Abstract
Background:
Amplitude spectrum area (AMSA) of ventricular fibrillation (VF) has been associated with survival from out-of-hospital cardiac arrest (OHCA). Ischemic heart disease has been shown to change AMSA. We studied whether the association between AMSA and survival changes with acute ST-elevation myocardial infarction (STEMI) as cause of the OHCA and/or previous MI.
Methods:
Multivariate logistic regression with log-transformed AMSA of first artifact-free VF segment was used to assess the association between AMSA and survival, according to presence of STEMI or previous MI, adjusting for resuscitation characteristics, medication use and comorbidities.
Results:
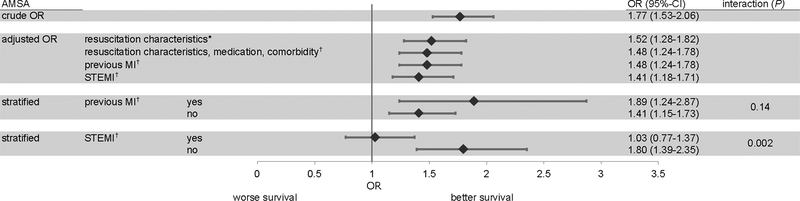
Of 716 VF-patients included from an OHCA-registry in the Netherlands, 328 (46%) had STEMI as cause of OHCA. Previous MI was present in 186 (26%) patients. Survival was 66%; neither previous MI (P=0.11) nor STEMI (P=0.78) altered survival. AMSA was a predictor of survival (ORadj: 1.52, 95%-CI: 1.28–1.82). STEMI was associated with lower AMSA (8.4 mV-Hz [3.7–16.5] vs. 12.3 mV-Hz [5.6–23.0]; P<0.001), but previous MI was not (9.5 mV-Hz [3.9–18.0] vs 10.6 mV-Hz [4.6–19.3]; P=0.27). When predicting survival, there was no interaction between previous MI and AMSA (P=0.14). STEMI and AMSA had a significant interaction (P=0.002), whereby AMSA was no longer a predictor of survival (ORadj: 1.03, 95%-CI: 0.77–1.37) in STEMI-patients. In patients without STEMI, higher AMSA was associated with higher survival rates (ORadj: 1.80, 95%-CI: 1.39–2.35).
Conclusions:
The prognostic value of AMSA is altered by the presence of STEMI: while AMSA has strong predictive value in patients without STEMI, AMSA is not a predictor of survival in STEMI-patients.
Keywords: cardiopulmonary resuscitation, heart arrest, sudden cardiac death, arrhythmia, ST-segment elevation myocardial infarction, quantitative waveform measures, ventricular fibrillation
Introduction
Early defibrillation for ventricular fibrillation (VF) is the most important predictor of survival from out-of-hospital cardiac arrest (OHCA).1 VF morphology may have additional value to predict chances of survival, and can be quantified by continuous VF waveform measures, based on amplitude, frequency, power spectrum, and coarseness of the signal.2 In particular, VF amplitude and frequency decline with increasing time delay from collapse to initial rhythm assessment (call-to-ECG delay); this decline correlates with decreases of high energy phosphates in myocardial cells and coronary perfusion pressure3,4, and can be slowed or reversed by cardiopulmonary resuscitation (CPR).5,6 Accordingly, amplitude spectrum area (AMSA) is one of the most often used quantitative VF waveform measures.
In general, higher VF waveform measures (e.g., higher AMSA) have been associated with higher survival rates in multiple observational studies7–10. This is generally ascribed to their strong correlation with favorable resuscitation characteristics (e.g., public location, bystander witnessed collapse, bystander CPR, short call-to-ECG delay).9 However, patient characteristics may also impact on AMSA and/or survival chances. Ischemic heart disease (both acute and previous myocardial infarction [MI]) has been shown to affect VF waveform measures11–16. We therefore studied whether AMSA may predict survival from OHCA in relation to either acute STEMI as cause of their OHCA or with previous MI in their history, or both.
Methods
Study design, setting and patient selection
The present study used data from the ARREST (AmsteRdam REsuscitation STudies) database, an ongoing prospective registry of all resuscitation attempts in the North-Holland province of The Netherlands. (18) This province has a population of 2.4 million people and covers 2671 km2, with both urban and rural communities, including Amsterdam. We included all patients with OHCA from cardiac causes between July 2005 and December 2011 with electrocardiogram (ECG) VF recordings from LIFEPAK (Physio-Control, Redmond WA, USA) automated external defibrillators (AED) or manual monitor-defibrillators (these defibrillators constitute >90% of all used defibrillators in the study region). We excluded patients with OHCA from clear non-cardiac causes (i.e., drowning, trauma, neurologic causes) or whose medical history or medication use could not be retrieved. The study cohort included the patients who were admitted to hospital, to be able to establish a reliable STEMI diagnosis using hospital diagnostics.
All data were collected according to the Utstein recommendations.17 Written informed consent was obtained from all participants who survived the OHCA. The Medical Ethics Review Board of the Academic Medical Center, Amsterdam, approved the study, including the use of data from patients who did not survive the OHCA.
Data collection
Data collection of the ARREST registry has been described in detail elsewhere.18 In short, for all suspected OHCA calls, dispatch forms with time stamps of start of EMS call and EMS dispatch are collected. After each resuscitation attempt, paramedics routinely send the digital continuous ECG recording from their manual defibrillators to the study center. If an AED was also attached, study personnel collect the ECG recording from the AED. The clock times of AED and manual defibrillator recordings are synchronized with a network clock. Initial rhythm from ECG recordings from ambulance manual defibrillator or AED are assessed by study personnel shortly after the OHCA, and VF is identified as initial rhythm. The impedance channel from the AED or manual defibrillator is used to establish when chest compressions were being given.
Resuscitation characteristics are collected from the dispatch center, first responders, paramedics and hospitals. Complete medication use in the year preceding the OHCA is obtained from the patient’s pharmacy. Medical history of the patients is obtained from the general practitioner (GP) by a study questionnaire. In The Netherlands, virtually every citizen has a GP, and the GP acts as gatekeeper for specialist medical care. Accordingly, the GP receives all medical correspondence. When information from a patient’s GP could not be retrieved, information on medical history is retrieved from hospital records if available. Survival to emergency department (ED), survival to hospital admission and survival to hospital discharge is retrieved from the hospital records. Survival to admission is known from the paramedics run sheet.
Definitions
The primary outcome was survival to hospital discharge, with AMSA as the main predictor variable. AMSA represents a summation of the frequencies in the VF signal weighted by their corresponding amplitudes.19. To calculate AMSA, ECG signals were exported with a sample rate of 125 Hz using Research Exporter (Physio-Control, version 1.2). All digitized signals were exported to MATLAB (R2014B, the Mathwork Inc) for further processing. The first movement and chest compression artifact-free VF segment was manually selected for analysis, along with VF segments prior to every defibrillation. Segments of 2–5 seconds artifact-free VF were band-pass filtered between 4 and 48 Hz. Using a fast Fourier transformation, ECG signals were transformed into the frequency domain. The waveform analysis was performed by one reader (MH) who was blinded to any patient information at the time of analysis.
We assessed whether acute MI was the cause of the OHCA, and whether previous MI was present in the patient’s medical history. Patients were considered to have acute MI if ST-elevation MI (STEMI) was confirmed in the hospital. Diagnosis of STEMI was based on available 12-lead ECGs, troponins, CK-MB and autopsy reports. As the diagnosis STEMI can only reliably be made in-hospital, we only included patients who were admitted to the hospital in this study. Patients were considered to have a previous MI if confirmed by the patient’s GP on a questionnaire, or from hospital records.
As possible confounders, we considered the effect of common cardiovascular medications that could be prescribed following a previous MI. Medication use was classified according to the Anatomical Chemical Therapeutic (ATC) code of the World Health Organization (WHO).20 Patients were considered users during OHCA if the prescription window covered the date of the OHCA. We included beta-blockers (ATC CO7), ACE-inhibitors (ATC C09A), anti-platelet therapy (ATC B01AC), lipid modifying medication (ATC C10AA) and loop-diuretics (ATC C03C). We also included heart failure (as a possible consequence of a previous MI) and hypertension (related to the prescribed medication) as potential confounders. These diagnoses were considered present if this was indicated on the questionnaire filled out by the GP, or on hospital case files.
The timestamp of EMS call and time of initial rhythm recording from manual defibrillator or AED was used to calculate the time delay between EMS call and initial rhythm recording and was defined as call-to-ECG delay.
Data analysis
Continuous data with normal distribution are shown as mean±SD, using Student’s T-test or ANOVA to test for significance. Proportions are shown as n (%), using Chi-Square test to test for significance. Variables with a non-normal distribution (AMSA and time-intervals) are expressed as median (interquartile range (IQR)), using Kruskall-Wallis or Mann-Whitney U test where appropriate to test for significance.
We performed logistic regression analyses to evaluate AMSA as predictor of survival to hospital discharge. AMSA was log-transformed before logistic regression analyses and tested for normality after transformation. Resuscitation characteristics, medication use and comorbidities with a univariate association with survival with P<0.10 or univariate differences in AMSA with P<0.10 were subsequently added to the model to evaluate their influence on the association between AMSA and survival. Next, we evaluated the interaction of previous MI and STEMI with AMSA as predictor of survival to discharge, and stratified the analyses accordingly.
All statistical tests were two-tailed, and a P of <0.05 was considered to be statistically significant. Statistics were performed in SPSS 21.0 for Mac.
Results
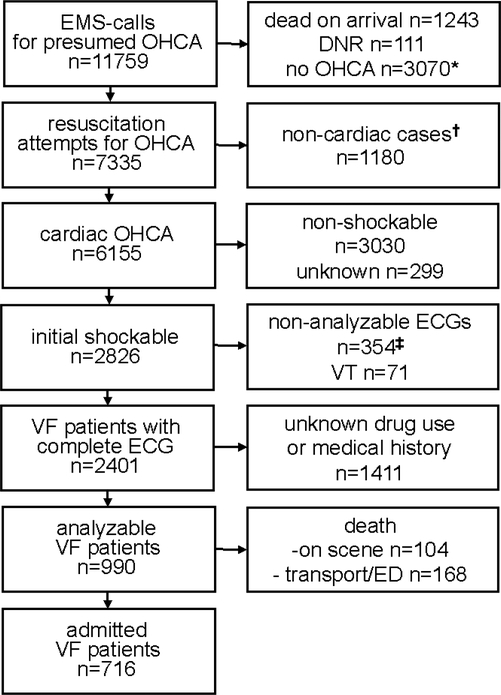
Of the 990 OHCA-VF patients with analyzable ECGs, complete medical- and medication use history, 104 patients (11%) died on the scene. An additional 168 (17%) patients died during transport or at the emergency department before diagnostic information could be obtained. The remaining 716 patients were admitted to the hospital (Figure 1). Of these 716 patients, 471 (66%) were discharged alive. For two patients survival was unknown. The baseline characteristics of the 716 admitted patients are shown in Table 1.
Figure 1: flowchart of patient inclusion between July 4th 2005 and December 31st 2011.
* including 4 patients with successful ICD shock
† including 222 trauma cases, 79 drownings, 326 respiratory causes and 553 other non-cardiac causes (e.g. suicide, intoxications, neurologic, malignancies, aortic dissection/rupture etc.).
‡ including 181 non-LIFEPAK defibrillators, 114 paper tracings, 45 incomplete ECGs and 14 complete ECGs with artifacts such as pacemaker spikes or movement.
DNR denotes do-not-resuscitate; EMS emergency medical history; Hx history; OHCA out-of-hospital cardiac arrest; VT ventricular tachycardia.
Table 1:
Baseline characteristics admitted VF patients
| n (%) | |
|---|---|
| Demographics (N=716) | |
| Age, y (SD) | 64.1 (±14.2) |
| Male sex | 550 (77%) |
| Cause of arrest (N=716) | |
| STEMI | 328 (46%) |
| Disease (N=716) | |
| Previous MI | 186 (26%) |
| Heart failure | 99 (14%) |
| Hypertension | 331 (46%) |
| Current medication use (N=716) | |
| Beta-blockers | 200 (28%) |
| ACE-inhibitors | 117 (16%) |
| Anti-platelet therapy | 140 (20%) |
| Lipid modifying medication | 189 (26%) |
| Loop diuretics | 76 (11%) |
| Resuscitation characteristics (N=716) | |
| Number of defibrillations (median) | 2070 (2) |
| Collapse at public place | 296 (41%) |
| Call-to-ECG delay, min (IQR)* | 7.6 (4.5–10.1) |
| EMS-witnessed collapse | 95 (13%) |
| Excluding EMS-witnessed collapse (N=621) | |
| Bystander witnessed | 553 (89%) |
| Bystander CPR | 496 (80%) |
For 43 patients the EMS-call was made before collapse of the patients. For these patients the delay was adjusted based on the dispatch forms and paramedic information.
Missing values; previous MI n=14, STEMI n=27, heart failure n=27, hypertension n=14, number of defibrillations n=14, witnessed collapse n=5, bystander CPR n=6 and location of collapse n=1. All other variables have no missing values.
CPR denotes cardiopulmonary resuscitation; EMS emergency medical services; IQR interquartile range; MI myocardial infarction; STEMI ST-elevated myocardial infarction; SD standard deviation
AMSA and survival
Mean segment duration of the first artifact-free VF segment was 4.75 sec. Median AMSA for all admitted patients was 10.2 mV-Hz (IQR 4.42–19.0), and was 3.4 mV-Hz (IQR 1.5–9.1, P<0.001) for non-admitted patients. Among patients who were admitted to the hospital, AMSA was higher for surviving patients (12.4 mV-Hz [IQR 6.0–22.4]), than for non-surviving patients (6.33 mV-Hz [IQR 2.78–12.2], P<0.001). The median time from first analyzable VF to first defibrillation was 20.2 sec (IQR 13.9–42.0), during which AMSA increased by 1.33 mV-Hz (±17.3) as a possible effect of CPR.
Table 2 shows the univariate association of demographics, ischemic heart disease, comorbidities, medication use and resuscitation characteristics with AMSA and survival for admitted patients. Previous MI was not associated with a significantly lower AMSA (P=0.27), while STEMI was associated with a 3.9 mV-Hz lower AMSA (P<0.001). None of the analyzed medications or comorbidities were associated with significantly different AMSA. In contrast, most resuscitation characteristics were associated with differences in AMSA; patients with shorter call-to-ECG delay (P<0.001), bystander witnessed collapse (P<0.001) and bystander CPR (P<0.015) had higher AMSA. Neither previous MI (P=0.11) nor STEMI (P=0.78) were associated with different survival rates. Patients with heart failure and users of any medication type (with the exception of lipid modifying medication) had lower survival rates. Younger age, shorter call-to-ECG delay, collapse in public places, EMS- or bystander witnessed collapse and bystander CPR were associated with higher survival rates (Table 2).
Table 2:
AMSA and survival to discharge of all admitted patients in relation to demographics, STEMI, medication use, comorbidities and resuscitation characteristics.
| AMSA (IQR)* | P† | n (% survival) | P‡ | ||
|---|---|---|---|---|---|
| Demographics (N=716) | |||||
| Age | <65 (n=370) | 11.0 (4.4–20.8) | 0.27 | 284 (77%) | <0.001 |
| ≥ 65 (n=346) | 9.7 (4.5–17.0) | 187 (54%) | |||
| Sex | male (n=550) | 8.9 (3.7–20.4) | 0.44 | 367 (67%) | 0.74 |
| female (n=166) | 10.6 (4.6–18.3) | 104 (104%) | |||
| Cause of arrest (N=716) | |||||
| STEMI | yes (n=328) | 8.4 (3.7–16.5) | <0.001 | 222 (68%) | 0.78 |
| no (n=361) | 12.3 (5.6–23.0 | 248 (69%) | |||
| Disease (N=716) | |||||
| Previous MI | yes (n=186) | 9.5 (3.9–18.0) | 0.27 | 114 (61%) | 0.11 |
| no (n=516) | 10.6 (4.6–19.3) | 350 (68%) | |||
| Heart failure | yes (n=99) | 10.3 (4.2–20.5) | 0.89 | 46 (47%) | <0.001 |
| no (n=590) | 10.4 (4.5–19.0) | 410 (70%) | |||
| Hypertension | yes (n=331) | 10.9 (4.3–19.0) | 0.81 | 208 (63%) | 0.11 |
| no (n=367) | 10.1 (4.7–19.7) | 252 (69%) | |||
| Current medication use (N=716) | |||||
| Beta-blockers | yes (n=200) | 9.6 (3.5–18.8) | 0.42 | 119 (60%) | 0.027 |
| no (n=516) | 10.4 (4.7–19.0) | 352 (68%) | |||
| ACE-inhibitors | yes (n=117) | 8.6 (3.8–17.9) | 0.32 | 65 (56%) | 0.011 |
| no (n=599) | 10.5 (4.5–19.3) | 406 (68%) | |||
| Anti-platelet therapy | yes (n=140) | 9.6 (4.4–18.6) | 0.87 | 82 (59%) | 0.045 |
| no (n=576) | 10.5 (4.4–19.0) | 389 (68%) | |||
| Lipid modifiers | yes (n=189) | 9.9 (4.2–18.6) | 0.72 | 118 (62%) | 0.26 |
| no (n=527) | 10.3 (4.5–19.4) | 353 (67%) | |||
| Loop diuretics | yes (n=76) | 10.0 (5.0–19.2) | 0.87 | 33 (43%) | <0.001 |
| no (n=640) | 10.3 (4.4–18.9) | 438 (68%) | |||
| Resuscitation characteristics (N=716) | |||||
| Defibrillations | 1 (n=281) | 12.3 (6.1–22.2) | <0.001 | 201 (72%) | 0.013 |
| >1 (n=421) | 8.7 (3.5–17.5) | 263 (63%) | |||
| Location collapse | home (n=420) | 9.7 (3.9–18.4) | 0.078 | 262 (62%) | 0.022 |
| public (n=296) | 10.1 (4.0–18.8) | 209 (71%) | |||
| Call-to-ECG delay | <8 min (n=456) | 11.7 (5.7–21.1) | <0.001 | 343 (75%) | <0.001 |
| ≥8 min (n=260) | 6.9 (2.8–15.6) | 128 (49%) | |||
| EMS-witnesse | yes (n=95) | 11.1 (5.3–24.5) | 0.099 | 91 (96%) | <0.001 |
| no (n=621) | 9.9 (4.3–18.4) | 377 (617%) | |||
| Excluding EMS-witnessed collapse (N=621)§ | |||||
| Bystander witnessed | yes (n=553) | 10.9 (4.7–19.8) | <0.001 | 346 (63%) | 0.028 |
| no (n=64) | 4.7 (2.3–9.7) | 31 (48%) | |||
| Bystander CPR | yes (n=496) | 10.6 (4.7–19.4) | 0.015 | 315 (64%) | 0.015 |
| no (n= 117) | 7.5 (3.4–15.3) | 60 (51%) | |||
Median AMSA in millivolt per Herz
Mann-Whitney U Test
Mann-Whitney U Test and Chi-Square test
Bystander witnessed collapse, bystander CPR and AED connected not applicable for EMS witnessed collapse (IQR) Missing values; STEMI n=27, heart failure n=26, hypertension n=14, number of defibrillations n=14, witnessed collapse n=4, bystander CPR n=4, survival to discharge n=2. All other variables no missing values.
AED denotes automated external defibrillator; CPR cardiopulmonary resuscitation; EMS emergency medical services; IQR interquartile range; MI myocardial infarction
STEMI and previous MI
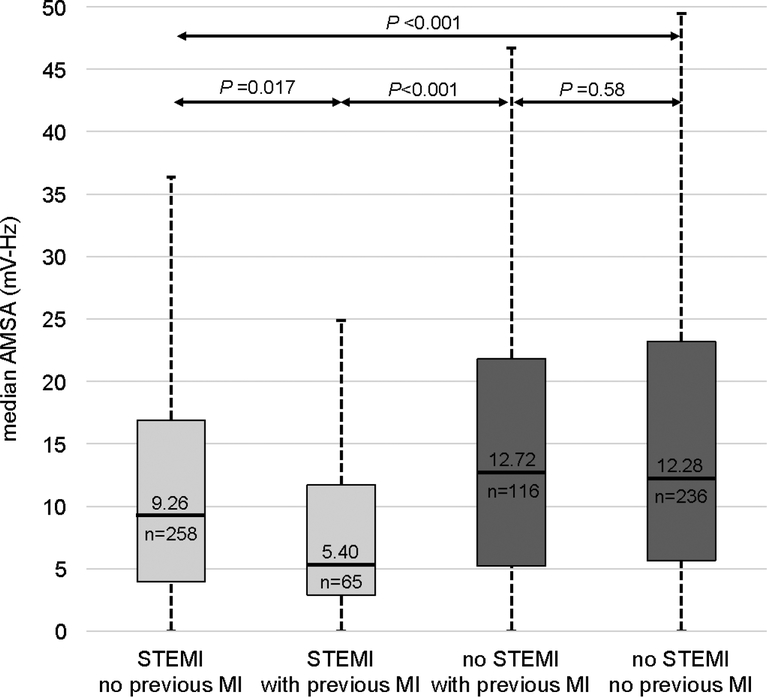
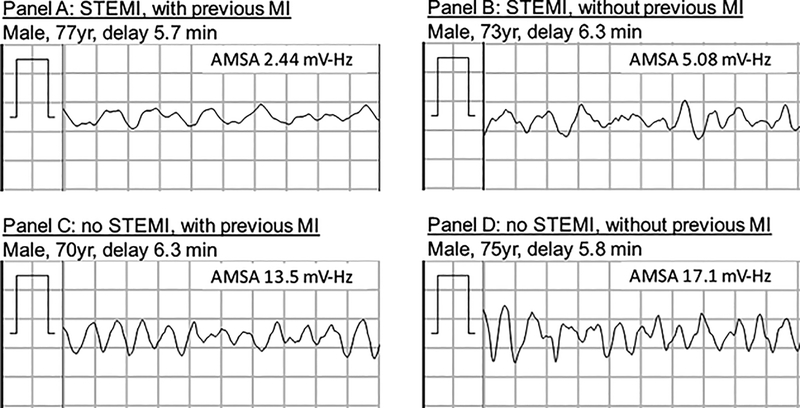
Patients with STEMI had a lower AMSA than patients without STEMI, regardless of previous MI (P<0.001; Figure 2). In patients without STEMI, there was no difference in AMSA between patients with or without a previous MI (P=0.58). However, in patients with STEMI a previous MI was associated with a lower AMSA (P=0.017). This is illustrated in the Figure 3, showing the first analyzable VF segment of four age and call-to-ECG delay matched male patients. The VF signal is more affected by current STEMI than by previous MI.
Figure 2: Tukey box-plot showing AMSA of admitted patients in relation to previous and STEMI.
Box showing interquartile range, whisker showing +/− 1.5 interquartile range. Differences between medians tested with Mann-Whitney U tests.
AMSA denotes amplitude spectrum measure; MI myocardial infarction; STEMI ST-elevated myocardial infarction
Figure 3: VF segment and AMSA of age, sex and call-to ECG delay matched patients.
MI denotes myocardial infarction; STEMI ST-elevated myocardial infarction
Patients with STEMI were more likely to undergo a coronary angiogram during admission (n=300 [93%)] followed by a percutaneous coronary intervention (PCI) (n=274 [84%]), than patients without STEMI (n=254 [71%] and n=88 [24%] respectively (P<0.001).
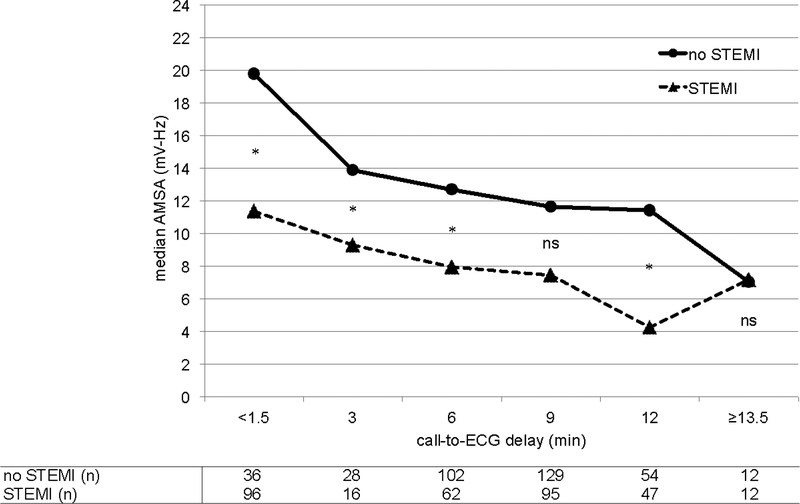
Figure 4 shows the decline in median AMSA with increasing call-to-ECG delay. Already shortly after collapse, patients with STEMI had a lower AMSA. In a linear regression analysis, log-transformed AMSA decreased with increasing call-to-ECG delay with the same rate for patients with STEMI (−0.067 log mV-Hz/min [95%-CI −0.090 to −0.045]) and without STEMI (−0.054 log mV-Hz [95%-CI −0.083 to −0.026]; P=0.47).
Figure 4: time sensitive changes of AMSA in relation to STEMI.
Median AMSA in relation to groups of call-to-ECG delay. Delay <1.5min indicates a delay of less than 1.5 minutes, including 3 indicates a delay between 1.5 and 4.5 min; 6 between 4.5 and 7.5 min; 9 between 7.5 and 10.5 min; 12 between 10.5 and 13.5 min; ≥13.5 more than 13.5 min. Differences between groups were tested using Mann-Whitney U tests with P<0.05 considered statistically significant.
MI denotes myocardial infarction; STEMI ST-elevated myocardial infarction
AMSA as predictor of survival
Logistic regression with log-transformed AMSA shows that AMSA is a predictor of survival (OR 1.77, 95%-CI 1.53–2.06). Also when adjusted for resuscitation characteristics, (bystander or EMS-witnessed collapse, location of collapse, bystander CPR, call-to-ECG delay, number of defibrillations), medication use, heart failure and STEMI or previous MI, AMSA remains a significant predictor of survival (all P<0.001; Figure 5). There was no significant interaction between call-to-ECG delay and AMSA (P=0.38), indicating that AMSA was a significant predictor of survival regardless of call-to-ECG delay. There was no significant interaction between AMSA and previous MI (P=0.11; Figure 5). However, there was a significant interaction between AMSA and STEMI (P=0.003). In patients with STEMI, AMSA was not a predictor for survival to discharge (OR 1.06, 95%-CI 0.80–1.40). Conversely, in patients without STEMI, higher AMSA was associated with higher survival rates (OR 1.86, 95%-CI 1.44–2.41) (Figure 5). Adding presence of coronary angiography or PCI to the logistic regression models did not change the results.
Figure 5: Forest plot of AMSA as predictor of survival to hospital discharge.
*Adjusted for call-to-ECG delay (continuous), EMS- or bystander witnessed collapse, bystander CPR, number of defibrillations (continuous), age (continuous).
†Adjusted for call-to-ECG delay (continuous), EMS- or bystander witnessed collapse, bystander CPR, number of defibrillations (continuous), age (continuous), heart failure, ACE-inhibitors, beta-blocker, and loop-diuretics use and heart failure.
Discussion
We found that AMSA is a predictor of survival to hospital discharge in patients admitted to hospital after an OHCA with VF: a lower AMSA is associated with lower survival rates. However, this prognostic value of AMSA is not present in patients with STEMI: these patients have lower AMSA than patients without STEMI, but AMSA was not predictive of survival to hospital discharge in patients with STEMI. Furthermore, previous MI is only associated with lower AMSA in patients with STEMI as cause of the OHCA.
STEMI and AMSA
High initial AMSA has been shown to be a predictor of short-term and long-term survival and good neurologic outcome in multiple human OHCA studies.8–10,15,21 Using AMSA as a predictor of outcome after OHCA is based on the assumption that AMSA is higher in patients with shorter delay and presence of bystander CPR. However, using a low AMSA as a simple surrogate measure for longer arrest duration has been challenged by several authors.11,16,22, and we confirm with this study that the use of AMSA as predictor for outcome from OHCA is confounded by the presence of STEMI.
As early as 1988 it was observed that in the acute ischemic phase of an MI, VF has a distinct ECG pattern with a low voltage.23 It was suggested that the amplitude of the VF signal might relate to dynamic changes of myocardial perfusion during coronary occlusion and reperfusion.23 In an animal study, AMSA was lower in the setting of STEMI, but only measured before and after the second and subsequent shocks.13 In another animal study, only frequency measures of VF were affected by STEMI in the first five minutes of untreated VF, but AMSA was not.24 As AMSA incorporates both frequency and amplitude measures, it was suggested that amplitude derived measures such as AMSA fail to distinguish different myocardial substrates24. In a human study in OHCA that investigated VF waveform measures in relation to acute MI and chronic coronary heart disease, patients with acute MI also showed significantly lower AMSA.11
We found that survival of STEMI patients was similar to that of patients without STEMI although AMSA was lower. In an animal study, the presence of STEMI was an independent predictor of return of spontaneous circulation (ROSC), and AMSA was no predictor of outcome from cardiac arrest when adjusted for arrest duration and STEMI status.22,24 In a study of comatose patients after OHCA with or without STEMI, survival to hospital discharge was higher for STEMI patients (55 vs. 41%).25 The authors concluded that these differences were caused by treatment differences, as more patients with STEMI underwent coronary angiography. When all patients who underwent coronary angiography were evaluated, no survival differences between patients with and without STEMI were found25. In the present study more patients with STEMI underwent coronary angiography and PCI compared to patients without STEMI, but adding these variables to the logistic regression analyses did not change the results.
Previous MI and AMSA
We found no significant effect of previous MI on AMSA. However, in the subgroup of patients with STEMI a previous MI was associated with lower AMSA. These results suggest than an area with acute myocardial ischemia on top of a previous myocardial scar leads to VF with a very low AMSA. In a very large study in which multiple VF waveform analyses were tested as predictors of defibrillation success and outcome from OHCA, AMSA was lower for patients with a previous MI.15 It is important to note that that study included all OHCA patients, regardless of admission to the hospital. As we aimed to also investigate the effect of STEMI, a hospital-made diagnosis, we had to limit our study cohort to admitted patients. This affects differences in AMSA, as AMSA of non-admitted patients is much lower.
An earlier study showed that a previous MI was associated with a lower AMSA in patients with electrically induced VF during defibrillation testing after cardioverter-defibrillator implantation, but only in the leads of a 12-lead ECG adjacent to the area of infarction. The setting of defibrillation testing excludes the possibility that differences were caused by an acute MI. However, the results of our study can be different, as we performed waveform measurements on non-electrically induced VF using single lead ECGs with usually a short delay from collapse to initial rhythm assessment, which all could lead to differences in VF waveform measures.16,26,27
AMSA as proxy
As expected, we showed a decline in AMSA with longer call-to-ECG delay in both patients with and without STEMI, albeit at a different absolute level (Figure 4). The AMSA of patients with STEMI and a very short delay (<1.5 min) was already lower than the AMSA of patients with a delay of 12 minutes but without STEMI. In patients with STEMI, low amplitude and frequency of VF might rather be used as an indicator of acute ischemia and not as a predictor of survival. This concept has already been proposed by other investigators.11,13 In patients with refractory VF but no ROSC, there is no opportunity to assess ST-elevation and there are no tools to identify STEMI. A low calculated AMSA or a brief visual confirmation of low frequency and low amplitude VF in patients with EMS witnessed collapse and a confirmed short delay might aid prehospital decision making, suggesting transport to a hospital with PCI capabilities as soon as possible.11 The opposite then should certainly be avoided: deciding that further resuscitation is futile because VF has low amplitude.
Limitations
In addition to the limitation of using a cohort of admitted patients, our diagnoses of previous MI, hypertension and heart failure were derived from a questionnaire that was received from the patient’s GP. Although this allows for collection of data from patients who died before transport to a hospital, questionnaire-based diagnoses are less reliable compared to the myocardial infarction diagnosis that was confirmed by more detailed data from hospital records.
We included only AMSA as VF waveform measure. Although this quantitative waveform measure is widely used and incorporates both amplitude and frequency measures, high frequency content of the VF signal largely determines the AMSA value.11,19 Other changes in VF signals that are not solely ampltiude or frequency derived (e.g., organization, coarseness) are less well presented by AMSA.
We included both witnessed and unwitnessed OHCA. In unwitnessed OHCA, call-to-ECG delay is a less accurate proxy for time in cardiac arrest than for witnessed arrest. However, we aimed to analyze the predictive capacity of waveform measures in both witnessed and unwitnessed OHCA. When our analyses were performed in only witnessed OHCA cases the results and conclusions were not different (data not shown).
Conclusions
We found that, when OHCA is caused by STEMI, AMSA of the VF signal is significantly lower than if no STEMI is present. For these patients, lower AMSA is not associated with worse survival to hospital discharge.
Acknowledgements
We thank all dispatch centers, ambulance services and first responders for their cooperation in the ongoing data collection. We thank Remy Stieglis and Paulien Homma for excellent data-management.
Funding sources
M. Hulleman is supported by a grant from the Netherlands Heart Foundation (grant 2013T034). D.D. Salcido is supported by the following research grants; NHLBI 1R01HL117979-01A1 (PI: Menegazzi, In-Kind), NHLBI 5K12HL109068-04 (PI: Yealy) and Laerdal Foundation Grant (PI: Salcido). H.L. Tan and M.T. Blom are supported by the Netherlands CardioVascular Research Initiative: the Dutch Heart Foundation, Dutch Federation of University Medical Centres, the Netherlands Organisation for Health Research and Development, and the Royal Netherlands Academy of Sciences (PREDICT project). H.L. Tan was also supported by the Netherlands Organization for Scientic Research (NWO, grant ZonMW Vici 918.86.616) and the Dutch Medicines Evaluation Board (MEB/CBG). None of the funders were involved in the study design, data collection, analysis, interpretation or in writing of the manuscript.
Footnotes
Disclusures
R.W. Koster is supported by a significant unconditional grant of Physio Control Inc, Redmond WA for the data collection in the ARREST studies. Physio Control Inc was not involved in the study design, data collection, analysis, interpretation or in writing of the manuscript. The other authors report no relevant disclosures.
References
- 1.Sasson C, Rogers MAM, Dahl J, Kellermann AL. Predictors of survival from out-of-hospital cardiac arrest: a systematic review and meta-analysis. Circ Cardiovasc Qual Outcomes. 2010;3:63–81. [DOI] [PubMed] [Google Scholar]
- 2.Callaway CW, Menegazzi JJ. Waveform analysis of ventricular fibrillation to predict defibrillation. Curr Opin Crit Care. 2005;11:192–199. [DOI] [PubMed] [Google Scholar]
- 3.Salcido DD, Menegazzi JJ, Suffoletto BP, Logue ES, Sherman LD. Association of intramyocardial high energy phosphate concentrations with quantitative measures of the ventricular fibrillation electrocardiogram waveform. Resuscitation. 2009;80:946–950. [DOI] [PubMed] [Google Scholar]
- 4.Reynolds JC, Salcido DD, Menegazzi JJ. Correlation between coronary perfusion pressure and quantitative ECG waveform measures during resuscitation of prolonged ventricular fibrillation. Resuscitation. 2012;83:1497–1502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Waalewijn RA, Nijpels MA, Tijssen JG, Koster RW. Prevention of deterioration of ventricular fibrillation by basic life support during out-of-hospital cardiac arrest. Resuscitation. 2002;54:31–36. [DOI] [PubMed] [Google Scholar]
- 6.Eftestøl T, Wik L, Sunde K, Steen PA. Effects of Cardiopulmonary Resuscitation on Predictors of Ventricular Fibrillation Defibrillation Success During Out-of-Hospital Cardiac Arrest. Circulation. 2004;110:10–15. [DOI] [PubMed] [Google Scholar]
- 7.Goto Y, Suzuki I, Inaba H. Frequency of ventricular fibrillation as predictor of one-year survival from out-of-hospital cardiac arrests. Am J Cardiol. 2003;92:457–459. [DOI] [PubMed] [Google Scholar]
- 8.Indik JH, Conover Z, McGovern M, Silver AE, Spaite DW, Bobrow BJ, Kern KB. Association of Amplitude Spectral Area of the Ventricular Fibrillation Waveform With Survival of Out-of-Hospital Ventricular Fibrillation Cardiac Arrest. Journal of the American College of Cardiology. 2014;64:1362–1369. [DOI] [PubMed] [Google Scholar]
- 9.Schoene P, Coult J, Murphy L, Fahrenbruch C, Blackwood J, Kudenchuk P, Sherman L, Rea T. Course of quantitative ventricular fibrillation waveform measure and outcome following out-of-hospital cardiac arrest. Heart Rhythm. 2014;11:230–236. [DOI] [PubMed] [Google Scholar]
- 10.Indik JH, Conover Z, McGovern M, Silver AE, Spaite DW, Bobrow BJ, Kern KB. Amplitude-spectral area and chest compression release velocity independently predict hospital discharge and good neurological outcome in ventricular fibrillation out-of-hospital cardiac arrest. Resuscitation. 2015;92:122–128. [DOI] [PubMed] [Google Scholar]
- 11.Olasveengen TM, Eftestøl T, Gundersen K, Wik L, Sunde K. Acute ischemic heart disease alters ventricular fibrillation waveform characteristics in out-of hospital cardiac arrest. Resuscitation. 2009;80:412–417. [DOI] [PubMed] [Google Scholar]
- 12.Wang H, Tang W, Ristagno G, Li Y, Sun S, Wang T, Weil MH. The potential mechanisms of reduced incidence of ventricular fibrillation as the presenting rhythm in sudden cardiac arrest. Crit Care Med. 2009;37:26–31. [DOI] [PubMed] [Google Scholar]
- 13.Indik JH, Allen D, Gura M, Dameff C, Hilwig RW, Kern KB. Utility of the Ventricular Fibrillation Waveform to Predict a Return of Spontaneous Circulation and Distinguish Acute From Post Myocardial Infarction or Normal Swine in Ventricular Fibrillation Cardiac Arrest. Circ Arrhythm Electrophysiol. 2011;4:337–343. [DOI] [PubMed] [Google Scholar]
- 14.Sherman L, Niemann J, Youngquist ST, Shah AP, Rosborough JP. Beta-blockade causes a reduction in the frequency spectrum of VF but improves resuscitation outcome: A potential limitation of quantitative waveform measures. Resuscitation. 2012;83:511–516. [DOI] [PubMed] [Google Scholar]
- 15.Ristagno G, Mauri T, Cesana G, Li Y, Finzi A, Fumagalli F, Rossi G, Grieco N, Migliori M, Andreassi A, Latini R, Fornari C, Pesenti A. Amplitude Spectrum Area to Guide Defibrillation: A Validation on 1617 Ventricular Fibrillation Patients. Circulation. 2014;:CIRCULATIONAHA.114.010989. [DOI] [PubMed] [Google Scholar]
- 16.Bonnes JL, Thannhauser J, Hermans MC, Westra SW, Oostendorp TF, Meinsma G, de Boer MJ, Brouwer MA, Smeets JLRM. Ventricular fibrillation waveform characteristics differ according to the presence of a previous myocardial infarction: A surface ECG study in ICD-patients. Resuscitation. 2015;96:239–245. [DOI] [PubMed] [Google Scholar]
- 17.Jacobs I, Nadkarni V, Bahr J, Berg RA, Billi JE, Bossaert L, Cassan P, Coovadia A, D’Este K, Finn J, Halperin H, Handley A, Herlitz J, Hickey R, Idris A, Kloeck W, Larkin GL, Mancini ME, Mason P, Mears G, Monsieurs K, Montgomery W, Morley P, Nichol G, Nolan J, Okada K, Perlman J, Shuster M, Steen PA, Sterz F, Tibballs J, Timerman S, Truitt T, Zideman D. Cardiac arrest and cardiopulmonary resuscitation outcome reports: update and simplification of the Utstein templates for resuscitation registries: a statement for healthcare professionals from a task force of the International Liaison Committee on Resuscitation (American Heart Association, European Resuscitation Council, Australian Resuscitation Council, New Zealand Resuscitation Council, Heart and Stroke Foundation of Canada, InterAmerican Heart Foundation, Resuscitation Councils of Southern Africa). Circulation. 2004;110:3385–3397. [DOI] [PubMed] [Google Scholar]
- 18.Blom MT, van Hoeijen DA, Bardai A, Berdowski J, Souverein PC, De Bruin ML, Koster RW, de Boer A, Tan HL. Genetic, clinical and pharmacological determinants of out-of-hospital cardiac arrest: rationale and outline of the AmsteRdam Resuscitation Studies (ARREST) registry. Open Heart. 2014;1:e000112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Povoas HP, Bisera J. Electrocardiographic waveform analysis for predicting the success of defibrillation. Crit Care Med. 2000;28:N210–211. [DOI] [PubMed] [Google Scholar]
- 20.WHO. The Anatomical Therapeutic Chemical Classification System with Defined Daily Doses (ATC/DDD) [Internet]. [cited 2016 Jun 27];Available from: http://www.who.int/classifications/atcddd/en/
- 21.Freese JP, Jorgenson DB, Liu P-Y, Innes J, Matallana L, Nammi K, Donohoe RT, Whitbread M, Silverman RA, Prezant DJ. Waveform analysis-guided treatment versus a standard shock-first protocol for the treatment of out-of-hospital cardiac arrest presenting in ventricular fibrillation: results of an international randomized, controlled trial. Circulation. 2013;128:995–1002. [DOI] [PubMed] [Google Scholar]
- 22.Indik JH, Shanmugasundaram M, Allen D, Valles A, Kern KB, Hilwig RW, Zuercher M, Berg RA. Predictors of resuscitation outcome in a swine model of VF cardiac arrest: A comparison of VF duration, presence of acute myocardial infarction and VF waveform. Resuscitation. 2009;80:1420–1423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rechavia E, Sclarovsky S, Strasberg B, Sagie A, Topaz O, Agmon J. Ventricular fibrillation complicating acute myocardial infarction. Two distinct clinical and electrocardiographic features. Chest. 1988;93:493–498. [DOI] [PubMed] [Google Scholar]
- 24.Indik JH, Donnerstein RL, Hilwig RW, Zuercher M, Feigelman J, Kern KB, Berg MD, Berg RA. The influence of myocardial substrate on ventricular fibrillation waveform: a swine model of acute and postmyocardial infarction. Crit Care Med. 2008;36:2136–2142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kern KB, Lotun K, Patel N, Mooney MR, Hollenbeck RD, McPherson JA, McMullan PW, Unger B, Hsu C-H, Seder DB. Outcomes of Comatose Cardiac Arrest Survivors With and Without ST-Segment Elevation Myocardial Infarction: Importance of Coronary Angiography. JACC: Cardiovascular Interventions. 2015;8:1031–1040. [DOI] [PubMed] [Google Scholar]
- 26.Indik JH, Peters CM, Donnerstein RL, Ott P, Kern KB, Berg RA. Direction of signal recording affects waveform characteristics of ventricular fibrillation in humans undergoing defibrillation testing during ICD implantation. Resuscitation. 2008;78:38–45. [DOI] [PubMed] [Google Scholar]
- 27.Sherman LD, Niemann JT, Rosborough JP, Menegazzi JJ. The effect of ischemia on ventricular fibrillation as measured by fractal dimension and frequency measures. Resuscitation. 2007;75:499–505. [DOI] [PMC free article] [PubMed] [Google Scholar]