Abstract
Objective:
Performance on pediatric quality measures varies across primary care practices. Healthcare quality is associated with organizational factors, but their effect is understudied in pediatric care. This study aimed to develop hypotheses regarding the relationship between organizational factors and composite scores on pediatric quality measures.
Methods:
Using a positive deviance approach, semi-structured interviews were conducted with pediatricians and staff (n=35) at 10 purposively selected high-performing pediatric primary care practices in Massachusetts between September and December 2016. Practices were sampled to achieve diversity in geographic location, size, and organizational structure. Interviews aimed to identify organizational strategies (e.g., care processes) and contextual factors (e.g., teamwork) that may be associated with performance on quality measures. Interviews were audiotaped, transcribed, and analyzed using qualitative content analytic methods.
Results:
We identified four major themes (MT): MT1) Practice Culture; MT2) Practice Structures and Quality Improvement Tools; MT3) Attitudes and Beliefs Related to Measuring Care Quality; and MT4) Perceived Barriers to Achieving High Performance on Quality Measures. MT1 sub-themes included contextual factors such as teamwork, leadership, and feeling respected as an employee; MT2 subthemes included fixed characteristics such as practice size and strategies such as use of an electronic medical record; MT3 and MT4 subthemes linked these constructs to factors external to the practices.
Conclusions:
This study suggested that elements of organizational culture may play as important a role in the quality of care delivered as specific quality improvement strategies. Interventions to further test this relationship may aid practices seeking to improve the care they deliver.
Keywords: pediatric healthcare quality, qualitative, positive deviance, organizational studies
Introduction
A landmark study of 12 urban pediatric primary care practices found that less than half of the 1,536 children studied received indicated care.1 Over the past decade, other studies of pediatric care quality have continued to demonstrate deficits in quality of care for children with specific diseases (e.g., asthma, autism, and special health care needs)2–4 and inequities in quality of care for children from vulnerable populations (e.g., racial/ethnic minority and limited English proficiency).5–8 Health systems, payers, and policy-makers have worked to address this issue through interventions such as the patient- centered medical home (PCMH),9 learning collaboratives, and pay-for-performance stratgeies.10,11 Despite these and other interventions, quality of care remains sub-optimal for many children.12–15
Although problems with pediatric quality of care are well-described, there is little empirical evidence to explain why issues with quality of care persist. Organizational strategies (e.g., use of technology, staffing) and contextual factors (e.g., work culture, leadership) have emerged as potential explanatory factors as to why efforts to address care quality might be effective in some settings but not in others.16–18 Physicians, staff, and parents of children with special healthcare needs at 12 high performing practices (Medical Home Index19 scores) identified a culture of quality improvement (QI), family-centered care with parents as improvement partners, team-based care, and care coordination as organizational drivers of care improvements. These practices were part of a large QI learning collaborative sponsored by the Center for Medical Home Improvement and the National Initiative for Children’s Healthcare; the focus was on children with special healthcare needs.20 Less is known about which organizational factors may be associated with quality of care for the general pediatric population. We aimed to begin address this gap in knowledge by interviewing key informants at a sample of high-performing pediatric practices in Massachusetts to gain their perspectives on organizational strategies and contextual factors that might drive performance on primary care pediatric quality measures.
Methods
Study Design
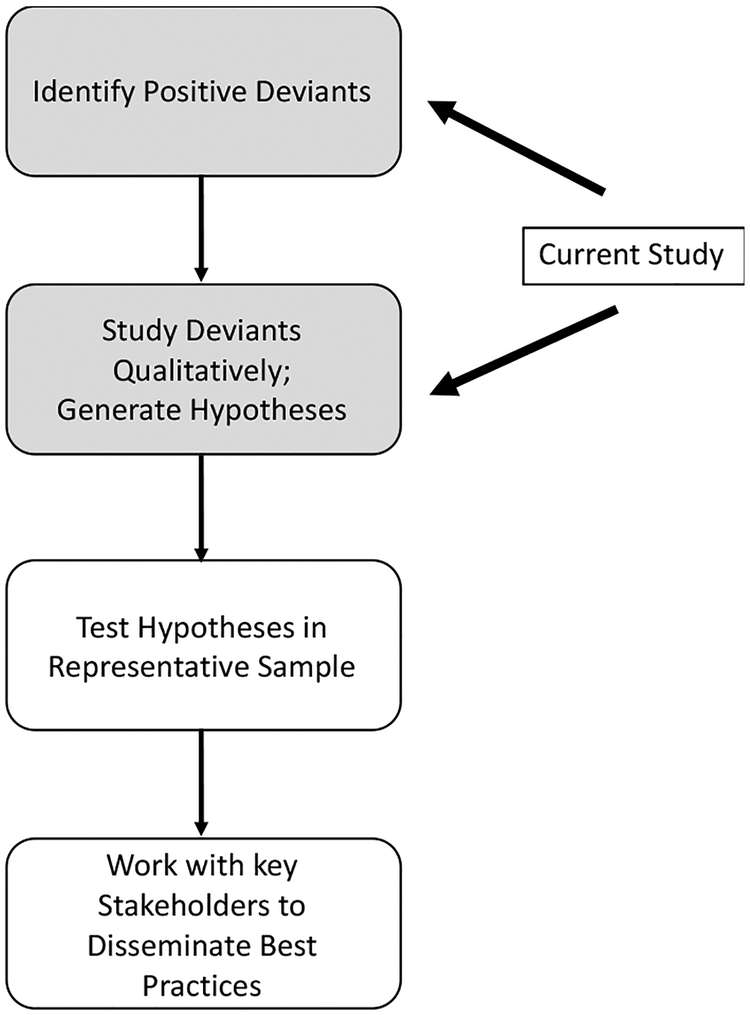
This qualitative study was the first phase of a positive deviance study aimed at identifying organizational factors associated with high composite clinical quality and patient experience scores (Figure 1). Positive deviance studies seek to identify strategies and contextual factors that enable individuals or groups to achieve better outcomes than similar groups with similar resources by studying positive outliers (“deviants”).21 This approach has been used to identify organizational factors associated with better performance on evidence based processes of care22 such as door-to-balloon time for patients with acute myocardial infarction.23
Figure 1.
Positive Deviance
Sample
First, we created composite clinical quality and patient experience scores for pediatric practices in Massachusetts using data obtained from Massachusetts Health Quality Partners (MHQP), a non-profit organization that partners with patients, physicians, healthcare organizations and payers to improve quality of care and patient experience.24 MHQP uses data from five of the largest commercial health insurance companies in Massachusetts to assess practices’ performance on eight common Healthcare Effectiveness Data and Information Set (HEDIS) measures. MHQP also administers a 55-item periodic patient/parent experience survey based on the Ambulatory Care Experience Survey and the Consumer Assessment of Healthcare Providers and Systems Survey.25 The response rate for the survey has ranged between 19.0% and 20.0%, similar to other large patient experience surveys.26 Two-hundred-twenty-seven practices had a score for at least one of the eight HEDIS measures reported by MHQP’ of these 182 (80.2%) had had scores for at least four measures. Thus, we created composite clinical quality scores for each of these 182 practices to balance achieving an adequate sample size and to include at least half of the measures reported by MHQP. Composite scores were used in this case as an indicator of a latent practice characteristic;27 we elected to include clinical quality and patient experience scores because different organizational strategies and contextual factors may be related to these two constructs. hree of the measures were for the conditions that occur with the greatest frequency in general pediatric practice: 1) well visits for children age 0–15 months or 3–5 years; 2) correct testing for strep throat; and 3) correct antibiotic use for upper respiratory infections. The fourth quality measure selected for a practice was the next measure with the most eligible patients at that practice. The composite score was calculated as the ratio of the sum of the number of patients receiving appropriate care (numerators) to the sum of the number of patients eligible for the measure (denominators). Composite clinical quality scores ranged from 0.57–0.97, indicating that there was sufficient variation in quality for a designation of “top performer” to be meaningful.
For patient experience measures, 162 of the 227 (71.4%) practices had received patient experience scores. We created a composite score for patient experience by determining the percentage of survey respondents in each practice that gave the practice the highest rating for each of the eight patient experience measures (“top box”). Practices’ composite patient experience scores ranged from 0.78–0.97.
We purposively recruited practices scoring in the top quartile for composite clinical quality and/or patient experience scores to achieve variation in geographical location in the state, practice size (number of providers), and organization type (private, multi-specialty organization, academic). We chose the top quartile as a cutoff to sample the highest performers while achieving variation in practice characteristics. We mailed an invitation to the practice owner or the practice manager (practice contact). After mailing the letters, we called practices to ascertain whether the letters were received, to answer questions, and to schedule interviews for interested practices. Practices were offered the choice of a $100 gift card for the practice or lunch for informants.
Interviews at High-Performing Practices
Each practice contact was asked to identify key informants and informants were asked at the time of our interviews if anyone else in the practice should be interviewed. Although we suggested that practice managers, pediatricians, front desk staff, nurses, and medical assistants be included, we ultimately let practices decide because of the differences in how practices structure job responsibilities. The first author (SG) conducted the interviews using a pre-tested interview guide. The guide consisted of open- ended questions and probes about why informants thought their practice scored higher than others on quality measures, what specific strategies they used to improve clinical quality and parent/patient experience, thoughts about quality measures, and what factors outside the practice might affect a practice’s quality scores. Some practices only agreed to consider participating if they could first see the interview questions, so the guide was e-mailed or mailed to all practice contacts with a copy of the study fact sheet prior to the interview. Interviews were conducted individually or in small groups to accommodate practices’ work flows and preferences. Interviews lasted 30–90 minutes, were digitally recorded, and transcribed verbatim by a trained transcriptionist; field notes were taken by a research assistant. Informed consent was obtained prior to conducting the interviews; Baystate Medical Center’s Institutional Review Board approved the study.
Analysis
We analyzed interview data following qualitative content analysis principles28 using Dedoose29 qualitative software. The lead author (SG) developed a provisional codebook after performing open line coding30 on the first three transcripts. KM read three subsequent transcripts and made recommendations for revisions of the provisional codebook. Open coding of transcripts proceeded in an iterative process with SG and a research assistant coding each transcript independently, discussing code choices, and using consensus to decide upon final codes; coding decisions were recorded in an “audit trail”. Coding agreement reached 85%. Concepts identified during open coding were then organized into broader themes and sub-themes. Practices were enrolled until theoretical saturation was achieved (no new concepts introduced in three consecutive interviews).31
Results
A total of 35 key informants were interviewed at 10 practices; interviews were conducted in person for seven practices and by phone for three. Characteristics of practices and key informants are summarized in Table 1. Race and ethnicity data and insurance case-mix were not available. Two of the practices were in the top quartile for composite clinical quality scores, four for composite patient experience scores, and four for both composite clinical quality and patient experience scores. The number of key informants per practice ranged from 1 to 6. Interpretation of the data was checked by mailing a summary of our analysis to participating practices and requesting feedback.
Table 1:
Practice and Participant Characteristics
| Characteristic | n |
|---|---|
| Practices (n=10) | |
| Region | |
| Western | 4 |
| Central | 3 |
| Metro/North Shore | 2 |
| Cape and Islands | 1 |
| Size (# of providers) | |
| <5 | 2 |
| 5–10 | 6 |
| >10 | 2 |
| Practice Type | |
| Private | 7 |
| Hospital-owned | 1 |
| Multi-site organization | 2 |
| Median Family Income of Practice’s Locale* | |
| Above State Median ($74,167 | 5 ($85,221-$114,354) |
| Below State Median | 5 ($37,118-$73,182) |
| Informants (n=35) | |
| Age | |
| 30–39 | 5 |
| 40–49 | 11 |
| 50–59 | 12 |
| 60+ | 6 |
| Gender | |
| Female | 28 |
| Male | 7 |
| Role in Practice | |
| Practice Manager/Administrator | 12 |
| Other Manager | 7 |
| Physician | 13 |
| PCMH Coordinator | 1 |
| # Years in Profession | |
| <1–4 | 1 |
| 5–9 | 8 |
| 10–19 | 9 |
| 20+ | 17 |
We identified four major themes pertinent to the relationship between organizational factors and performance on a composite quality measure: 1) Practice Culture; 2) Practice Structures and QI Tools; 3) Attitudes and Beliefs Related to Measuring Care Quality; and 4) Perceived Barriers to Achieving High Performance on Quality Measures. Although the interview guide included open-ended questions directed specifically at clinical quality or patient experience, participant responses generally intermingled these concepts, making it impossible to attribute statements to one of these constructs with confidence. Major themes (MT) and their associated subthemes are described below with illustrative quotes; additional quotes are located in Table 2.
Table 2.
Major Themes and Sub-themes with Representative Quotes
| Themes and Subthemes | Quotes |
|---|---|
|
1. Practice Culture (Contextual Factors) |
|
| Interpersonal relationships | … We are all family. We all talk to each other like we are family. We work through things when there is problem here, problems at home…we’re one … [we are] here for each other. (1–2) |
| I think it’s basically the team [that makes our scores high]. I think we support each other really well within the clinical staff and the front staff… (4–1)* | |
| With this team-based approach, I look at the physician as the leader of the team and the MA [medical assistant] as the coordinator of the team… because the nurses are talking on the phone and giving immunizations, the doctors are in the room with the patient, and it’s really the MA, that’s how I view our team. (9–1)* | |
| Patient-centered care | Their [patient’s] car might have broken down… So… we had a little training thing to teach the office staff [to] put yourself in their shoes, turn it around, how would you like to be treated? What would you like to have done when you get to the doctor’s office … don’t make that first judgment? Wait… listen to what’s going on with them and help them solve the problem… (5–1)* |
| I called another office this morning, good docs, you know, well respected colleague … and I was stunned by how awful the experience was on the phone.… It was structured for the staff and the providers. clearly not structured for the parents… the message is, “you’re bothering us”… All those businesses that do this [good customer service] … hotels… restaurant … these places have developed a skill set about serving people [that pediatric practices need to adopt]. (8–1)* | |
| … I think we. consciously work on attitude… from the department level all the way throughout the group. But, I will say the consistent drive [to maintain positive attitudes] … and when new people come in [to work with us], that’s the culture… what you’re expected to do and that’s what everybody else does so that it’s easier to do it. (7–1)* | |
| …if your employees aren’t well taken care of then you’re not going to have the good output and they [the practice owners] do support us and they do treat us very well. …if you have happy employees, you’re going to have a great machine and it runs well. (3–1) | |
| I always felt that… my role in IT [helped our practice provide high quality care]…being a practicing physician is critical because I use the tools to build [the IT system] but… my staff gives feedback on it. There are tools that I… as a physician would never use, but… my nurses will tell me this note for a triage template doesn’t make sense… (9–1)* | |
| … you can also make a mistake and not be crucified for it. you do your best, sometimes you make a mistake. and, the doctors are supportive. so, you don’t have to feel bad. (3–1)* | |
| Leadership | |
|
2. Practice Structures and Quality Improvement Tools and Strategies (Structures and Strategies) |
|
| Practice structures | “I… meet [informally] with local… large practice administrators on a regular basis… we consult each other via e-mail quite a bit… we’re able to use our collective knowledge, collective power…” (10–1) |
| … [as] an employed physician [vs. owner] you’re not as invested in how things are going. When you are an owner-physician, you have much more investment to both sides of the equation… I’m not only concerned about what I’m doing with my patients, but how is everybody else doing? A stressed-out physician or a stressed- out staff person isn’t able to provide care that I want delivered …When I leave, I want to make sure my patients are as tenderly cared for [as if I were caring for them myself] because I care about them. (6–1)* | |
| … the physical space is a huge plus as far as patient satisfaction. one of the things we did was to make enough space so that there’s a place to move the patient out of the waiting room. So… they don’t have to wait in the waiting room very long. (7–1)* | |
| [Co-located behavioral health] … it’s such an incredibly long overdue necessary service… I think it [is]… the kind of care that people need, from a young mother who may even just have a little bit of postpartum depression to potty training, ADD, my kid’s shy, or they’re cutting. It’s immediate advice, immediate help. The doctors can just walk somebody down the hall and say - I’d like to introduce you to this person… It’s just an absolutely fabulous service. (4–1)* | |
| I think the key in our own practice is… just making sure… you hire enough people. I feel like we are so well supported with the nurses, with our managerial staff. I’m never like, oh my god I don’t have a nurse to help me… We have so much support from our nurse team, the doctor-nurse team… making sure that there is enough support staff to really help make the physician fell not stressed out. (6–1)* | |
| And then we have other in-services… that are either… customer service, which is about… expressing empathy to patients, dealing with difficult patients, or their tech [technology skills]. I was finding some people are not very tech savvy. And so we are doing some basic technology classes, computer use, EMR use… (6–1)* | |
| Our biggest challenge is… how we communicate change, because change is so constant, and people get bombarded with emails. We have gone through different email formats to try to communicate better “Why I’m receiving this, who does it affect? …What time does it need to get done?” We’re being very specific with the way we communicate internally to make sure everyone gets on the same page. (10–1)* | |
| [Independent Physician Association meetings are] The last Thursday of every month, and in the meetings the offices share information, we learn policy and procedures that they [IPA] are going to try out, test out for quality measures. And they have a big support group that if you have any questions or need any help they will come out to the office. (5–1)* | |
| So, the plus for the patient [of using scribes] is that they can deal with the doctor directly… so the patient experience is actually better. The doctor’s experience is much better because I can talk to you as a patient and not have to be doing this [mimed typing in the computer]. (8–1) | |
| …we have a suggestion board and we have to go through it at each of our large meetings and if there were anything suggested or started, they’re still up there at the next meetings so we have to say, X this was your responsibility and then she will give an update or she will say, I didn’t do it. And then that will give us the prompt to keep going with it. (9–1)* | |
| It’s a little scary [to have a patient advisory council]. It was very good. Obviously it was nice to hear that they… had very positive things to say but they also had some suggestions, like we really should spend more time [with patients] or have dedicated areas for adolescents… I think bringing the parents in to get their feedback is important. (8–1)* | |
| Quality improvement tools and strategies | We use this software… called “turbo scan” and we snap it [physical exam form] and send it to the EMR. So we are now scanning it in the room, people can walk out the door and not have to stop at the front desk. It’s a small thing, but it’s an example of why not try it? (8–1)* |
|
3. Attitudes and Beliefs, Related to Care Quality (Factors that might interact with Strategies and Contextual Factors) |
|
| Measuring quality of care | |
| …what I hate the most is… [the quality measure] antibiotics prescribed for URIs [upper respiratory infections]…they came in for upper respiratory infection… and we get a culture and we didn’t prescribe any antibiotics from the first round. But then… the culture comes back positive and we prescribe antibiotics two days later. We prescribed antibiotics not for the URI, [but] for the strep. The claim was not revised; the insurance company is going to have a mismatch. (10–1) | |
| The meaning of quality | Well this is a very difficult question… about how you measure quality in a field that likes to think it’s a science. There’s a lot more than we can measure. How do you measure art? (8–1)) |
| I think it’s [quality measurement] engaged the physicians in a way that we weren’t engaged before. We really do spend a lot of time talking about the measures … (4–1)* | |
| We happen to feel it’s time to design some independent quality measures. There is obesity initiative, as far as follow up and tracking… which I think is more true quality than just making sure they got their physical for the year. (7–1)* | |
| …quality… is just recognizing that what’s great for one patient isn’t necessarily what’s right for the other. We try to individualize that… I try to look at each patient and their individual needs and not whether or not they fit in a box, or whether or not they need a test because somebody said they should because of their age. (9–1)* | |
| The other thing I think about quality is… how do they do in the big picture? Not the little individual things, but are they eating properly? Do they have an overall healthy lifestyle?… Are they safe? Are they wearing their seatbelt? Are they learning how to swim so they don’t drown … to me that’s much bigger than getting an antibiotic… (9–1)* | |
|
4. Perceived Barriers to High Performance (Factors that might interact with Strategies and Contextual Factors) |
I think a lot of it [achieving high quality scores] is the ability for practice staff and leadership to actually think about it. So, whether it’s the time, interest, financial resources, staffing, it’s the ability to think about it and pay attention to it. (4–1) |
| I… have one patient that was a frequent in-patient… we hadn’t seen her in three years because we didn’t have a phone number, we couldn’t actually find this patient… (9–1)* | |
| I have to say one of my pet peeves is… I won’t treat your tonsillitis or strep without a throat culture, but… I’d love to have one of the HEDIS people come… get a throat culture on them. (Laughter) I’ll actually give you [the HEDIS person] an hour and I’ll give you three support people. You know what I’m talking about. (6–1)* | |
| The computer is only as good as the person who input the original data. (9–1)* | |
| Part of access (measure) is providers not being here all of the time but sort of spreading themselves thin through shifts. (10–1)* |
Practice/informant number
MT-1 Practice Culture
This theme was comprised of informants’ perceptions of how their practices’ underlying beliefs, values, and ways of interacting with each other and with patients contributed to their high performance on quality measures. These contextual factors are often described as part of an organization’s culture.32
Interpersonal relationships
Many informants referred to their clinical team “a family” and felt that team cohesiveness, good communication, and feeling that every team member had a “voice” contributed to the high quality care they delivered. These team relationships were believed to have a “trickle-down effect”, meaning that patients and parents could tell that the staff and physicians enjoyed their work and worked well together and that this led to better quality of care and patient experience.
Patient-centered care
Some informants stated that their practices provided strong patient and family-centered care, offering the following examples: partnering with parents on care, striving for physician-patient continuity, tailoring services to patients’ needs, offering specialty services on site, taking extra time with families that seem dissatisfied, offering pleasant waiting spaces, having short waits to get appointments, having appointments start on time, offering plentiful close parking, and providing good “customer service”. Informants also attributed their performance to the team’s work ethic, careful attention to detail, and positive attitudes.
Leadership
The importance of leadership was a common theme across all participating practices. “Leaders” included physicians, both with and without formal managerial roles, and practice/office, nurse, and front desk managers. Physicians taking an “old fashioned” approach (taking their own phone calls, doing home visits) set a tone for the practice and some staff said that the fact that their practice’s physicians and managers cared about them as a people, their lives outside of work, and their professional development made a difference.
A number of physicians in these higher-performing practices held leadership positions outside of the practice, serving as information technology specialists or leading hospital quality committees.
Informants believed that an “open door policy” and lack of “micro-management” contributed to staff satisfaction and subsequently to higher care quality, as did flexible scheduling and adequate staffing. One participant commented that her managers made her feel that it was “okay” to admit to making a mistake, which made it easier to address systems issues.
MT-2 Practice Structures and QI Tools and Strategies
This theme included both fixed structural aspects of a practice (e.g., size) and organizational strategies (e.g., scribes) that informants felt contributed to care quality.
Practice structures
Informants described the impact of practice size (advantages of both smaller and larger practice size), perceived strengths of a physician-owner/partner model, physical layout of an office, and access to both formal (e.g., Pediatric Research in the Outpatient Setting) and informal (e.g., field trips to other practices) learning networks as important contributors to providing high-quality care.
QI tools and strategies
One practice cited use of “scribes” as a contributor to quality of care; providers had become increasingly dissatisfied with the balance of time spent with patients versus documentation and scribes allowed the physician to spend more time with patients and families, improving satisfaction for all. Other practices designated a provider and/or a staff member to be the quality “champion”, used Plan- Do-Study-Act cycles33 when they implemented a QI project, and used a suggestion board. A number of practices also had obtained Patient Centered Medical Home recognition or were in the process of doing so and two practices had recently started a family advisory council to advise them on QI. Some informants cited the availability of both internal and external training opportunities as a contributor to their success.
Tools available in the electronic medical record (EMR), such as patient registries, intra-staff communication systems, patient-call reminder lists, and automatic “warnings” were all felt to contribute to the quality of care delivered. Informants also discussed the limits of the EMR as a QI tool, noting that it is only as good as the data entered into it.
MT-3 Attitudes and Beliefs Related to Care Quality
This theme focused on how general pediatricians and staff perceive quality measures, which could interact with organizational strategies and contextual factors, influencing their effect on a practice’s performance on quality measures.
Measuring care quality
When asked for their thoughts on measuring care quality, informants offered both positive and negative perceptions of quality measurement. One positive perception was that, although it required a good deal of administrative time to measure, document, and report performance, doing so was worth it if it improved care. Others felt that the care they provided was already high quality and that measuring quality “probably helped lower performing practices” more.
Negative perceptions of quality measures included that they do not necessarily measure what is most important, that it is possible to “game the system”, that a practice could do the right thing and not get “credit”, and that complying with quality measures sometimes has unintended consequences for patients. Some informants were of the opinion that the measures are too rigid, that they do not allow a provider to consider an individual patient’s needs, and that quality measures hold them responsible for things that are beyond their control.
The meaning of quality
We asked informants what high quality care meant to them, acknowledging that existing clinical quality and patient experience measures may not capture everything they feel is important. Responses included the need to provide equitable not equal care, supporting a child and family’s overall well-being, and the importance of both relational and technical elements of care.
MT4 Perceived Challenges to Achieving High Scores on Quality Measures
Some informants discussed factors that could affect performance on quality measures independent of organizational of organizational strategies and contextual factors, even if they felt that these did not affect quality of care per se. These included not having the resources needed to document all that they do, no time to follow up on errors in documentation with insurance companies, and that an action indicated by a quality measure is sometimes not appropriate for a given patient.
Informants also discussed financial pressures related to quality measurement. Since performance on quality measures has been increasingly tied to reimbursement, some practices felt that they had to use scarce resources to document and report quality data, but that this process did not change care quality. Another informant explained that her practice was penalized financially after joining an accountable care organization because even though her practice’s quality scores were high, other practices’ scores were not.
Discussion
In this first phase of a positive deviance study of high-performing pediatric primary care practices in Massachusetts, pediatric providers and staff offered insights into organizational strategies and contextual factors that may be associated with high scores on quality measures. Although the informants described structural factors and strategies such as us practice size and use of electronic health record-based registries for QI, many emphasized factors related to organizational culture (e.g., leadership, team function) and relational factors such as informal social networks. This suggested that these contextual factors may play an important role in the quality of care a general pediatric practice provides.
The relationship between organizational culture and successful implementation of QI strategies has been suggested in other studies. For example, King et al. studied implementation of a national literacy program in seven pediatric practices.34 A survey of 20 providers and 70 staff members found that physicians and staff at the practices that had difficulty implementing the program viewed their jobs as cumbersome, felt communication in the practice was poor, and were not perceived to be respectful of patients; physicians and staff at the practices that successfully implemented the program had positive organizational cultures similar to those described by informants in the current study. Organizational culture has also been linked to burnout, which in turn has been linked to quality of care.35,36 Should a strong association between organizational culture and performance on quality measures in pediatric primary care be borne out, interventions to better define and improve the contextual factors that contribute to this may be developed.
The current study found that access to informal information channels, such as social-professional networks outside of traditional formal structured QI resources, may be associated with performance on quality measures. Some informants reported learning about QI strategies through casual discussions with friends who had similar jobs in other practices, through informal links to other practices, and by observing other practices. While there is a substantial literature on social networks in large health care organizations,37–39 much less is known about the social networks of smaller primary care pediatric practices, particularly the relationship between both individuals’ and practices’ positions in a network and the care quality provided by the practice, offering an area of potential further investigation.
PCMH certification is associated with higher performance on some quality measures in certain settings.12,40,41 PCMH principles have been classified as “high touch” (e.g., continuity of care, adequate communication with specialists) and “low touch” (e.g., use of EMR, short wait times for appointments).40,42 A 2010 study by Ferrante et al. showed a strong association between the “high touch” principles and receipt of preventive services when compared to the “low touch”principles,42 a finding reflected in the current study’s informants’ focus on “high touch” factors to explain their high performance. Although implementing “low touch” interventions is often less complicated, developing strategies for implementing “high touch” interventions may result in higher quality of care.
This study’s strengths include use of a unique data set that provided validated quality data from the majority of pediatric practices in Massachusetts. Potential limitations included a focus on a single state, but the range of performance on quality measures suggested that results may be similar in other states. Reliance on quality data derived from a database of privately insured patients is a limitation, but that the practices interviewed cared for both privately and publicly insured patients. Low response rates for MHQP’s patients experience survey also demonstrates limitations of patient experience data in general. Mailing the interview guides to practices ahead of time may have decreased spontaneity of responses but was necessary given that some practices refused to consider participating in the study until they had a sense of what questions they would be asked and because time informants could spend was limited. Practices determined who participated in the interviews and other staff members might have offered different perceptions. Practices also chose whether to hold interviews individually or in groups, in person, or by phone. While this approach was pragmatic given busy clinical schedules, some informants’ perspectives may have been silenced due to power differentials during group interviews. Because informants spoke broadly about care quality and did not differentiate between clinical quality and patient experience scores in their comments, we often could not determine whether comments pertained to one of these constructs or both and it may that different organizational characteristics are more predictive of high scores on one of these constructs. Our study design intentionally sought informants’ perceptions of “what works”; further study is needed to determine whether the factors identified are associated with performance in a representative sample. Finally, patient interviews were beyond the scope of this study; patient experience may serve as a proxy for patient perceptions of the practice.
Although the methods used in this study preclude making broadly generalizable inferences, the findings suggest that interventions to improve organizational culture should continue to be developed as part of efforts to improve pediatric quality of care. The role of informal professional social networks in performance quality is a new finding that warrants further investigation. Future research should determine whether these and the organizational factors identified in this study are associated with performance on pediatric quality measures in a representative sample of pediatric practices. This, in turn, could offer practices evidence-based guidance on where to direct their change efforts.
What’s New?
General pediatricians and staff at high-performing practices identified contextual factors, such as leadership traits and clinical team relationships, that they felt contribute to quality of care and that may be modifiable in pediatric practices seeking to improve care quality.
Funding Source:
All phases of this study were supported by the University of Massachusetts Medical School - Baystate and the University of Massachusetts - Amherst. Dr. Goff’s time was supported by an NIH Career Development Award (NICHD K23HD080870). Dr. Lindenaur’s time was supported by an NIH Mid-career Development Award (NHLBI HL132008).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors have no conflicts of interest relevant to this article to disclose
Financial Disclosure: The authors have no financial relationships relevant to this article to disclose.
References
- 1.Mangione-Smith R, DeCristofaro AH, Setodji CM, et al. The quality of ambulatory care delivered to children in the United States. N Engl J Med. 2007;357(15):1515–1523. doi: 10.1056/NEJMsa064637 [DOI] [PubMed] [Google Scholar]
- 2.Eneriz-Wiemer M, Sanders LM, Barr DA, Mendoza FS. Parental limited English proficiency and health outcomes for children with special health care needs: a systematic review. Acad Pediatr. 2014;14(2):128–136. doi: 10.1016/j.acap.2013.10.003 [DOI] [PubMed] [Google Scholar]
- 3.Flores G, Snowden-Bridon C, Torres S, et al. Urban minority children with asthma: substantial morbidity, compromised quality and access to specialists, and the importance of poverty and specialty care. J Asthma Off J Assoc Care Asthma. 2009;46(4):392–398. doi: 10.1080/02770900802712971 [DOI] [PubMed] [Google Scholar]
- 4.Homer CJ, Szilagyi P, Rodewald L, et al. Does quality of care affect rates of hospitalization for childhood asthma? Pediatrics. 1996;98(1):18–23. [PubMed] [Google Scholar]
- 5.Fairbrother G, Friedman S, DuMont KA, Lobach KS. Markers for primary care: missed opportunities to immunize and screen for lead and tuberculosis by private physicians serving large numbers of inner-city Medicaid-eligible children. Pediatrics. 1996;97(6 Pt 1):785–790. [PubMed] [Google Scholar]
- 6.Mangione-Smith R, McGlynn EA. Assessing the quality of healthcare provided to children. Health Serv Res. 1998;33(4 Pt 2):1059–1090. [PMC free article] [PubMed] [Google Scholar]
- 7.Devising Flores G., implementing, and evaluating interventions to eliminate health care disparities in minority children. Pediatrics. 2009;124 Suppl 3:S214–223. doi: 10.1542/peds.2009-1100J [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Betancourt JR, Tan-McGrory A. Creating a safe, high-quality healthcare system for all: meeting the needs of limited English proficient populations; Comment on “Patient safety and healthcare quality: the case for language access”. Int J Health Policy Manag. 2014;2(2):91–94. doi: 10.15171/ijhpm.2014.21 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Edwards ST, Bitton A, Hong J, Landon BE. Patient-centered medical home initiatives expanded in 2009–13: providers, patients, and payment incentives increased. Health Aff Proj Hope. 2014;33(10):1823–1831. doi: 10.1377/hlthaff.2014.0351 [DOI] [PubMed] [Google Scholar]
- 10.Coker TR, Windon A, Moreno C, Schuster MA, Chung PJ. Well-child care clinical practice redesign for young children: a systematic review of strategies and tools. Pediatrics. 2013;131 Suppl 1:S5–25. doi: 10.1542/peds.2012-1427c [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Devers KJ, Foster L, Brach C. Nine states’ use of collaboratives to improve children’s health care quality in medicaid and CHIP. Acad Pediatr. 2013;13(6 Suppl):S95–102. doi: 10.1016/j.acap.2013.04.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aysola J, Bitton A, Zaslavsky AM, Ayanian JZ. Quality and equity of primary care with patient-centered medical homes: results from a national survey. Med Care. 2013;51(1):68–77. doi: 10.1097/MLR.0b013e318270bb0d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Homer CJ, Cooley WC, Strickland B. Medical home 2009: what it is, where we were, and where we are today. Pediatr Ann. 2009;38(9):483–490. doi: 10.3928/00904481-20090820-06 [DOI] [PubMed] [Google Scholar]
- 14.Mangione-Smith R, Schonlau M, Chan KS, et al. Measuring the effectiveness of a collaborative for quality improvement in pediatric asthma care: does implementing the chronic care model improve processes and outcomes of care? Ambul Pediatr Off J Ambul Pediatr Assoc. 2005;5(2):75–82. doi: 10.1367/A04-106R.1 [DOI] [PubMed] [Google Scholar]
- 15.Billett AL, Colletti RB, Mandel KE, Miller M, Sharek PJ, Lannon CM. Exemplar pediatric collaborative improvement networks: achieving results. Pediatrics. 2013;131 Suppl 4:S196–203. doi: 10.1542/peds.2012-3786F [DOI] [PubMed] [Google Scholar]
- 16.Kaplan HC, Provost LP, Froehle CM, Margolis PA. The Model for Understanding Success in Quality (MUSIQ): building a theory of context in healthcare quality improvement. BMJ Qual Saf. 2012;21(1):13–20. doi: 10.1136/bmjqs-2011-000010 [DOI] [PubMed] [Google Scholar]
- 17.Kaplan HC, Brady PW, Dritz MC, et al. The influence of context on quality improvement success in health care: a systematic review of the literature. Milbank Q. 2010;88(4):500–559. doi: 10.1111/j.1468-0009.2010.00611.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McDonald KM. Considering context in quality improvement interventions and implementation: concepts, frameworks, and application. Acad Pediatr. 2013;13(6 Suppl):S45–53. doi: 10.1016/j.acap.2013.04.013 [DOI] [PubMed] [Google Scholar]
- 19.Cooley WC, McAllister JW, Sherrieb K, Clark RE. The Medical Home Index: development and validation of a new practice-level measure of implementation of the Medical Home model. Ambul Pediatr Off J Ambul Pediatr Assoc. 2003;3(4):173–180. [DOI] [PubMed] [Google Scholar]
- 20.McAllister JW, Cooley WC, Van Cleave J, Boudreau AA, Kuhlthau K. Medical home transformation in pediatric primary care--what drives change? Ann Fam Med. 2013;11 Suppl 1:S90–98. doi: 10.1370/afm.1528 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pascale RT, Sternin J, Sternin M. The Power of Positive Deviance: How Improbable Innovators Solve the World’s Toughest Problems. Boston, Mass.; London: Harvard Business ; McGraw-Hill [distributor]; 2010. [Google Scholar]
- 22.Bradley EH, Curry LA, Ramanadhan S, Rowe L, Nembhard IM, Krumholz HM. Research in action: using positive deviance to improve quality of health care. Implement Sci IS. 2009;4:25. doi: 10.1186/1748-5908-4-25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bradley EH, Herrin J, Wang Y, et al. Strategies for reducing the door-to-balloon time in acute myocardial infarction. N Engl J Med. 2006;355(22):2308–2320. doi: 10.1056/NEJMsa063117 [DOI] [PubMed] [Google Scholar]
- 24.Massachusetts Health Quality Partners. http://www.mhqp.org/default.asp?nav=010000. Accessed September 24, 2013.
- 25.Lehrman WG, Friedberg MW. CAHPS Surveys: Valid and Valuable Measures of Patient Experience. Hastings Cent Rep. 2015;45(6):3–4. doi: 10.1002/hast.507 [DOI] [PubMed] [Google Scholar]
- 26.Toomey SL, Elliott MN, Zaslavsky AM, et al. Variation in Family Experience of Pediatric Inpatient Care As Measured by Child HCAHPS. Pediatrics. 2017;139(4). doi: 10.1542/peds.2016-3372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shwartz M, Restuccia JD, Rosen AK. Composite Measures of Health Care Provider Performance: A Description of Approaches. Milbank Q. 2015;93(4):788–825. doi: 10.1111/1468-0009.12165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 29.Dedoose. http://www.dedoose.com/. Published July 1, 2014. Accessed July 1, 2014.
- 30.Crabtree BF, Miller WL. Doing Qualitative Research. SAGE; 1999. [Google Scholar]
- 31.Strauss AC, Corbin J. Basics of Qualitative Research: Second Edition: Techniques and Procedures for Developing Grounded Theory. 2nd ed. Sage Publications, Inc; 1998. [Google Scholar]
- 32.Schneider B, Ehrhart MG, Macey WH. Organizational climate and culture. Annu Rev Psychol. 2013;64:361–388. doi: 10.1146/annurev-psych-113011-143809 [DOI] [PubMed] [Google Scholar]
- 33.Taylor MJ, McNicholas C, Nicolay C, Darzi A, Bell D, Reed JE. Systematic review of the application of the plan-do-study-act method to improve quality in healthcare. BMJ Qual Saf. 2014;23(4):290–298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.King TM, Muzaffar S, George M. The role of clinic culture in implementation of primary care interventions: the case of Reach Out and Read. Acad Pediatr. 2009;9(1):40–46. doi: 10.1016/j.acap.2008.10.004 [DOI] [PubMed] [Google Scholar]
- 35.Helfrich CD, Simonetti JA, Clinton WL, et al. The Association of Team-Specific Workload and Staffing with Odds of Burnout Among VA Primary Care Team Members. J Gen Intern Med. 2017;32(7):760–766. doi: 10.1007/s11606-017-4011-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Humphries N, Morgan K, Conry MC, McGowan Y, Montgomery A, McGee H. Quality of care and health professional burnout: narrative literature review. Int J Health Care Qual Assur. 2014;27(4):293–307. doi: 10.1108/IJHCQA-08-2012-0087 [DOI] [PubMed] [Google Scholar]
- 37.Dunn AG, Westbrook JI. Interpreting social network metrics in healthcare organisations: a review and guide to validating small networks. Soc Sci Med 1982. 2011;72(7):1064–1068. [DOI] [PubMed] [Google Scholar]
- 38.Jippes E, Achterkamp MC, Brand PL, Kiewiet DJ, Pols J, van Engelen JM. Disseminating educational innovations in health care practice: training versus social networks. Soc Sci Med 1982. 2010;70(10):1509–1517. [DOI] [PubMed] [Google Scholar]
- 39.Meltzer D, Chung J, Khalili P, et al. Exploring the use of social network methods in designing healthcare quality improvement teams. SSM Soc Sci Med. 2010;71(6):1119–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jackson GL, Powers BJ, Chatterjee R, et al. The Patient-Centered Medical Home A Systematic Review. Ann Intern Med. 2013;158(3):169–178. doi: 10.7326/0003-4819-158-3-201302050-00579 [DOI] [PubMed] [Google Scholar]
- 41.DeVries A, Li C-HW, Sridhar G, Hummel JR, Breidbart S, Barron JJ. Impact of medical homes on quality, healthcare utilization, and costs. Am J Manag Care. 2012;18(9):534–544. [PubMed] [Google Scholar]
- 42.Ferrante JM, Balasubramanian BA, Hudson SV, Crabtree BF. Principles of the Patient-Centered Medical Home and Preventive Services Delivery. Ann Fam Med. 2010;8(2):108–116. doi: 10.1370/afm.1080 [DOI] [PMC free article] [PubMed] [Google Scholar]