Figure 3. A need for pain biomarkers:
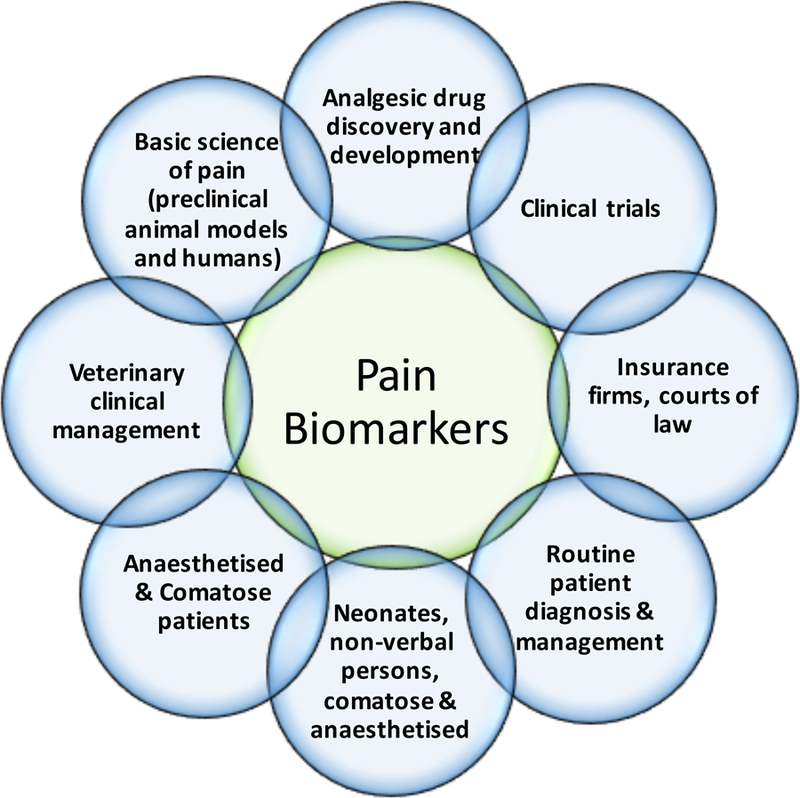
There are numerous situations that would benefit from the availability of specific, sensitive and accurate biomarkers for pain. Each of these are in themselves complex areas of biological science and medicine that require different combinations of the features of biomarkers listed in Table 1 relative to each other. For example, while routine patient management would benefit from use of safety and monitoring biomarkers, it would arguably be of greater benefit for non-verbal patients and neonates for a pharmacodynamic response biomarker. The consequences of false negative findings from a pain biomarker, include: (1) trust issues between doctor-patient, employee-patient or family-patient; (2) denial of medical treatment; (3) mental health, stress, spousal/family issues; (4) financial/insurance and employment issues; (5) privacy/legal (medical malpractice issues). The consequences of false positive findings, include: (1) unnecessary, costly, harmful analgesic treatment in non-communicative patients; (2) human, infrastructure, financial and time resources; (3) misunderstanding as a substitute for self-report. These are serious issues to be considered in the development of any pain biomarker, as has been discussed (Davis et al., 2017).
