Abstract
Context.
Parents of children in the pediatric cardiac intensive care unit (CICU) report inadequate communication and a lack of empathy during conversations with their clinicians.
Objective.
To assess quantitatively and qualitatively the contributions made by team members of different professions in communicating with parents during family meetings.
Methods.
Prospective observational study. The study was conducted in the pediatric CICU at the Children’s Hospital of Philadelphia. Subjects were members of the interprofessional team attending family meetings for patients admitted to the CICU longer than two weeks. We used quantitative conversation attribution and coding to compare durations of attendee contributions and contribution type by professional role. The SCOPE codebook and other quantitative codes drawn from best practices in family meetings were used to measure communication behaviors. A qualitative analysis of nurses’ and social workers’ contributions was used to identify themes not otherwise captured.
Results.
Across 10 meetings, physicians spoke for an average of 78.1% (SD 10.7%) of each meeting, nonphysicians 9.6% (SD 7.8%), and parents 17.4% (SD 12.2%). Parental understanding was assessed an average of 0.2 (SD 0.4) times per meeting. Parents expressed emotion an average of 4.2 times per meeting (SD 7.1), and the clinical team responded empathetically 2.2 times per meeting (SD 4.3). All clinician empathic responses were a minority of their overall contributions. Conversation was almost exclusively between physicians and families until physicians indicated other team members could contribute.
Conclusions.
Coordination of team members’ roles in the meetings may improve parental engagement necessary for decision-making and empathic responses that are often missed.
Keywords: Interprofessional communication, pediatric cardiac intensive care, family meeting, provider-patient communication, interprofessional teams
Most parents of children in the cardiac intensive care unit (CICU) want to share in decision-making with their child’s clinical teams.1–4 Shared decision-making is difficult, however, when various participants have divergent understanding of the patient’s prognosis. Parents of children in the CICU often do not understand that their child has a life-limiting disease until two days before death,5 hampering the shared decision-making process. The underlying breakdown in communication that these misunderstandings implies can undermine the achievement of goal-concordant care6 and leads parents to express dissatisfaction with the decision-making process.7
To improve communication, professional organizations recommend that interprofessional teams and families discuss the diagnosis and treatment options in a family meeting.8 However, there is little guidance on what role each team member should play in these meetings. Moreover, in other ICU settings, family meetings have clear problems with missed opportunities for shared decision-making,7,9–11 with physicians talking the majority of time,7,11 nurses feeling unwelcome to participate,12 teams failing to check families’ understanding of the prognostic information provided,13 and inadequately listening to families and acknowledging their emotions.10 To date, little data exist in the pediatric CICU for how family meetings are conducted and what different interprofessional team members contribute to the discussion.
We therefore conducted a prospective observational study of family meetings in the pediatric CICU, aiming to quantitatively and qualitatively assess the conversation contributions made by team members when in communicating with parents during family meetings.
Methods
The Children’s Hospital of Philadelphia’s (CHOP) Institutional Review Board approved this prospective observational study, which was conducted in CHOP’s CICU between March and June 2016. CHOP’s CICU is a 26-bed ICU that has approximately 1000 admissions per year, with 11 intensivists, seven nurse practitioners, 127 nurses, and two social workers.
Subjects
Subjects were members of the interprofessional team attending pediatric CICU weekly family meetings for patients admitted to the CICU longer than two weeks. One new patient who has been hospitalized for at least two weeks was elected by the clinical group for a family meeting each week. Any clinician on the team could nominate a patient. Clinicians reported that they would nominate patients who did not have a clear discharge plan in the next few days or who had medical uncertainty leading to challenges in care planning. The goal of the family meetings was to update the family about the patient’s ICU course and address questions or concerns; although the conversations may have included bad news, they were not discussions of foregoing life-sustaining treatment. The interprofessional team, including all CICU attendings, nursing, social work, dietitians, physical and occupational therapists, and relevant subspecialists, was invited to meet and prepare before the family meeting.
Subjects completed surveys providing their demographic information, professional role on the team, years in practice, and average number of family meetings attended each week (0, 1, 2–4, or >5). Parents gave permission for the recording but were not considered subjects of the study.
Analysis
We audio-recorded family meetings and imported the recordings into NVivo 11. A research assistant was present in the room during the discussion to accurately identify and log who was speaking. In the first round of quantitative coding, the research assistant used NVivo and the notes from the meeting to attribute all clearly spoken utterances to the clinical team members and family members. We used quantitative conversation attribution and coding to determine the percentage that members of each professional group spoke during each meeting (speaking percentages do not equal 100% as a result of silences and instances when members of each group spoke at the same time). The timing of when different professionals spoke during the meeting was also determined via examination of conversation attribution using NVivo.
Before further quantitative coding, audio recordings were transcribed. All coding was completed by two authors (E. S. and T. E. S.) after they trained on the codebooks using a nonanalyzed family meeting. The Kappa statistic for the codes across all meetings averaged 0.85 (median 0.88; range 0.66–1.00). The Studying Communication in Oncologist-Patient Encounters (SCOPE) codebook14 was used to evaluate communication behaviors between the team and family. We analyzed the data for a quantitative count of the number of instances that each of the following behaviors occurred: elicitation of parental concerns, assessment of parental understanding, asking how much information they want to know, closed- and open-ended questions, and empathic or inappropriate responses to empathic opportunities (Table 1).
Table 1.
Codebook and Exemplar Quotes
| Code | Definition | Exemplar Quote |
|---|---|---|
| Elicitation of parental concerns | Medical team attempt to bring up topics of parental concern, worries, or fears | “What are you worried about?” (CICU Physician) |
| Assessment of parental understanding | Medical team attempt to clarify or confirm parental knowledge of disease and treatment | “Tell me what you understand about your child’s illness?” (CICU Physician) |
| Asking parent(s) how much information they want to know | Medical team attempt to find out how much information a parent wants to know about a given topic | “I have the results from the last imaging; how much detail would you like me to go into?” (CICU Physician) |
| Closed-ended question | Question that can be answered with a “yes” or “no” | “Does all of this make sense to you so far?” (CICU Physician) |
| Open-ended question | Question that allows a wide range of possible answers | “What questions do you have for me?” (CICU Physician) |
| Empathic opportunity | Parent explicitly or implicitly expresses emotion | “I’s definitely scary [to hold my baby].” (Parent) |
| Empathic terminator | In response to an empathic opportunity, the medical team changes the topic, makes a joke, denies the paren’s emotion, or ends the conversation (Active response; does not include nonresponse) | “I’m just kind of like nervous now about Friday, I’m like ’AHH!!’ you know, but we’ll figure it out.” (Parent) |
| “No, it’ll be some good data I think that will help everybody make some decisions.” (CICU Physician) | ||
| Empathic response to empathic opportunity | Medical team uses an “I wish” statement; names paren’s emotion; shows understanding of paren’s emotion; communicates respect or praise; shows support; or explores paren’s emotion | “I’s hard. A lot of people don’ realize that babies are born with any problems, let alone a complex heart problem that needs some time to figure out.” (Nurse Manager) |
| Team elicits questions from family | Team asks whether the parent has a question or indicates an openness to answering questions | “Any questions so far?” (CICU Physician) |
| Parent asks a question of the medical team | Question asked by parent | “So if they find that out, are they still going to do the bronchoscopy?” (Parent) |
| Discussion of medical information | All medical details pertaining to the patien’s current acute illness, including symptoms and prognosis, as well as chronic and past medical conditions, treatments, family medical history, and health screening | “There have been times when she’s collapsed part of the left lung, as well.” (CICU Physician) |
| Rapport building | Use of casual humor or kindness to put parents at ease | “The nurses love [your son.] They fight over [your son]! [Laughter]” (Nurse Manager) |
| Encouraging family involvement in care | Team encourages parents or other family members to be more involved in (medical or overall) care of the patient | “Do you feel comfortable with the nursing care and working with the nurses to care for the baby? Cause we want to get you to do more of her care …” (Social Worker) |
| Clarifying procedures and processes of communication | Explanation of who to contact and/or how to contact them in the event of conflict or confusion; or the hierarchy of staff in the CICU and how to interact with it | “Everyday, 24/7, there’s a charge nurse, so if you feel like you need to speak to someone besides the bedside nurse there’s a charge nurse here all the time. And then during the day, during the week, there’s usually someone here from leadership if you want to talk to someone.” (Nurse Manager) |
| Addressing parental needs and resources | Comments or questions about the logistics or psychosocial complexity of the parent/family’s current situation or future needs | “Are you guys still okay staying at the hotel? I know we spoke early on about the Ronald McDonald house.” (Social Worker) |
| Facilitation of meeting discussion | Team member begins meeting, plans future discussion, or prompts other team members to speak | “Did you want to talk about early intervention?” (Social Worker) |
We also coded the number of instances that each of the following family meeting best practices for promoting shared decision-making occurred10,15–17: sharing medical information with families, eliciting their questions, and attending to their concerns (Table 1).
Finally, a qualitative analysis was done of nurses’ and social workers’ contributions to identify themes not captured by the quantitative codes. Using a content codes approach, two coders (J. K. W. and T. E. S.) developed a codebook and coded the transcripts using a consensus method for any disagreements.
Results
Subjects
Each of the 10 meetings had at least one CICU intensivist, social worker, and nurse, with four clinicians present on average and a range of three to six clinicians per meeting. A total of 28 different clinicians (Table 2) attended at least one meeting with five clinicians attending two meetings, one clinician attending three meetings, and two social workers each attending four or more meetings. Team members who attended these meetings were predominantly female (82%), and one-third of them do not attend any family meetings in an average week on service (39.3%), whereas one-fourth of them attended 2–4 meetings per week. Half (50%) of the team members had six or more years of experience. Five meetings had one family member present, whereas another five had two family members present. One set of parents did not give permission for a recording to be made of their family’s meeting, so that meeting was not recorded. All team members provided consent for participation, allowing the recording of all other eligible meetings.
Table 2.
Clinician Participants in 10 Family Meetings
| Clinician Characteristics | Participants n = 28 Frequency (%) |
|---|---|
| Professional role | |
| Attending intensivist | 8 (28.6) |
| Cardiologist | 1 (3.6) |
| Subspecialist Attending | 3 (10.7) |
| Nurse practitioner | 4 (12.3) |
| Nurse manager | 5 (17.8) |
| Bedside nurse | 2 (7.1) |
| Social worker | 2 (7.1) |
| Interpreter | 3 (10.7) |
| Gender | |
| Male | 5 (17.8) |
| Female | 23 (82.1) |
| Race | |
| White | 12 (42.9) |
| Black or African American | 3 (10.7) |
| Other | 4 (14.2) |
| Missing | 9 (32.1) |
| Ethnicity | |
| Hispanic | 2 (7.1) |
| Non-Hispanic | 17 (60.7) |
| Missing | 9 (32.1) |
| Years working in field | |
| Less than 1 | 0 |
| 2–5 years | 5 (17.9) |
| 6–10 years | 8 (28.6) |
| >10 years | 6 (21.4) |
| Missing | 9 (32.1) |
| Average family meetings attended per week | |
| None | 11 (39.3) |
| 1 | 1 (3.6) |
| 2–4 | 7 (25) |
| More than 5 | 0 |
| Missing | 9 (32.1) |
Meeting Characteristics
All 10 meetings included provision of medical information, with two meetings including the delivery of serious news. The two meetings discussing serious news did not vary consistently in any relevant characteristics. There was discussion of future management and what would need to occur for discharge from the ICU in eight meetings. Meeting duration averaged 34 minutes with a range of 17 to 64 minutes. All the meetings were led by the CICU attending physician.
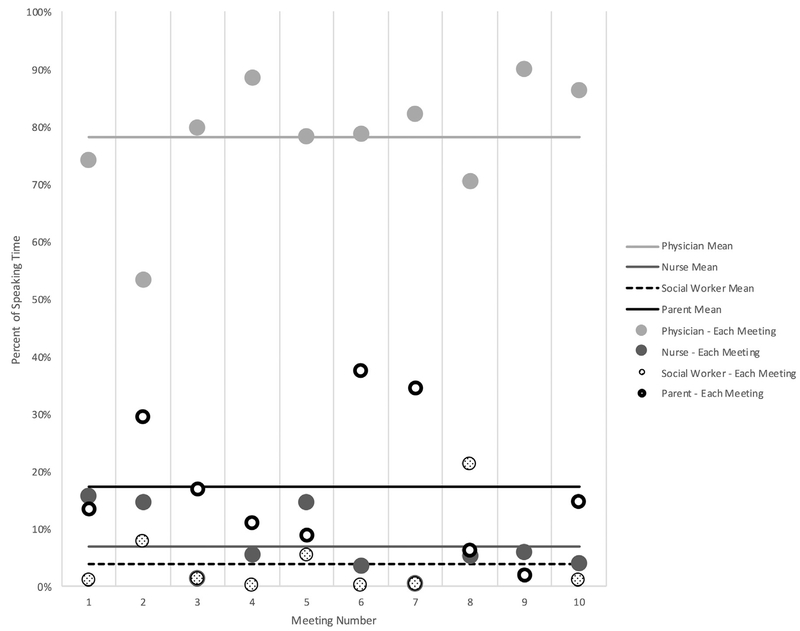
Comparison of Speaking Time by Profession
Physicians spoke for an average of 78.1% of each meeting (median 79.2%; SD 10.7%), social workers for an average of 3.9% (median 1.1%; SD 6.5%), and nurses for an average of 7.0% (median 5.4%; SD 5.7%). Parents spoke for an average of 17.4% of each meeting (median 14%; SD 12.2%) (Figure 1).
Fig. 1.
Percentage of speaking time by participant category.
Distribution of Professionals’ Contributions
In eight of 10 meetings, there were two phases of the conversation defined by who contributed to the conversation. The first phase of the conversation was almost exclusively between physicians and parents, lasting an average of 69.8% (SD: 18.4%) of the total meeting. In a second phase, nonphysician contributions were added after the physician indicated they had concluded their contributions. One example of the transition occurred when a CICU attending stated: “I believe that was really all that … we had discussed and talked about. [Nurse manager] anything else?” In two of the 10 meetings, nurses offered medical contributions during the physician-dominated portion without an explicit invitation by the physician. One example of a nurse contributing to a conversation occurred as follows:
Physician: You’re okay?
Parent: Mm-hmm.
Physician: Okay.
Nurse: Do you have any questions for us related to his care or his recovery or things that have been going on?
Discussion of Medical Information by Profession
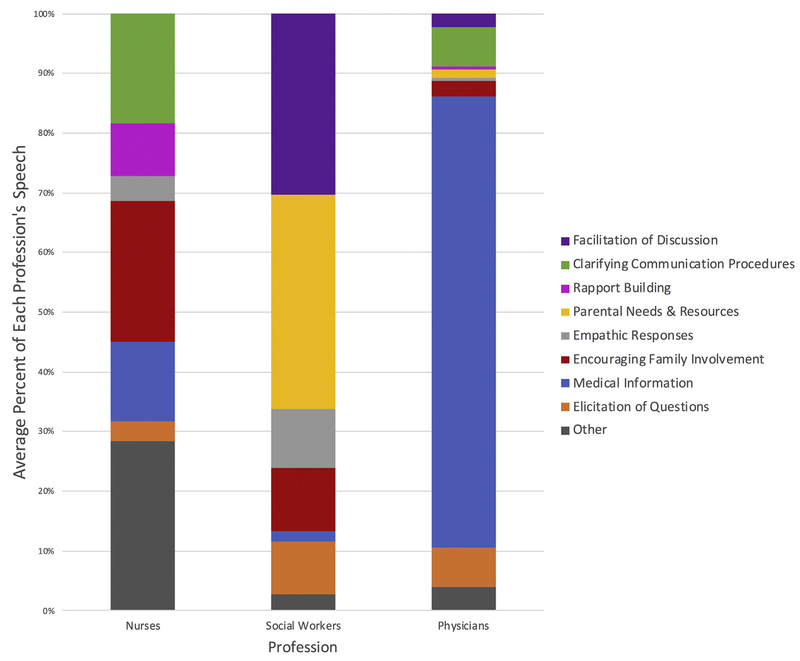
On average, 75.6% (SD 8.5%) of physicians’ total contributions were a discussion of medical information about the patient’s condition(s), treatments, and tests; 13.3% (SD 18.1%) of nurses’ total contributions provided medical information and consisted largely of clarifying statements of physician colleagues. On average, less than 2% (SD 3.7%) of social workers’ total contributions were about medical information. One example occurred when a social worker asked about the parents need for more information: “I know your first question before we started was about eating, so you understand about the feeding tube, or do you have more questions about what that looks like?”
Assessment of Parental Information and Elicitation of Concerns and Questions
Parents were asked how much information they wanted in only one of 10 meetings. Parental understanding was assessed once at the beginning of two meetings by CICU attendings; in no meeting was this assessed at the end of the meeting. On average, the team elicited parental concerns or worries 0.6 times per meeting (SD 1.3) (Table 3). One example of an elicitation of parental concerns was given by the physician: “So before I get started into what we already talked about, are there any specific things that you want to make sure we address today? Any specific problems or concerns that you have?” Social workers elicited parental concerns 0.4 times per meeting (SD 1.3), and physicians elicited parental concerns 0.2 times per meeting (SD 0.6), whereas nurses did not make elicitations.
Table 3.
Communication Behaviors in Family Meetings in the CICU (Measured by Frequency per Meeting)a
| Variable | Mean | Median | SD | Range |
|---|---|---|---|---|
| Elicitation of parental concerns | 0.6 | 0 | 1.3 | 0–4 |
| Assessment of parental understanding | 0.2 | 0 | 0.4 | 0–2 |
| Asking parent(s) how much information they want to know | 0.1 | 0 | 0.3 | 0–1 |
| Closed-ended question | 12.2 | 9.5 | 10.2 | 0–26 |
| Open-ended question | 1.7 | 0 | 2.5 | 0–7 |
| Empathic opportunity | 4.2 | 1.5 | 7.1 | 0–23 |
| Empathic terminator | 0.7 | 0 | 1.3 | 0–4 |
| Empathic response to empathic opportunity | 2.2 | 1 | 4.3 | 0–14 |
| Team elicits questions from family | 6.2 | 6 | 4.6 | 0–13 |
| Parent asks a question of the medical team | 6.3 | 5 | 4.9 | 1–16 |
| Rapport building | 3.4 | 1.5 | 5.8 | 0–19 |
| Encouraging family involvement in care | 2.6 | 0 | 4.3 | 0–13 |
| Clarifying procedures and processes of communication | 0.6 | 0 | 1.1 | 0–3 |
| Addressing parental needs and resources | 1.9 | 0 | 2.7 | 0–7 |
| Facilitation of meeting discussion | 2.4 | 0 | 6.3 | 0–20 |
The “medical information” code is not included in this table because the bulk of each meeting was discussion of medical information. See Figure 2 for proportion of speech consisting of medical information by profession.
Team members elicited questions from parents an average of 6.2 times per meeting (SD 4.6; range 0–13 times) (Table 3). This category is distinct from the elicitation of worries because it includes any time a parent was asked if they had questions or expressed an openness by the team to answer questions. Elicitation of questions was further broken down into two subtypes: closed-ended questions, in which the only possible response was “yes” or “no,” and open-ended questions, which gave parents the opportunity for a longer response (i.e., to express any questions, thoughts, or concerns on their mind). Clinicians asked parents an average of 12.2 (SD 10.2) closed-ended questions, such as “Does that make sense?” and an average of 1.7 (SD 2.5) open-ended questions, such as “What questions do you have about that?” per meeting. Parents asked an average of 6.3 questions (SD 4.9; range 1–16 questions) per meeting. Physicians elicited questions most frequently, with an average of 4.6 elicitations per meeting (SD 4.2), which averaged 6.7% (SD 7.6%) of physicians’ total contributions; followed by social workers at 0.8 per meeting (SD 2.2), which averaged 8.9% (SD 18.2%) of social workers’ total contributions; and nurses at 0.7 per meeting (SD 0.7), which averaged 3.4% (SD 5.2%) of nurses’ total contributions (Figure 2).
Fig. 2.
Proportion of most common contributions by profession.
Responses to Parental Emotion
Parents displayed emotion, creating an opportunity for an empathic response, an average of 4.2 times per meeting (SD 7.1) (Table 3). The clinical team responded empathetically an average of 2.2 times per meeting (SD 4.3) and either failed to respond or responded inappropriately (by joking, changing the topic, denying the parental emotion, or ending the discussion) to the remainder of empathic opportunities. An example of an empathic response to an empathic opportunity occurred as follows:
Parent [crying]: It’s been a lot.
Attending Physician: This is hard.
Nurse: You have been such amazing advocates for him.
Although CICU attendings had the highest number of expressions of empathy, with an average of 1.3 per meeting (SD 2.8), these expressions averaged only 0.5% (SD 1.2%) of physicians’ total contributions (Figure 2). On the other hand, social workers averaged 0.3 (SD 0.5) expressions of empathy per meeting, but their expressions of empathy constituted 10% (SD 3.1%) of social workers’ total contributions, the highest percentage of any clinician. Nurses averaged 0.8 expressions of empathy per meeting (SD 1.9), which comprised an average of 4% (SD 8.1%) of nurses’ total contributions.
Analysis of Nonphysician Contributions
Themes arising from nurse contributions not already captured in the quantitative elements of the study included 1) rapport building (e.g., “My husband has red hair. I love the red heads!”), 2) encouraging family involvement in patient care (e.g., “Have you done any skin to skin? … it’s ok for you to ask to hold her and for you to say to your nurse in the morning, ‘I wanna hold her today.”’), and 3) clarifying procedures and processes of communication (e.g., “If you do ever have concerns or questions or anything, we have a very detailed, a big structure of nursing support, so your first, your first line of contact is your bedside nurse that you have for that shift.”). Rapport building comprised 9% of nurse total contributions, whereas encouraging parental involvement in patient care comprised 23.7%, and clarifying procedures and processes comprised 18.3% (Figure 2).
Themes arising from social work contributions included 1) addressing parental needs and resources (e.g., “I know we spoke early on about Ronald McDonald house and you wanted to hold off on that. Well that’s always still an option.”), 2) encouragement of family members’ involvement (e.g., “And at any point if you want [your other child] to be here and you want her to learn about the tubes and what she can and cannot touch … child life is the best resource for that.”), and 3) facilitating who speaks in the meeting (e.g., “So we’ll just go ahead and start with you.”). Addressing parental needs and resources comprised a total of 35.8% of social worker contributions, with encouragement of family members’ involvement in care comprising 10.5% and facilitation of discussion comprising 30.4%.
Discussion
This study, which examined the ways in which members of interprofessional teams communicate with each other and with families during family meetings in the pediatric CICU, had four significant findings. First, based on professional role, team members behaved quite distinctly in the meetings, offering different kinds of contributions. Second, physicians frequently controlled who spoke throughout the meeting and signaled to nonphysicians when they could join the conversation with families. Third, empathic responses, while higher than percentages reported in the adult literature,18,19 still occurred only 50% of the time, with all clinicians responding empathically rarely. Fourth, despite attempts at elicitation of questions, parents spoke a minority of the time, with infrequent assessments by clinical team members of the parents’ understanding of information shared by the team.
Team members’ distinct contributions in the meeting suggest that interprofessional team members attend to different aspects of care in family meetings. Although physicians predominantly offered medical information, nonphysician clinicians made important contributions to the meetings by encouraging parental involvement in patient care, addressing resource needs and other family member involvement. These contributions by nonphysicians were broader than those reported in the pediatric ICU literature, where 60% of observed nurses’ contributions were to clarify clinical information.12 In our study, nurses’ contributions were largely encouraging parental involvement and clarifying communication procedures, whereas social workers’ contributions primarily assessed parental needs and how to support the whole family, including siblings and grandparents. These distinct contributions are masked by most analyses of family meetings that either aggregate all clinician contributions10,11,20 or primarily focus on physician contributions.3,21,22,23 The distinct contributions by nonphysicians that our study identified can be used to underscore the importance of interprofessional staff in family meetings, especially, because there are many reported barriers to nurse attendance of these meetings.12 In addition, these distinctions in behaviors can be used to develop team processes that ensure that nonphysician contributions are given adequate time in family meetings. Team members could be trained in these processes so that, regardless of which individual is in the role of attending or social worker, all members understand the expectations for contributions in the meeting.
The extent to which physicians controlled communication in the meeting has implications for how the interprofessional team is able to function as a team. The high proportion of physician-speaking time compared with other clinicians and families is consistent with other research groups’ findings in meetings with adult patients24 and in the neonatal ICU21,25,26 and pediatric ICU.3,11 Our study, however, more granularly characterized the types of contributions made by different professionals within these meetings and when they occurred. Conversations were found to be primarily between the physicians and parents until the physician invited other clinicians to participate in the conversation, usually, because the physician has covered all the material they intended to discuss. The siloed nature of conversations has not been previously described in the literature and has implications for the ways in which team members support each other and work in concert with one another. Many discussions of teamwork encourage characteristics like backup behavior, which allows for a team member to step in and complete a task if they perceive it has not been done successfully.27 If social norms on a team do not allow for a nonphysician to engage in the conversation until signaled by the physician, it may limit the ability of the team to use its full complement of skills to ensure parents understand all the information and have their expressions of emotion appropriately attended to. Further research of how high-functioning teams engage throughout conversations with families is warranted to determine best practices.
Our third major finding, namely that all clinician responses to parental emotion were inconsistent, leaving half of empathic opportunities inappropriately acknowledged, has clinical implications. The team’s ability to respond to emotion is particularly salient in ICUs, where parents experience significant stress and anxiety,28 which may impair their ability to assimilate new information if not acknowledged and addressed.29 Although social workers had the highest proportion of empathic responses at 10% of their contributions, followed by nurses at 4%, these empathic responses were still a minority of their overall contributions. An increasing emphasis has been placed on training physicians in explicit expressions of empathy given their lack of formal communication skills training,30 but our findings raise questions of whether other professionals may also need formal training in responding to emotion as well. Further investigation should determine whether nonphysicians do not feel empowered to respond to emotion before a physician’s invitation to participate in the conversation or if they, like physicians, would benefit from more formal communication skills training.
Similarly, our fourth finding that parents’ participation in meetings was limited, and little was done by the clinical team to assess the parents’ understanding of the large amounts of medical information shared with them, also has clinical implications. Similar to what has been described in the adult ICU,13 parents of pediatric patients received information without an assessment of how much or what kind of information they wanted. Best practice in communication encourages asking parents how much information they want to know31 because disclosure of serious illness or discussion of death for patients and families from a variety of cultures may be viewed as disrespectful, impolite, or even harmful.32 Also, families’ ability to absorb prognostic information provided in different formats, even within one family, varies.33 Assuming all parents want the same amount and kind of information may substantially contribute to their misunderstanding of the information provided.
Parents’ participation in the meetings was also highly variable—there were several meetings in which they spoke little, despite some attempts to ask them questions. Parental involvement in these conversations may depend on parent characteristics, such as their self-efficacy,34 experience with navigating discussions with the health care team, and team skill in eliciting their questions. Parents with low health literacy or less education are less likely to voice their concerns unless teams elicit them.35 Given evidence that physicians provide more detailed information when prompted by patients and their families,36 families who ask fewer questions may also receive less information needed to make decisions. Clinician communication practices should anticipate parents with varying levels of self-efficacy and health literacy to ensure processes are in place to meet all parents’ decision support needs, regardless of their individual skill levels. In addition, although we did not assess parental satisfaction with these conversations, other pediatric data have drawn associations between more parent-centered conversations and higher parent satisfaction.7
Limitations
This study has several limitations. First, we do not know how our findings would relate to the perceptions of the family or team because we did not assess their perceptions. Although the team may not have used some of the elements of best practice, this does not mean that families were dissatisfied with the information they received and the decision-making practice. Second, this study included a small sample size of 10 family meetings in the pediatric CICU, so these results may not be generalizable to other family meetings, particularly in other units. Third, this study was limited to verbal communication via audio recordings. Important nonverbal communication themes, particularly in terms of support offered to families, may have been missed and should be explored in future studies. Fourth, interpretation of these findings should be done in the context of the type of family meetings that were recorded: the meetings covered different kinds of parental and medical concerns and did not all require a decision to be made. The practice of pre-emptively meeting with families of long-stay patients may mean that families had either a variety of or no pressing questions/concerns that they needed addressed.
Conclusion
Doubt is warranted regarding whether the goals of interprofessional teamwork are achieved in family meetings when physicians dominate control of the conversation while also missing opportunities to assess parental understanding and respond to parental emotion. The identification of communication and teamwork behaviors in family meetings provides important information for interprofessional teams interested in improving communication during these meetings. Future studies are needed to demonstrate whether a communication skills training intervention for interprofessional teams will improve team collaboration and communication with families, including response to emotion and elicitation of parental understanding and concerns.
Disclosures and Acknowledgments
This work was supported by a Cambia Foundation Sojourns Scholar Award, the Children's Hospital of Philadelphia Department of Pediatrics Academic Enrichment Fund, and the National Heart, Lung, And Blood Institute of the National Institutes of Health under Award Number K23HL141700. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
References
- 1.Hexem KR, Mollen CJ, Carroll K, Lanctot DA, Feudtner C. How parents of children receiving pediatric palliative care use relgion, spirituality, or life philosophy in tough times. J Pallliative Med 2011;14:39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mack JW, Wolfe J, Grier HE, Cleary PD, Weeks JC. Communication about prognosis between parents and physicians of children with cancer: parent preferences and the impact of prognostic information. J Clin Oncol 2006;24: 5265–5270. [DOI] [PubMed] [Google Scholar]
- 3.Maurer SH, Hinds PS, Spunt SL, Furman WL, Kane JR, Baker JN. Decision making by parents of children with incurable cancer who opt for enrollment on a phase I trial compared with choosing a do not resuscitate/terminal care option. J Clin Oncol 2010;28:3292–3298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Tomlinson D, Bartels U, Hendershot E, Maloney AM, Ethier MC, Sung L. Factors affecting treatment choices in paediatric palliative care: comparing parents and health professionals. Eur J Cancer 2011;47:2182–2187. [DOI] [PubMed] [Google Scholar]
- 5.Blume E, Balkin E, Aiyagari R, et al. Parental perspectives on suffering and quality of life at end-of-life in children with advanced heart disease: an exploratory study. Pediatr Crit Care Med 2014;15:336–342. [DOI] [PubMed] [Google Scholar]
- 6.Rosenberg A, Orellana L, Kang T, et al. Differences in parent-provider concordance regarding prognosis and goals of care among children with advanced cancer. J Clin Oncol 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.October T, Wang J, Roter D. Parent satisfaction with communication is associated with physician’s patient-centered communication patterns during family conferences. Pediatr Crit Care Med 2016;17:490–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Davidson JE, Aslakson RA, Long AC, et al. Guidelines for family-centered care in the neonatal, pediatric, and adult ICU. Crit Care Med 2017;45:103–128. [DOI] [PubMed] [Google Scholar]
- 9.Institute of Medicine. Dying in America: Improving Quality and Honoring Individual Preferences Near the End of Life. Washington, D.C: Institute of Medicine, 2014. [Google Scholar]
- 10.Curtis JR, Engelberg RA, Wenrich MD, Shannon SE, Treece PD, Rubenfeld GD. Missed opportunities during family conferences about end-of-life care in the intensive care unit. Am J Respir Crit Care Med 2005;171:844–849. [DOI] [PubMed] [Google Scholar]
- 11.Michelson K, Clayman ML, Ryan C, Emanuel L, Frader J. Communication during pediatric intensive care unit family conferences: a pilot study of content, communication, and parent perceptions. Health Commun 2017;32: 1225–1232. [DOI] [PubMed] [Google Scholar]
- 12.Watson AC, October TW. Clinical nurse participation at family conferences in the pediatric intensive care unit. Am J Crit Care 2016;25:489–497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. The language of prognostication in intensive care units. Med Decis Making 2010;30:76–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koropchak C, Pollak KI, Arnold RM, et al. Studying communication in oncologist-patient encounters: the SCOPE Trial. Palliat Med 2006;20:813–819. [DOI] [PubMed] [Google Scholar]
- 15.McFarlin J, Tulsky JA, Back AL, Arnold RM. A talking Map for family meetings in the intensive care Unit. JCOM 2017;24. [Google Scholar]
- 16.Wood GJ, Chaitin E, Arnold RM. Communication in the ICU: Holding a family meeting. UpToDate, 2017. [Google Scholar]
- 17.Michelson KN, Clayman ML, Haber-Barker N, et al. The use of family conferences in the pediatric intensive care unit. J Palliat Med 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kennifer SL, Alexander SC, Pollark KI, et al. Negative emotions in cancer care: do Oncologists’Responses depend on severity and type of emotion? Patient Educ Couns 2009; 76:51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pollak KI, Arnold RM, Jeffreys AS, et al. Oncologist communication about emotion during visits with patients with advanced cancer. J Clin Oncol 2007;25:5748–5752. [DOI] [PubMed] [Google Scholar]
- 20.Stapleton RD, Engelberg RA, Wenrich MD, Goss CH, Curtis JR. Clinician statements and family satisfaction with family conferences in the intensive care unit*. Crit Care Med 2006;34:1679–1685. [DOI] [PubMed] [Google Scholar]
- 21.Boss RD, Donohue PK, Larson SM, Arnold RM, Roter DL. Family conferences in the neonatal ICU: observation of communication dynamics and contributions. Pediatr Crit Care Med 2016;17:223–230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.October TW, Watson AC, Hinds PS. Characteristics of family conferences at the bedside versus the conference room in pediatric critical care. Pediatr Crit Care Med 2013;14. [DOI] [PubMed] [Google Scholar]
- 23.White DB, Engelberg RA, Wenrich MD, Lo B, Curtis JR. Prognostication during physician-family discussions about limiting life support in intensive care units. Crit Care Med 2007;35:442–448. [DOI] [PubMed] [Google Scholar]
- 24.McDonagh JR, Elliott TB, Engelberg RA, et al. Family satisfaction with family conferences about end-of-life care in the intensive care unit: increased proportion of family speech is associated with increased satisfaction. Crit Care Med 2004;32:1484–1488. [DOI] [PubMed] [Google Scholar]
- 25.Boss RD, Donohue PK, Roter DL, Larson SM, Arnold RM. “This is a decision you have to make”: using simulation to study prenatal counseling. Simul Healthc 2012;7:207–212. [DOI] [PubMed] [Google Scholar]
- 26.Lamiani G, Meyer E, Browning DM, Brodsky D. Analysis of enacted difficult conversations in neonatal intensive care. J Perinatal 2009;29:310–316. [DOI] [PubMed] [Google Scholar]
- 27.Baker DP, Day R, Salas E. Teamwork as an essential component of high-reliability organizations. Health Serv Res 2006;41(4 Pt 2):1576–1598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Balluffi A, Kassam-Adams N, Kazak A, Tucker M, Dominguez T, Helfaer M. Traumatic stress in parents of children admitted to the pediatric intensive care unit. Pediatr Crit Care Med 2004;5:547–553. [DOI] [PubMed] [Google Scholar]
- 29.Pochard F, Azoulay E, Chevret S, et al. Symptoms of anxiety and depression in family members of intensive care unit patients before discharge or death. A prospective multicenter study. J Crit Care 2005;20:90–96. [DOI] [PubMed] [Google Scholar]
- 30.Visser M, Deliens L, Houttekier D. Physician-related barriers to communication and patient- and family-centred decision-making towards the end of life in intensive care: a systematic review. Crit Care 2014;18:604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.The Hospital of Sick Kids, Cultural Competence Train-the-Trainer Manual. Toronto, Canada: The University of Toronto, 2011:1–382. [Google Scholar]
- 32.Searight HR, Gafford J. Cultural diversity at the end of life: issues and guidelines for family physicians. Am Fam Physician 2005;71:515–522. [PubMed] [Google Scholar]
- 33.Boss RD, Lemmon ME, Arnold RM, Donohue PK. Communicating prognosis with parents of critically ill infants: direct observation of clinician behaviors. J Perinatol 2017;37:1224–1229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Maly RC, Umezawa Y, Leake B, Silliman RA. Determinants of participation in treatment decision-making by older breast cancer patients. Breast Cancer Res Treat 2004;85: 201–209. [DOI] [PubMed] [Google Scholar]
- 35.Anderson WG, Arnold RM, Angus DC, Bryce CL. Passive decision-making preferences is associated with anxiety and depression in relatives of patients in the intensive care unit. J Crit Care 2009;24:249–254. [DOI] [PubMed] [Google Scholar]
- 36.Cegala D, Chisolm D, Nwomeh B. Further examination of the impact of patient participation on physicians’ communication style. Patient Educ Couns 2012; 89:25–30. [DOI] [PubMed] [Google Scholar]