigma in community, (31) social cohesion, (32) participation in community mobilisation, (33) GBV violence experience | Not measured | (NA) | (NA) |
| Mergenova et al40 | FSW, PWID | (31) Biologically confirmed STI and (32) HIV rate, (33) unprotected sexual acts, (34) unsafe injection | (34) Condom use self-efficacy, (35) sexual communication skills, (36) savings, (37) perceived stigma, (38) social norms score, (39) social support | Not measured | (NA) | (NA) |
| Ramakrishnan et al49 | FSW | (35) HIV prevalence, (36) consistent condom use, (37) treatment for HIV and STIs, (38) knowledge of HIV transmission, (39) sexual behaviour | None | (NA) | (NA) | (NA) |
| Souverein et al44 | FSW | (40) STI incidence rate, (41) condom use | None | (NA) | (NA) | (NA) |
| USAID36 | FSW, MSM, TG | (42) HIV testing, (43) no of sex partners, (44) consistent condom use | (40) Trust in service/social support networks, (41) recognition of unmet rights, (42) participation in political organisations, HIV association, including peer group socialisation, and government | measured | (1) Consistent condom use, participation in PrevenSida or identifying HIV association | Positive |
| (1) Consistent condom use, peer group socialisation | Neutral | |||||
| Wirtz et al45 | MSM | (45) Condom use at last sex, (46) use of lubricants, (47) casual male partners | (43) Disclosure of sexual orientation to family and healthcare providers | Not measured | (NA) | (NA) |
This analysis excludes studies that do not measure empowerment, inclusion, and agency outcomes and study protocols given their irrelevance.
ART, antiretroviral therapy; FSW, female sex workers; GBV, gender-based violence; IDU, injecting drug users; IPV, intimate partner violence; MSM, men who have sex with men; NA, not applicable (direction of relationship is positive, negative or neutral);PMTCT, prevention of mother-to-child transmission; PrEP, pre-exposure prophylaxis; PWID, people who inject drugs; STI, sexually transmitted infection; TG, transgender; USAID, United States Agency for International Development.
Of the 15 included studies, nine studies did not measure relationships between HIV prevention outcomes and empowerment, inclusion or agency.19 38–41 43 45 46 48 Two studies measured relationships between HIV prevention outcomes and empowerment, inclusion and agency outcomes.36 42 Four were excluded for their irrelevance to the analyses because they were protocols or baseline findings.37 44 47 49
Chiao et al performed a quasi-experimental evaluation of a multilevel social action based theory intervention for FSWs on four islands in the southern Philippines.42 The study examined two different programme components—peer counselling and managers training—at individual sites and also combined at one site, all compared with a control site. Of these four sites, the manager training site had the most significant increase in consistent condom use. Specifically, they found that FSWs who had a manager with a supportive attitude (inclusion outcome) and who encouraged protective behaviours through weekly meetings were more likely to use condoms consistently (traditional HIV prevention outcome).
USAID performed a midterm evaluation of the national HIV response programme PrevenSida in Nicaragua for MSM.36 The evaluation used information from a large monitoring database populated by several national response governing bodies that collected data on programme coverage as well as changes in protective behaviours. The cross-sectional analysis presented in this report found that neither participation in peer group socialisation sessions provided by PrevenSida or the number of interpersonal contacts was associated with an increase in odds of consistent condom use, but there was a positive association between participation in PrevenSida and participation in some kinds of organisations (NGO, HIV association, political organisation or government programme) (agency outcome) and consistent condom use as measured by a ‘consistent condom use index’ (traditional HIV prevention outcome).
Discussion
The findings of this review indicate that combination HIV prevention programmes for marginalised populations have delivered a variety of theory-based biomedical, behavioural and structural interventions and measure changes in empowerment, inclusion and agency. However, although each combination prevention intervention included behavioural and structural components, we found that empowerment, inclusion and least of all agency were not measured consistently or in a standardised way. When these outcomes were measured, analyses of their relationships with HIV prevention outcomes were rare. Out of our 15 included studies, only two measured the relationship between an inclusion or agency outcome and an HIV prevention outcome.
Many authors described how social support, self-efficacy, stigma reduction, encouraging community dialogues, strengthening support networks, and stigma and discrimination workshops for public servants were essential in reducing HIV incidence. However, there was little evidence to support this as the primary and secondary outcomes measured in the studies remained in the biomedical realm of HIV incidence, HIV testing, consistent condom use and the number of partners. Therefore, it remains unclear how and why structural components in combination prevention programmes contribute to biomedical outcomes.
The combination HIV prevention programmes included in our review focused extensively on the structural components of the intervention, which were also rather diverse. Most described community-wide awareness raising, sensitivity training for stakeholders and microfinance. The structural component targeted the immediate community levels (eg, FSW ‘communities’, MSM ‘communities’), while a few involved employers/managers, the local governments and law enforcement officials. The ‘higher’ structural-level interventions such as national-level legal or policy change and creating more politically favourable environment in support of the key issues to be dealt with, such as legalising sex work or legal recognition of MSM, were generally absent. The interventions also favoured tackling social rather than political and/or economic facets of the issues; there were only five subcomponents that tackled financial security. However, existing literature indicates that there is a need to tackle these ‘higher’ and more complicated structural issues, which can present significant constraints to HIV prevention success and intervention sustainability and drive up the disease burden, in order to systematically improve the socioeconomic status and (comprehensive, including psychological and mental) healthcare of the populations.3 10 15 50–57 This argument is, nevertheless, not meant to downplay the importance of and need to tackle the ‘lower’ level structural issues and the non-structural interventions as well as the challenges in dealing with the bigger picture.10 51 53 56 57
We found that the combination HIV prevention programmes for marginalised populations included in this review described underlying theories of change that identify aspects of empowerment, inclusion and agency as intermediary and necessary steps on the pathway. However, in their evaluations, few measured empowerment, fewer measured inclusion and still fewer measured agency. This absence of measurement is in stark contrast to the global and national rhetoric of empowerment, inclusion and agency to demand equal rights in the health sector as well as in the broader society.8 30 31 52 58
The absence of measurement has made the response to the main inquiry in our systematic review rather incomplete. Our second research question asked about the extent to which included evaluations measure the relationships between empowerment and HIV prevention outcome. We found that 2 out of 15 studies measured the relationship between traditional HIV prevention outcomes and empowerment, inclusion and agency outcomes. According to these two studies, two out of the three relationships measured were positive. Our third question asks if there is sufficient evidence to support that improved agency to demand rights leads to improved HIV prevention outcomes. To this question, our review is inconclusive. Only 1 study out of 15 measured agency outcomes and tested three associations (not causal relationship) between the agency outcomes: (1) participation in PrevenSida, (2) being able to identify or participate in an HIV association and (3) peer group socialisation and one traditional HIV prevention outcome (consistent condom use). They found a positive relationship between the first two agency outcomes and condom use.
Outcomes related to empowerment, inclusion and agency were scarce but diverse. They included self-reported perceptions of stigma and discrimination from healthcare personnel, perceived control over HIV risk and its severity, sexual communication skills, social norm scales, gender-based violence counselling or referral and HIV stigma. HIV prevention requires the involvement of the marginalised individual and their communities. It also involved the broader societies. Their empowerment to tackle the issues they face is essential. Measuring empowerment outcomes and their relationship with the traditional outcomes is a necessary step towards accelerating HIV prevention.8 52 54
Another note is that the comprehensive evaluation studies and protocols focused disproportionally on a few marginalised populations and missed out on the others, and this can have implications for public policy interventions as well as comprehensive HIV programme evaluation studies. FSWs was the focus in seven studies, MSM in five studies, and adolescent girls and young women in three studies. Two studies covered PWID; one project evaluation study covered TG women; and no study covered people in prisons or other closed settings. In addition, none of the evaluations used qualitative research methods or mixed methods, which can augment the measurement of abstract concepts and experiences of empowerment, inclusion and agency to demand equal rights.
Limitations of the review
There are a few limitations in this study. First, our systematic review only included studies and protocols published in English due to the limitations of the authors. However, we did not encounter any non-English abstracts in our search so we were unlikely to miss eligible articles. Second, we performed the review only on studies and protocols that aimed to evaluate combination HIV prevention programmes. This excluded studies that adopted merely two of the three intervention components (biomedical, behavioural and structural), which could have shed light on the measurement of empowerment, inclusion and agency outcomes and the relationship between the outcomes and traditional HIV prevention outcomes.1 Third, we were not able to perform a synthesis of the effect sizes and meta-analysis due to the heterogeneity of interventions and outcomes, and therefore, we cannot make any statements about the effect of empowerment, inclusion and agency that may have been helpful to programme planners and policy-makers.
Fourth, the authors of this review defined the four outcome categories and placed the measures into those categories. This introduces a level of subjectivity that may limit the generalisability of this review. We employed commonly used definitions and double data extraction to carry out our categorisation and to reduce subjectivity. Fifth, some larger programmes may have several evaluations that collect and present data on other outcomes that we did not find in our search. Larger programmes’ names were used in keyword searches (Avahan, PrevenSida and Pragati) to find other evaluations that might include non-traditional HIV prevention outcomes. The evaluation that included the most comprehensive reporting of main results was the included study. Finally, as with any review, this review is subject to publication bias and may be more likely to contain studies that had positive findings that had more funding or staff or those that had other supportive factors that would make it more likely for them to be published. We searched the grey literature in order to capture a balanced perspective but all except one of our included studies came from peer-reviewed journals.
Conclusions
Findings from this review provide important information for policy-makers, programme planners, and researchers and directions for future research.
Implications for policy-makers and funders
Nearly four decades into the HIV pandemic, structural barriers continue to pose challenges to HIV prevention among marginalised populations. Therefore, it is essential to properly measure whether and how combination prevention programmes affect the empowerment, inclusion and agency of the people they aim to serve. Yet, we found that despite the heavy emphasis in the HIV prevention community on combination programming, the included evaluation studies focused heavily on monitoring and evaluating traditional HIV prevention outcomes. One reason for this may be the emphasis by policy-makers and funders to demonstrate biomedical results and immediate success. We encourage policy-makers and funders to consider the intermediate steps on the pathways to increased condom use and HIV testing to be as important as the primary outcomes as they can explain the ‘how’ of their achievements, which will support replication and expansion of programmes that are working, so as to ensure sustainability of the programmes. In this sense, key global players like the Global Fund, the Bill and Gates Foundation, and UNAIDS could play a key role in promoting this endeavour and can even come together to agree on the measurement and outcome issues.
Implications for programme implementers
We found that, while theories underscored many of the interventions described in the included studies, the reach of the structural components was limited. Understanding the many possible reasons why programming is limited including staff time, capacity and funds, we encourage programme implementers and planners to look beyond the immediate community level in order to change the larger context within which marginalised populations access healthcare. In this regard, design and implementation of the combination prevention programmes should try to adhere to the recommendations in the UNAIDS’s report (2010), and individuals’ empowerment, inclusion and agency for change should feature in the programmes and their monitoring and evaluation, accordingly.
Implications for researchers
We found a lack of measurements of empowerment, inclusion and agency outcomes. Our findings suggest that research on combination prevention would benefit from interdisciplinary approaches spanning beyond public health, with meaningful engagement of communities in research priority setting and design, as well as incorporating perspectives from social sciences and humanities. We encourage public health researchers to rely on conceptual frameworks or theories of change to guide both programme development and evaluations.
As indicated in the introduction, our review is perhaps the first one that looks into the impacts of combination HIV prevention programmes on individuals’ empowerment, inclusion and agency for changes. Further similar reviews and studies are required to better understanding the relationships between programme design and implementation and its impact on individuals’ empowerment and involvement. One potential review, for example, may inquire the relationship between contexts, mechanisms and outcomes, examining how and why outcomes can vary substantially by contexts and are related to the particular mechanisms and interventions employed in a given setting and the types of outcomes measured. Further research studies may want to explore how public health policy can be better ‘evidence informed’ and contextualised.59 60
Acknowledgments
This study was made possible by the Partnership to Inspire, Transform and Connect the HIV response (PITCH). The PITCH is a strategic partnership between Aidsfonds, Frontline AIDS and the Dutch Ministry of Foreign Affairs.
Footnotes
Handling editor: Stephanie M Topp
Twitter: @PantelichMarija
Contributors: CB, SS, ST, MP, ER and SY conceived the study. CB and SS conducted the search and retrieval. CB, SS and SY conducted the analyses. CB, SS and SY drafted the manuscript. ST, MP and ER reviewed and provided critical inputs. All authors read and approved the final manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: No data are available.
References
- 1.James-Hawkins L, Peters C, VanderEnde K, et al. . Women's agency and its relationship to current contraceptive use in lower- and middle-income countries: a systematic review of the literature. Glob Public Health 2018;13:843–58. 10.1080/17441692.2016.1239270 [DOI] [PubMed] [Google Scholar]
- 2.Alaofè H, Zhu M, Burney J, et al. . Association between women's Empowerment and maternal and child nutrition in Kalalé district of northern Benin. Food Nutr Bull 2017;38:302–18. 10.1177/0379572117704318 [DOI] [PubMed] [Google Scholar]
- 3.Heaton TB. Are improvements in child health due to increasing status of women in developing nations? Biodemography Soc Biol 2015;61:252–65. 10.1080/19485565.2015.1047487 [DOI] [PubMed] [Google Scholar]
- 4.Women UN. Sdg 5: achieve gender equality and empower all women and girls. New York: UN Women, 2017. [Google Scholar]
- 5.Hanmer L, Klugman J. Exploring women's agency and Empowerment in developing countries: where do we stand? Fem Econ 2016;22:237–63. 10.1080/13545701.2015.1091087 [DOI] [Google Scholar]
- 6.Bekker L-G, Johnson L, Cowan F, et al. . Combination HIV prevention for female sex workers: what is the evidence? The Lancet 2015;385:72–87. 10.1016/S0140-6736(14)60974-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Delany-Moretlwe S, Cowan FM, Busza J, et al. . Providing comprehensive health services for young key populations: needs, barriers and gaps. J Int AIDS Soc 2015;18(2(Suppl 1)):19833 10.7448/IAS.18.2.19833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.UNAIDS – Joint United Nations Programme on HIV/AIDS Fast-tracking combination prevention: towards reducing new HIV infections to fewer than 500,000 by 2020. Geneva: UNAIDS, 2015. [Google Scholar]
- 9.UNAIDS – Joint United Nations Programme on HIV/AIDS Combination HIV prevention: tailoring and coordinating biomedical, behavioural and structural strategies 10 to reduce new HIV infections a UNAIDS discussion paper. Geneva: UNAIDS, 2010. [Google Scholar]
- 10.International HIV/AIDS alliance Ending AIDS among people who use drugs: our theory of change. Brighton: International HIV/AIDS Alliance, 2018. [Google Scholar]
- 11.Kerrigan D, Kennedy CE, Morgan-Thomas R, et al. . A community empowerment approach to the HIV response among sex workers: effectiveness, challenges, and considerations for implementation and scale-up. The Lancet 2015;385:172–85. 10.1016/S0140-6736(14)60973-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Awungafac G, Delvaux T, Vuylsteke B. Systematic review of sex work interventions in sub-Saharan Africa: examining combination prevention approaches. Trop Med Int Health 2017;22:971–93. 10.1111/tmi.12890 [DOI] [PubMed] [Google Scholar]
- 13.Conserve DF, Jennings L, Aguiar C, et al. . Systematic review of mobile health behavioural interventions to improve uptake of HIV testing for vulnerable and key populations. J Telemed Telecare 2017;23:347–59. 10.1177/1357633X16639186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Knight R, Karamouzian M, Salway T, et al. . Online interventions to address HIV and other sexually transmitted and blood-borne infections among young gay, bisexual and other men who have sex with men: a systematic review. J Int AIDS Soc 2017;20:e25017 10.1002/jia2.25017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Larney S, Peacock A, Leung J, et al. . Global, regional, and country-level coverage of interventions to prevent and manage HIV and hepatitis C among people who inject drugs: a systematic review. Lancet Glob Health 2017;5:e1208–20. 10.1016/S2214-109X(17)30373-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.MacArthur GJ, van Velzen E, Palmateer N, et al. . Interventions to prevent HIV and hepatitis C in people who inject drugs: a review of reviews to assess evidence of effectiveness. Int J Drug Policy 2014;25:34–52. 10.1016/j.drugpo.2013.07.001 [DOI] [PubMed] [Google Scholar]
- 17.Shangani S, Escudero D, Kirwa K, et al. . Effectiveness of peer-led interventions to increase HIV testing among men who have sex with men: a systematic review and meta-analysis. AIDS Care 2017;29:1003–13. 10.1080/09540121.2017.1282105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bärnighausen T, Bloom DE, Humair S. Health systems and HIV treatment in sub-Saharan Africa: matching intervention and programme evaluation strategies. Sex Transm Infect 2012;88:e2 10.1136/sextrans-2011-050303 [DOI] [PubMed] [Google Scholar]
- 19.Firestone R, Rivas J, Lungo S, et al. . Effectiveness of a combination prevention strategy for HIV risk reduction with men who have sex with men in central America: a mid-term evaluation. BMC Public Health 2014;14:1244 10.1186/1471-2458-14-1244 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Stangl AL, Lloyd JK, Brady LM, et al. . A systematic review of interventions to reduce HIV-related stigma and discrimination from 2002 to 2013: how far have we come? J Int AIDS Soc 2013;16:18734 10.7448/IAS.16.3.18734 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hudelson C, Cluver L. Factors associated with adherence to antiretroviral therapy among adolescents living with HIV/AIDS in low- and middle-income countries: a systematic review. AIDS Care 2015;27:805–16. 10.1080/09540121.2015.1011073 [DOI] [PubMed] [Google Scholar]
- 22.McAteer CI, Truong N-AT, Aluoch J, et al. . A systematic review of measures of HIV/AIDS stigma in paediatric HIV-infected and HIV-affected populations. J Int AIDS Soc 2016;19:21204 10.7448/IAS.19.1.21204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fonner VA, Kennedy CE, O'Reilly KR, et al. . Systematic assessment of condom use measurement in evaluation of HIV prevention interventions: need for standardization of measures. AIDS Behav 2014;18:2374–86. 10.1007/s10461-013-0655-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Catumbela E, Certal V, Freitas A, et al. . Definition of a core set of quality indicators for the assessment of HIV/AIDS clinical care: a systematic review. BMC Health Serv Res 2013;13:236 10.1186/1472-6963-13-236 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kennedy CE, Fonner VA, O'Reilly KR, et al. . A systematic review of income generation interventions, including microfinance and vocational skills training, for HIV prevention. AIDS Care 2014;26:659–73. 10.1080/09540121.2013.845287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Barr D, Amon JJ, Clayton M. Articulating a rights-based approach to HIV treatment and prevention interventions. Curr HIV Res 2011;9:396–404. 10.2174/157016211798038588 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Beyrer C, Baral SD, van Griensven F, et al. . Global epidemiology of HIV infection in men who have sex with men. The Lancet 2012;380:367–77. 10.1016/S0140-6736(12)60821-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kabeer N. Resources, agency, achievements: reflections on the measurement of women's Empowerment. Dev Change 1999;30:435–64. 10.1111/1467-7660.00125 [DOI] [Google Scholar]
- 29.Pratley P. Associations between quantitative measures of women's empowerment and access to care and health status for mothers and their children: a systematic review of evidence from the developing world. Soc Sci Med 2016;169:119–31. 10.1016/j.socscimed.2016.08.001 [DOI] [PubMed] [Google Scholar]
- 30.World Bank Group Inclusion Matters: The Foundation for Shared Prosperity : New frontiers of social policy. Washington DC: World Bank Group, 2013. [Google Scholar]
- 31.Markham S. Women as agents of change: having voice in society and influencing policy. Washington DC: World Bank, 2013. [Google Scholar]
- 32.Sterne JAC, Hernán MA, Reeves BC, et al. . ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016;355 10.1136/bmj.i4919 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Higgins JPT, Altman DG, Gøtzsche PC, et al. . The Cochrane collaboration's tool for assessing risk of bias in randomised trials. BMJ 2011;343:d5928 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bangdiwala SI, Bhargava A, O'Connor DP, et al. . Statistical methodologies to pool across multiple intervention studies. Transl Behav Med 2016;6:228–35. 10.1007/s13142-016-0386-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.da Costa BR, Jüni P. Systematic reviews and meta-analyses of randomized trials: principles and pitfalls. Eur Heart J 2014;35:3336–45. 10.1093/eurheartj/ehu424 [DOI] [PubMed] [Google Scholar]
- 36.United States Agency for International Development (USAID) Mid-Term Performance Evaluation of USAID’s Bilateral VIH Program in Nicaragua. Washington DC: USAID, 2014. [Google Scholar]
- 37.Beattie TS, Isac S, Bhattacharjee P, et al. . Reducing violence and increasing condom use in the intimate partnerships of female sex workers: study protocol for Samvedana plus, a cluster randomised controlled trial in Karnataka state, South India. BMC Public Health 2016;16:660 10.1186/s12889-016-3356-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Cowan FM, Davey C, Fearon E, et al. . Targeted combination prevention to support female sex workers in Zimbabwe accessing and adhering to antiretrovirals for treatment and prevention of HIV (SAPPH-IRe): a cluster-randomised trial. Lancet HIV 2018;5:e417–26. 10.1016/S2352-3018(18)30111-5 [DOI] [PubMed] [Google Scholar]
- 39.Go VF, Frangakis C, Minh NL, et al. . Efficacy of a multi-level intervention to reduce injecting and sexual risk behaviors among HIV-infected people who inject drugs in Vietnam: a Four-Arm randomized controlled trial. PLoS One 2015;10:e0125909 10.1371/journal.pone.0125909 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mergenova G, El-Bassel N, McCrimmon T, et al. . Project nova: a combination HIV prevention and microfinance intervention for women who engage in sex work and use drugs in Kazakhstan. AIDS Behav 2019;23:1–14. 10.1007/s10461-018-2268-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Colchero MA, Bautista-Arredondo S, Cortés-Ortiz MA, et al. . Impact and economic evaluations of a combination prevention programme for men who have sex with men in Mexico. AIDS 2016;30:293–300. 10.1097/QAD.0000000000000925 [DOI] [PubMed] [Google Scholar]
- 42.Chiao C, Morisky DE, Ksobiech K, et al. . Promoting HIV testing and condom use among Filipina commercial sex workers: findings from a quasi-experimental intervention study. AIDS Behav 2009;13:892–901. 10.1007/s10461-008-9418-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Futterman D, Shea J, Besser M, et al. . Mamekhaya: a pilot study combining a cognitive-behavioral intervention and mentor mothers with PMTCT services in South Africa. AIDS Care 2010;22:1093–100. 10.1080/09540121003600352 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Souverein D, Euser SM, Ramaiah R, et al. . Reduction in STIs in an empowerment intervention programme for female sex workers in Bangalore, India: the Pragati programme. Glob Health Action 2013;6:22943 10.3402/gha.v6i0.22943 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Wirtz AL, Trapence G, Jumbe V, et al. . Feasibility of a combination HIV prevention program for men who have sex with men in Blantyre, Malawi. J Acquir Immune Defic Syndr 2015;70:155–62. 10.1097/QAI.0000000000000693 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Kerrigan D, Mbwambo J, Likindikoki S, et al. . Project Shikamana: baseline findings from a community Empowerment-Based combination HIV prevention trial among female sex workers in Iringa, Tanzania. J Acquir Immune Defic Syndr 2017;74 Suppl 1(Suppl 1:S60–S68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Buttolph J, Inwani I, Agot K, et al. . Gender-Specific combination HIV prevention for youth in high-burden settings: the MP3 youth observational pilot study protocol. JMIR Res Protoc 2017;6:e22 10.2196/resprot.5833 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Fatti G, Shaikh N, Jackson D, et al. . Low HIV incidence in pregnant and postpartum women receiving a community-based combination HIV prevention intervention in a high HIV incidence setting in South Africa. PLoS One 2017;12:e0181691 10.1371/journal.pone.0181691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Ramakrishnan L, Gautam A, Goswami P, et al. . Programme coverage, condom use and STI treatment among FSWs in a large-scale HIV prevention programme: results from cross-sectional surveys in 22 districts in southern India. Sex Transm Infect 2010;86 Suppl 1:i62–8. 10.1136/sti.2009.038760 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beyrer C, Sullivan P, Sanchez J, et al. . The increase in global HIV epidemics in MSM. AIDS 2013;27:2665–78. 10.1097/01.aids.0000432449.30239.fe [DOI] [PubMed] [Google Scholar]
- 51.Degenhardt L, Peacock A, Colledge S, et al. . Global prevalence of injecting drug use and sociodemographic characteristics and prevalence of HIV, HBV, and HCV in people who inject drugs: a multistage systematic review. Lancet Glob Health 2017;5:e1192–207. 10.1016/S2214-109X(17)30375-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Salazar X, Núnez-Curto A, Villayzán J, et al. . How Peru introduced a plan for comprehensive HIV prevention and care for transwomen. J Int AIDS Soc 2016;19(3 Suppl 2):20790 10.7448/IAS.19.3.20790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Schunter BT, Cheng W-S, Kendall M, et al. . Lessons learned from a review of interventions for adolescent and young key populations in Asia Pacific and opportunities for programming. J Acquir Immune Defic Syndr 2014;66 Suppl 2:S186–S192. 10.1097/QAI.0000000000000185 [DOI] [PubMed] [Google Scholar]
- 54.Lall P, Lim SH, Khairuddin N, et al. . Review: an urgent need for research on factors impacting adherence to and retention in care among HIV-positive youth and adolescents from key populations. J Int AIDS Soc 2015;18(2 Suppl 1):19393 2S1 10.7448/IAS.18.2.19393 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Weir SS, Baral SD, Edwards JK, et al. . Opportunities for enhanced strategic use of surveys, medical records, and program data for HIV surveillance of key populations: Scoping review. JMIR Public Health Surveill 2018;4:e28 10.2196/publichealth.8042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Yi S, Tuot S, Mwai GW, et al. . Awareness and willingness to use HIV pre-exposure prophylaxis among men who have sex with men in low- and middle-income countries: a systematic review and meta-analysis. J Int AIDS Soc 2017;20:21580 10.7448/IAS.20.1.21580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Beyrer C, Crago A-L, Bekker L-G, et al. . An action agenda for HIV and sex workers. The Lancet 2015;385:287–301. 10.1016/S0140-6736(14)60933-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.World Bank World development report 2012: gender equality and development. Washington DC: World Bank, 2012. [Google Scholar]
- 59.Bowen S, Zwi AB. Pathways to "evidence-informed" policy and practice: a framework for action. PLoS Med 2005;2:e166 10.1371/journal.pmed.0020166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Kingdon JW, Agendas TJA. Alternatives, and public policies. Boston: Little Brown, 1984. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgh-2019-001560supp001.pdf (208.5KB, pdf)
bmjgh-2019-001560supp002.pdf (207.2KB, pdf)
bmjgh-2019-001560supp003.pdf (163.4KB, pdf)


