Abstract
Objective
Back and neck pain are associated with disability and loss of independence in older adults. It’s unknown whether long-term management using commonly recommended treatments is superior to shorter-term treatment. This randomized clinical trial compared short-term treatment (12 weeks) versus long-term management (36 weeks) of back and neck related disability in older adults using spinal manipulative therapy (SMT) combined with supervised rehabilitative exercises (SRE).
Methods
Eligible participants were age 65 and older with back and neck disability for more than 12 weeks. Co-primary outcomes were changes in Oswestry and Neck Disability Index after 36 weeks. An intention to treat approach used linear mixed-model analysis to detect between group differences. Secondary analyses included other self-reported outcomes, adverse events and objective functional measures.
Results
182 participants were randomized. The short-term and long-term groups demonstrated significant improvements in back (−3.9, 95% confidence interval (CI) −5.8 to −2.0 versus −6.3, 95% CI −8.2 to −4.4) and neck disability (−7.3, 95% CI −9.1 to −5.5 versus −9.0, 95% CI = −10.8 to −7.2) after 36 weeks, with no difference between groups (back 2.4, 95% CI −0.3 to 5.1; neck 1.7, 95% CI −0.8 to 4.2). The long-term management group experienced greater improvement in neck pain at week 36, self-efficacy at week 36 and 52, functional ability and balance.
Conclusion
For older adults with chronic back and neck disability, extending management with SMT and SRE from 12 to 36 weeks did not result in any additional important reduction in disability.
Back and neck pain are common symptoms in the elderly and are associated with significant disability which can negatively impact general health, functional independence, and quality of life. 1–5 Back and neck pain often occur together 6 and are the leading causes of years lived with disability globally. 7 Spine pain ranks as the second most expensive chronic non-cancer pain among Medicare recipients in the US. 8 As the population of adults over the age of 65 is predicted to double in size by 2050, 9 mitigating the effects of back and neck related disability is an important public health priority.
More than half of individuals presenting for back or neck pain care report continued or recurrent pain after one year. 10, 11 This raises the question of whether longer-term management strategies 12 may be effective in sustaining improvement over time. While this has been explored in small studies of adults with low back pain 13, 14 the evidence remains inconclusive, particularly in relation to the elderly. Spinal manipulative therapy (SMT) and supervised rehabilitative exercise (SRE) are both recommended first line, non-pharmacologic treatments for back and neck pain in the general population. 15–18 Combining both approaches may result in superior pain relief and function. 19 In a previous study by our team, a combination of SMT and SRE resulted in greater improvements among older adults suffering from neck pain and disability than exercise alone; 20 however, there remains a lack of robust research in this area and little attention paid to the effectiveness of longer term management.
The primary aim of this randomized, observer-blinded, comparative effectiveness trial was to compare the effectiveness of SMT + SRE, delivered via either a short-term treatment (12 weeks) or long-term management (36 weeks) strategy, on older adults with spine-related disability. Neck and back disability were co-primary outcomes. Secondary outcomes included neck and back pain, general heath, improvement, self-efficacy, kinesiophobia, satisfaction, falls, medication use, and biomechanical functional measures.
Materials and Methods
Study Design
This randomized clinical trial was approved by the Institutional Review Board at Northwestern Health Sciences University. An in-depth description of the study design, treatment protocols, and outcome measures has been previously published. 21
Participants were recruited from a metropolitan area in the upper mid-west United States. Individuals were screened for general inclusion criteria by certified study personnel utilizing a computer-guided questionnaire. Those who qualified after initial screening attended a series of two baseline evaluations comprised of informed consent, patient self-report questionnaires, health history, physical evaluation, cervical and lumbar x-rays and a functional assessment.
Participants were 65 years of age and older, English speaking, and community dwelling, with self-reported back and neck disability ≥ 12 weeks in duration. Disability was defined as scoring 10% or higher on both the Neck Disability Index (NDI) and Oswestry Disability Index (ODI), with the addition of both scores totaling 25 or greater. Participants also had the ability to ambulate without the aid of a wheelchair or motorized scooter and had stable prescription pain medication use in the 4 weeks prior to enrollment. Exclusion criteria included significant co-morbid conditions and frank contraindications to either SMT or SRE. 21
Randomization
Eligible individuals were randomly assigned to treatment, using a 1:1 computer generated random block permutation allocation scheme under the direction of an independent statistician. The randomization scheme was concealed from study staff, who opened sequentially numbered, opaque, sealed envelopes containing treatment assignments in the presence of participants as they became eligible.
Originally a 3-arm study, the third comparison group (SRE alone for 36 weeks) was discontinued after 18 randomized participants due to slower than projected enrollment and award reductions from the funding agency. The modified, 2-arm design was approved by the steering committee, funding agency, IRB and data and safety monitoring board.
Interventions
Participants received either 12 or 36 weeks of SMT+ SRE. The same treatments were delivered in both study groups, with the only exception being length of care. SMT was delivered by chiropractors with at least 5 years of experience. SRE was delivered by exercise therapists with at least 4 years of experience instructing pain patients in therapeutic exercise. The exercise therapists were trained to follow a standardized program and delivered care under the supervision of study chiropractors.
SMT focused on high velocity, low amplitude manipulation. 22 Low amplitude mobilization, manual distraction, gentle soft tissue massage, heat or cold therapy, and active or passive muscle stretching were permitted to facilitate SMT. The frequency of care, spinal region(s) treated, and type of therapy used were left to the discretion of the treating chiropractor, based on clinical experience, patient preferences and response to care. Visits were approximately 20 to 30 minutes in length. Each participant received SMT a minimum of once per month, with treatments not exceeding twice per week.
SRE consisted of an aerobic warm up, followed by a standardized program of stretching, strengthening, and balance exercises used in previous research studies and described at length elsewhere. 21 The selection of exercises, progressions, and number of repetitions were individualized to accommodate participants’ abilities and tolerance. All participants received standardized advice to stay active and self-care tips for pain management. Participants received one-hour instructional sessions twice in the first month, then once per month through the duration of the randomly assigned intervention phase, with daily home exercises encouraged between sessions.
Standardized forms documented treatment visits, including examination findings, treatment used, adverse events, and compliance.
Data Collection
Sociodemographic data were collected at baseline. Patient self-report outcomes were collected via questionnaires at baseline and weeks 4, 12, 34, 36, 52, and 78. Functional outcome measures were recorded at baseline and week 37. Qualitative interviews were collected post intervention (week 12 or 36, depending on group). Physical activity assessed with accelerometry, and participants’ perspectives of treatment as ascertained during qualitative interviews, will be reported in subsequent publications.
Co-primary Outcomes
Back and neck disability were measured using the Oswestry Disability Index, version 2.0 23, 24 and the Neck Disability Index. 25 The NDI was derived from the ODI, therefore having similar measurement properties and aiding in the comparison of results. Each asks individuals to rate 10 functional activities on a scale of 0–5 (0=no disability with activity, 5=maximal disability), with high scores indicating increasing disability.
Secondary Outcomes
Neck and low back pain in the past week, days of prescription or over-the-counter medication, improvement, satisfaction, kinesiophobia, self-efficacy, quality of life, and expectations for improvement were secondary outcomes. The incidence of falls was collected by asking participants if they have fallen and landed on the floor or ground or have fallen and hit an object like a table or chair during the previous four weeks. 26 Functional ability was assessed by hand grip strength and the Short Physical Performance Battery (SPPB). 27, 28
A more detailed description of data collection has been described in a previous publication. 21
Adverse Events
Active and passive surveillance methods were used to collect information on adverse events. Patient self-report questionnaires asked, “since you started treatment in the study have you experienced any of the following?”, followed by a list of side effects known to be associated with SMT and exercise. Participants were asked to rate “yes” responses on a 0–10 bothersomeness scale, with 0=not at all bothersome, and 10=extremely bothersome. 29 Chiropractors and therapists queried patients about side effects since the last visit and documented responses on standardized treatment forms. Adverse events were categorized by investigators according to standards defined by the U.S. Department of Health and Human Services.
Sample Size
For a two-arm design, 85 participants were needed to detect a minimally important between group difference of 10% in the co-primary outcome ODI at week 36, with a power of 0.90 and alpha level of 0.025. Assuming a 15% loss to follow up rate, 100 individuals were sought for each treatment group.
Analysis
Analyses followed a pre-specified plan and were performed using Statistical Analysis Software (version 9.3, SAS Institute Inc., Cary, NC). An intention-to-treat approach included all participants in their originally assigned group. Baseline demographic and clinical characteristics of groups were compared using two-sample t tests, Wilcoxon rank sum test, and Chi-square/Fisher’s exact tests where appropriate. Baseline demographic or clinical variables considered relevant by the investigators based on the literature, or those correlated at 0.5 or greater with the primary outcomes, were included as covariates in all primary and secondary analyses. Gender and expectations have been shown to be predictive of persistent musculoskeletal-related disability in the elderly; 30 these variables were subsequently included as covariates.
Primary analysis used linear mixed models (PROC MIXED in SAS) to compare between group differences in the co-primary outcomes of ODI and NDI between baseline and week 36. All participants scored both regardless of where their primary complaint was, and each was analyzed separately. The model adjusted for the fixed effects of treatment group, time, and treatment x time interaction, and included a random intercept to account for within-patient correlations. The alpha level was reduced to 0.025 to account for testing two independent primary outcomes.
The proportion of participants in each group demonstrating ≥15%, ≥30% and ≥50% improvement in ODI and NDI from baseline were compared using logistic regression. 31, 32 Finally, area under the curve (AUC) analyses of neck and back disability were conducted using linear regression models.
Secondary outcome measures were similarly analyzed using linear mixed models. Analyses included between group differences at all time points, as well as within group change from baseline at each time point. Baseline outcome measures were included as covariates when available.
Descriptive statistics of baseline characteristics and outcome measures in the 36 week exercise only arm of the study (n=18) were not part of the primary analyses, and are reported separately in Supplementary Table S1.
Results
Of 612 screened, 182 individuals were randomized (91 to each group). An additional 18 people were randomized to a discontinued third intervention group of 36 weeks of SRE (see Supplementary Table S1). Figure 1 describes participant flow through the study. Follow up rates were high, with an overall 97% collection rate of the co-primary outcomes at week 36. Treatment groups were similar at baseline (Table 1), with the exception of lower expectations for improvement and a greater proportion of women in the short-term treatment group. On average, study participants reported moderate neck (25.9) and back related (26.2) disability, and moderate neck (4.6) and back (5.0) pain.
Figure 1.
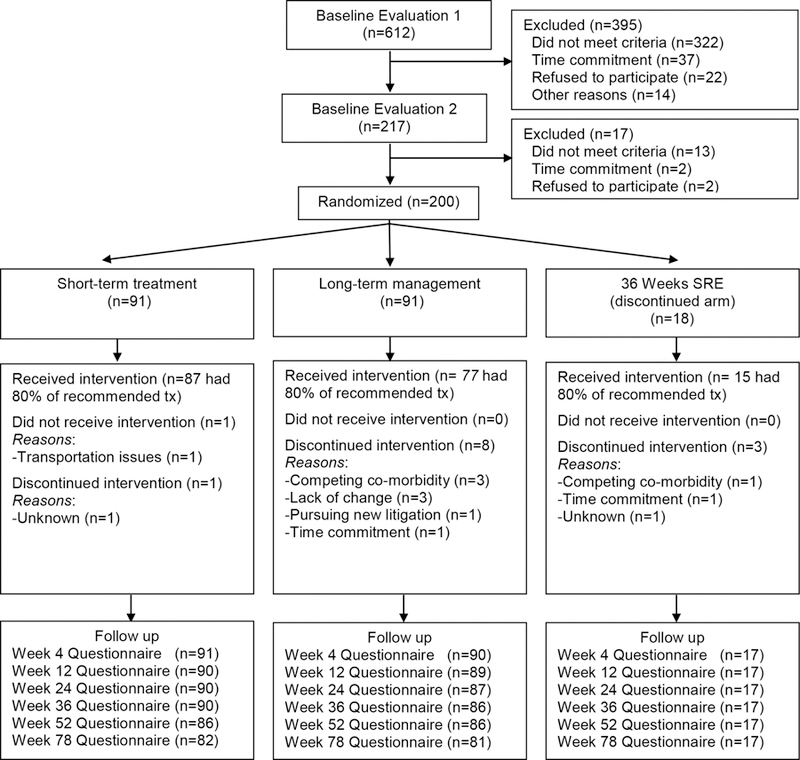
Study participant flow chart
Table 1.
Participant demographics and baseline clinical characteristics
| Mean (SD) or N (%) | Overall N=182 |
Short-term treatment SMT+SRE N=91 |
Long-term management SMT + SRE N=91 |
P value | ||
|---|---|---|---|---|---|---|
| Age (years) | mean (SD) | 71.1 (5.3) | 71.5 (5.4) | 70.7 (5.2) | 0.35 | |
| median (range) | 69 (65 – 87) | 70 (65 – 86) | 69 (65 – 87) | |||
| Female | 108 (59%) | 61 (67%) | 47 (52%) | 0.035† | ||
| Duration of neck pain (years) |
mean (SD) | 12.7 (13.1) | 13.6 (12.6) | 11.7 (13.6) | ||
| median (range) | 10 (0.2 – 58) | 10 (.2 – 50) | 7.5 (.2 – 58) | 0.10 | ||
| Duration of back pain (weeks) |
mean (SD) | 17.6 (15.8) | 18.0 (15.0) | 17.2 (16.7) | ||
| median (range) | 14.5 (0.2 – 60) | 15 (0.3 – 60) | 13 (0.2 – 60) | 0.31 | ||
| Ethnicity | ||||||
| Hispanic or Latino | 1 (1%) | 0 (0%) | 1 (1%) | 1 | ||
| Not Hispanic or Latino | 177 (99%) | 88 (100%) | 89 (99%) | |||
| Race | ||||||
| White | 175 (97%) | 90 (99%) | 85 (94%) | 0.12 | ||
| All othersa | 6 (3%) | 1 (1%) | 5 (6%) | |||
| Physical activity levelb | 3.5 (0.8) | 3.5 (0.7) | 3.5 (0.8) | 0.85 | ||
| Neck Disability Index (0–100) | 25.9 (8.5) | 25.2 (7.5) | 26.6 (9.3) | 0.26 | ||
| Neck pain (0–10) | 4.6 (1.7) | 4.5 (1.6) | 4.7 (1.8) | 0.42 | ||
| Back Disability Index (0–100) | 26.2 (9.2) | 25.6 (8.1) | 26.7 (10.2) | 0.39 | ||
| Back pain (0–10) | 5.0 (1.9) | 5.1 (1.8) | 5.0 (2.0) | 0.70 | ||
| Tobacco use (yes) | 14 (8%) | 6 (7%) | 8 (9%) | 0.58 | ||
| Alcohol use (yes) | 102 (56%) | 47 (52%) | 55 (60%) | 0.23 | ||
| Body Mass Index | 28.8 (5.8) | 28.7 (5.8) | 28.9 (5.8) | 0.79 | ||
| Quebec Task Force Classification (neck)c | ||||||
| 1 | 41 (23%) | 20 (22%) | 21 (23%) | 0.56 | ||
| 2 | 101 (55%) | 47 (52%) | 54 (59%) | |||
| 3a | 17 (9%) | 9 (10%) | 8 (9%) | |||
| 3b | 16 (9%) | 11 (12%) | 5 (5%) | |||
| 3c | 7 (4%) | 4 (4%) | 3 (3%) | |||
| Quebec Task Force Classification (back)d | ||||||
| 1 | 118 (65%) | 61 (67%) | 57 (63%) | 0.69 | ||
| 2 | 34 (19%) | 16 (18%) | 18 (20%) | |||
| 3 | 22 (12%) | 9 (10%) | 13 (14%) | |||
| 4 | 8 (4%) | 5 (5%) | 3 (3%) | |||
| Expectations for improvemente | 2.5 (0.8) | 2.4 (0.7) | 2.7 (0.8) | 0.028† | ||
Statistically significant pairwise comparison at ≤0.05
All others includes American Indian or Alaska Native (n=1), Black or African American (n=4), and Other (n=1)
Physical activity level (1=no physical activity, 6=very heavy physical activity)
Quebec Task Force Categories (neck) 1=neck complaint of pain, stiffness, or tenderness only; 2=neck complaint and musculoskeletal sign(s) without radiation; 3=neck complaint and a) pain + radiation to extremity, proximally, b) pain + radiation to extremity, distally, c) pain + radiation to upper limb with neurologic signs
Quebec Task Force Categories (back) 1=pain without radiation; 2=pain + radiation to proximal extremity; 3=pain + radiation to distal extremity; 4=pain + radiation to lower limb with neurologic signs
Expectations for improvement: “Three months from now, how do you expect your back and neck problem to be?” (1=no symptoms/ 100% improvement, 9=as bad as it could be/ 100% worse)
Participants in the short-term treatment group attended an average of 10 SMT and 4 exercise instruction visits. Those in the long-term management group attended an average of 19 SMT and 9 exercise instruction visits, with an average of 11 SMT and 4 exercise visits occurring in the first 12 weeks. Participants in both groups reported performing the exercises at home an average of four times per week at the week 12 visit. That number decreased in both groups to an average of three times per week at the week 36 visit. While both groups demonstrated improvement, there was no statistically significant difference between groups in the co-primary outcomes of neck and back disability between baseline and week 36 (Table 2). This was confirmed by the AUC analysis (ODI = 38.5 (−141.2, 218.2), p = 0.67; ND I= −10.0 (−180.8, 160.7) p = 0.91). The responder analysis demonstrated no statistically significant differences in the proportions who reached 15%, 30% or 50% improvement in disability at either the 12 or 36 week time point (Supplemental Figure S1 and Supplemental Figure S2). The only exception was the proportion reaching 50% improvement in neck disability, which favored the short-term treatment group at week 12 (p=0.05). Overall, both groups actualized the greatest proportion of responders for each threshold at the end of their respective treatment periods.
Table 2.
Co-primary outcomes: changes from baseline and between group differences in neck and back disability
| Mean (95% CI) |
||||
|---|---|---|---|---|
| Co-primary Outcomes | Short-term treatment (N=91) |
Long-tern management (N=91) |
Mean Difference (95% CI) |
P Value |
| Neck Disability (NDI)a | ||||
| Baseline | 25.2 (23.7, 26.8) | 26.6 (24.7, 28.6) | −1.4 (−3.9, 1.1) | 0.26 |
| Change from baseline to wk 4 | −4.5 (−6.2, −2.7) | −2.9 (−4.7, −1.2) | −1.5 (−4.0, 0.9) | 0.23 |
| Change from baseline to wk 12 | −7.8 (−9.6, −6.1) | −5.5 (−7.3, −3.8) | −2.3 (−4.8, 0.2) | 0.07 |
| Change from baseline to wk 24 | −7.6 (−9.3, −5.8) | −5.7 (−7.4, −3.9) | −1.9 (−4.4, 0.6) | 0.14 |
| Change from baseline to wk 36 | −7.3 (−9.1, −5.5) | −9.0 (−10.8, −7.2) | 1.7 (−0.8, 4.2) | 0.18 |
| Change from baseline to wk 52 | −7.2 (−9.0, −5.4) | −7.1 (−8.9, −5.3) | −0.1 (−2.6, 2.4) | 0.95 |
| Change from baseline to wk 78 | −6.8 (−8.6, −5.0) | −8.6 (−10.4, −6.8) | 1.8 (−0.8, 4.4) | 0.17 |
| Back Disability (ODI)b | ||||
| Baseline | 25.6 (23.9, 27.3) | 26.7 (24.6, 28.9) | −1.2 (−3.9, 1.5) | 0.39 |
| Change from baseline to wk 4 | −1.9 (−3.8, 0) | −2.0 (−3.9, −0.2) | 0.1 (−2.5, 2.8) | 0.92 |
| Change from baseline to wk 12 | −6.1 (−8.0, −4.2) | −4.6 (−6.5, −2.7) | −1.5 (−4.2, 1.1) | 0.26 |
| Change from baseline to wk 24 | −5.5 (−7.4, −3.6) | −4.1 (−6.0, −2.3) | −1.4 (−4.0, 1.3) | 0.32 |
| Change from baseline to wk 36 | −3.9 (−5.8, −2.0) | −6.3 (−8.2, −4.4) | 2.4 (−0.3, 5.1) | 0.08 |
| Change from baseline to wk 52 | −3.6 (−5.6, −1.7) | −4.4 (−6.3, −2.5) | 0.8 (−1.9, 3.5) | 0.56 |
| Change from baseline to wk 78 | −3.5 (−5.5, −1.5) | −5.8 (−7.7, −3.8) | 2.3 (−0.5, 5.0) | 0.11 |
NDI=Neck Disability Index. Higher scores indicate greater disability.
ODI=Oswestry Disability Index. Higher scores indicate greater disability.
With few exceptions, there were no statistically significant differences between groups in secondary patient self-report outcomes (Table 3). Those in the long-term management group did experience greater improvement in neck pain at week 36, and greater gains in self-efficacy at week 36 and 52. Expectations for improvement decreased in both groups over time, although more significantly so in the short-term treatment group. There were statistically significant between group differences in the SPPB overall score, and in the SPPB balance test sub-score in favor of the long-term management group (Supplemental Table S2). No between group differences were observed for the rate of self-reported falls during the follow-up period (Supplemental Table S3).
Table 3.
Patient self-report outcomes at baseline and change at weeks 12, 36, 52 and 78
| Outcome Measure |
Time point/ Change from baseline at time point |
Mean (95% CI) | Mean Difference (95% CI) |
P Value | |
|---|---|---|---|---|---|
| Short-term treatment (N=91) |
Long-term management (N=91) |
||||
| Neck paina | Baseline | 4.5 (4.2, 4.8) | 4.7 (4.3, 5.1) | −0.2 (−0.7, 0.3) | 0.42 |
| Change from baseline to wk 12 | −1.7 (−2.1, −1.3) | −1.3 (−1.7, −0.9) | −0.4 (−0.9, 0.2) | 0.17 | |
| Change from baseline to wk 36 | −1.4 (−1.8, −1.1) | −2.1 (−2.5, −1.7) | 0.7 (0.1, 1.2) | 0.02† | |
| Change from baseline to wk 78 | −1.6 (−2.0, −1.2) | −1.9 (−2.3, −1.5) | 0.2 (−0.3, 0.8) | 0.41 | |
| Back paina | Baseline | 5.1 (4.7, 5.4) | 5.0 (4.5, 5.4) | 0.1 (−0.5, 0.7) | 0.70 |
| Change from baseline to wk 12 | −1.9 (−2.3, −1.5) | −1.4 (−1.8, −1.0) | −0.5 (−1.1, 0.0) | 0.07 | |
| Change from baseline to wk 36 | −1.6 (−2.0, −1.2) | −2.0 (−2.4, −1.6) | 0.4 (−0.2, 1.0) | 0.19 | |
| Change from baseline to wk 78 | −1.4 (−1.9, −1.0) | −1.7 (−2.2, −1.3) | 0.3 (−0.3, 0.9) | 0.33 | |
| Medication useb | Baseline | 3.0 (2.5, 3.6) | 2.7 (2.2, 3.3) | 0.3 (−0.5, 1.0) | 0.50 |
| Change from baseline to wk 12 | −0.6 (−1.0, −0.1) | −0.8 (−1.2, −0.3) | 0.2 (−0.5, 0.9) | 0.55 | |
| Change from baseline to wk 36 | −0.5 (−0.9, 0.0) | −0.9 (−1.4, −0.5) | 0.5 (−0.2, 1.1) | 0.16 | |
| Change from baseline to wk 78 | −0.8 (−1.3, −0.3) | −0.3 (−0.8, 0.2) | −0.5 (−1.2, 0.2) | 0.12 | |
| Improvementc | 12 wk | 3.0 (2.7, 3.3) | 3.4 (3.1, 3.7) | −0.4 (−0.8, 0.0) | 0.07 |
| 36 wk | 3.3 (3.0, 3.6) | 3.1 (2.8, 3.4) | 0.2 (−0.2, 0.6) | 0.31 | |
| 78 wk | 3.3 (3.0, 3.6) | 3.3 (3.0, 3.5) | 0.0 (−0.4, 0.4) | 0.89 | |
| Satisfactiond | 12 wk | 1.8 (1.6, 2.0) | 1.8 (1.6, 2.0) | −0.1 (−0.3, 0.2) | 0.73 |
| 36 wk | 2.0 (1.8, 2.2) | 1.8 (1.6, 2.0) | 0.2 (−0.1, 0.5) | 0.13 | |
| 78 wk | 2.2 (2.0, 2.3) | 2.0 (1.8, 2.2) | 0.1 (−0.2, 0.4) | 0.35 | |
| Kinesiophobiae | Baseline | 34.5 (33.4, 35.6) | 34.2 (33.1, 35.4) | 0.2 (−1.3, 1.8) | 0.77 |
| Change from baseline to wk 12 | −3.1 (−4.1, −2.2) | −2.1 (−3.1, −1.1) | −1.0 (−2.4, 0.4) | 0.14 | |
| Change from baseline to wk 36 | −2.5 (−3.5, −1.5) | −1.9 (−2.9, −0.9) | −0.6 (−2.0, 0.8) | 0.39 | |
| Change from baseline to wk 78 | −2.2 (−3.3, −1.2) | −1.7 (−2.7, −0.7) | −0.6 (−2.0, 0.9) | 0.43 | |
| Self efficacyf | Baseline | 49.0 (47.4, 50.7) | 46.3 (44.2, 48.3) | 2.8 (0.1, 5.4) | 0.04† |
| Change from baseline to wk 12 | 3.1 (1.6, 4.6) | 1.3 (−0.2, 2.7) | 1.8 (−0.3, 3.9) | 0.08 | |
| Change from baseline to wk 36 | 1.4 (−0.1, 2.9) | 3.6 (2.1, 5.1) | −2.2 (−4.3, −0.1) | 0.04† | |
| Change from baseline to wk 78 | 0.9 (−0.7, 2.4) | 2.6 (1.1, 5.0) | −1.7 (−3.9, 0.5) | 0.12 | |
| Quality of life (EuroQol) indexg | Baseline | 0.8 (0.8, 0.8) | 0.8 (0.8, 0.8) | 0.0 (−0.0, 0.0) | 0.94 |
| Change from baseline to wk 12 | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.0) | 0.0 (−0.0, 0.0) | 0.15 | |
| Change from baseline to wk 36 | 0.0 (0.0, 0.1) | 0.0 (0.0, 0.0) | 0.0 (−0.0, 0.0) | 0.72 | |
| Change from baseline to wk 78 | 0.0 (0.0, 0.0) | 0.0 (0.0, 0.0) | 0.0 (−0.0, 0.0) | 0.92 | |
| Expectations for improvementh | Baseline | 2.4 (2.3, 2.6) | 2.7 (2.5, 2.8) | −0.3 (−0.5, 0.0) | 0.03† |
| Change from baseline to wk 12 | 0.6 (0.3, 0.8) | 0.1 (−0.1, 0.3) | 0.5 (0.1, 0.8) | 0.01† | |
| Change from baseline to wk 36 | 0.9 (0.7, 1.2) | 0.6 (0.3, 0.8) | 0.4 (0.0, 0.7) | 0.05† | |
Statistically significant pairwise comparison at <0.05
Neck and low back pain in the past week (0–10). Lower scores indicate less pain.
Days of prescription or over-the-counter medication use over the past week (0=have not taken any, 7=every day).
Improvement (1=no symptoms/100% improvement, 9=as bad as it could be/ 100% worse)
Satisfaction (1=completely satisfied/ couldn’t be better, 7=completely dissatisfied, couldn’t be worse)
Tampa Scale of Kinesiophobia (17-item instrument). Lower scores indicate lower levels of kinesiophobia.
Pain Self-Efficacy Questionnaire (10-item instrument). Higher scores indicate stronger self efficacy beliefs.
EuroQol EQ-5D was used to determine participants’ general health. US population based preferences were used to calculate an index score. Higher scores indicate greater health status.
Expectations for improvement measured by asking “Three months from now, how do you expect your back and neck problem to be?” (1=no symptoms/ 100% improvement, 9=as bad as it could be/ 100% worse)
Non-study Treatment
At 12 weeks, 11 participants (6 in the short-term treatment group, 5 in the long-term management group) reported visits to non-study health care providers for their back or neck problem in the past month. At week 36, that number grew to 21 visits reported among those whose study treatment had ended at 12 weeks, and 17 visits for those just finishing their 36 weeks of treatment in the long-term management group. At the week 78 long-term follow up, similar numbers in each group (25 in the short-term group, 28 in the long-term treatment group) reported non-study health care visits.
Adverse Events
No serious adverse events were reported. Six individuals reported mild to moderate adverse events (three in each group) and included one or a combination of: increase in neck pain (2), back pain (1), numbness in the hands (2) or feet (2), headache (1), and dizziness with exercise (1). Approximately half of participants reported in questionnaires that they experienced at least one side effect over the course of the study (51% of the total sample at 12 weeks; 58% of those in the short-term treatment group, 47% of the long-term management group at 36 weeks). No significant difference between groups was observed in frequency at either time point. An increase or change in neck or back pain was most common.
Discussion
This study is one of the first to examine the relative effectiveness of short-term treatment (12 weeks) versus long-term management (36 weeks) of commonly recommended non-pharmacologic treatments, SMT with SRE, for older spine pain sufferers. It is also novel in that it addresses low back and neck pain related disability simultaneously, which better reflects patients’ real-world pain experiences in which back and neck pain co-occur. 6, 33, 34 While both groups experienced improvements in disability from baseline to week 36, there were no statistically significant differences and small effect size between groups (Cohen’s effect size 0.22 for NDI and 0.25 for ODI). Both groups achieved the greatest average improvement at the time of treatment completion, and generally sustained improvement through the long term. Similar results were observed for the secondary outcomes, with the exception of the long-term management group self-reporting greater improvement in neck pain and self-efficacy and exhibiting increased gains in some objective functional measures. Future effectiveness and cost-effectiveness studies with long-term follow-up are needed to determine whether these improvements in secondary outcomes are worth the extra time and cost associated with long-term management. Importantly, no serious adverse events were reported. Cumulatively these findings suggest SMT and SRE are safe for elderly individuals experiencing low back and neck pain related disability and that longer-term management may empower them and result in important functional benefits (e.g. balance, physical performance).
The lack of group differences in primary and most secondary outcomes, and the absence of a no-treatment control, make it difficult to discern the extent to which natural history and regression to the mean impacted the results. However, given the older age, chronicity and disability of the study sample, and the persistence of observed improvements through the 78 week follow up, it is likely that the SMT and SRE conferred specific benefits.
Expectations have been shown to be predictive of persistent disability among older adults receiving treatment for musculoskeletal conditions. 30 Initially, expectations for improvement were greater among participants randomized to the long-term management group, compared to those receiving a shorter course of care. As a result, this baseline difference was included as a covariate in the analysis. Over the course of the trial, both groups lowered their expectations for improvement, more so in the short-term treatment group. The reasons for this change in expectations, and their impact on improvement, warrants further exploration.
More than a quarter of the study sample achieved greater than 50% improvement in neck and back disability at the primary time point; 33–55% reported obtaining 30% improvement. Nearly three quarters of participants reported at least 15% improvement in neck disability, and more than half reported the same magnitude of improvement in back disability. We report a range of thresholds in the responder analysis of this study, as there is some disagreement in the literature as to what constitutes clinically important difference in the NDI 35, 36 and ODI. 32, 37, 38 A change of 15% may represent a clinically meaningful improvement among older adults suffering from chronic spine related disability, especially given the relatively low cost and low risk of SMT and SRE as interventions. 31, 39, 40
Maintaining good physical function is crucial for the elderly to remain independent. At 36 weeks, those in the long-term management group had significantly increased their score on the Short Physical Performance Battery compared to the short-term treatment group, by a degree that could be considered medium in terms of meaningful change (.76 versus .14 points). 41 The Balance Test sub-score decreased slightly in the short-term group whereas it increased significantly in the long-term group (−0.03 versus 0.33).
Using the Oswestry and NDI instruments to measure disability, we observed that improvements were generally larger for NP than for LBP (−8.28 versus −5.13 for whole sample), and this was true for both men and women (data not shown). The change in neck disability is similar to the 8.4 point improvement observed in a previous trial investigating the same interventions in an elderly population over a 12 week period. Differences in pain, however, was less than the 3 point change observed in that trial.20 Whether SRE and SMT combined are genuinely more effective for chronic NP than for chronic LBP in the elderly, or whether this is explained by differences in responsiveness between the two disability instruments cannot be elucidated from our data.
Originally this trial was designed to include a third arm, which would have allowed us to assess the impact of adding SMT to SRE. Redesign due to poor enrollment and funding did not likely influence the results as reported here. Strengths include a rigorous study design including self-report and objective measures; standardized, yet pragmatic interventions; and high follow-up rates. Limitations include the inability to blind clinicians and participants due to the nature of the interventions. While combining both neck and back related disability into a single study population may create a more heterogenous sample than either alone, doing so reflects the phenomenon of spine related disability for many sufferers, and how patients present for care. This trial did not differentiate between specific effects of the intervention and contextual effects, which may play a large role when treating people with chronic pain. However, the treatments as studied generally reflect how spinal manipulation and rehabilitative exercise are delivered in clinical practice. Finally, while visits to non-study health care providers was similar between groups, the impact on the study results is unknown.
Our study adds additional support to evidence-based guidelines, which recommend that manual treatment, along with general and specific exercises, should be considered as first line treatments for people with back and neck pain. 15–18
Conclusion
For adults aged 65 and older with chronic back and neck disability, extending management with SMT and SRE from 12 to 36 weeks did not result in any additional important reduction in disability. Statistically significant differences in favor of long-term management were found for the secondary outcomes of self-reported improvement in neck pain and self-efficacy, as well as functional measures of balance and physical performance. These findings may be important for healthy ageing and spine care in the elderly, and warrant further investigation.
Supplementary Material
Supplemental Figure S1. Responder Analyses of Neck Disability Index
Note: More individuals in the short-term treatment group achieved ≥50% reduction in neck disability after 12 weeks of care, AOR=2.14 (1.01, 4.53), p=0.05
Supplemental Figure S2. Responder Analysis for Oswestry Disability Index (ODI)
Significance and Innovations.
Back and neck pain are not only common among older adults but result in significant disability and loss of independence.
Both short-term treatment and long-term management with a combination of spinal manipulative therapy and exercise resulted in similar improvement in disability, with the greatest improvement achieved at the time of treatment completion.
Long-term management resulted in greater improvement in neck pain and self-efficacy, as well as balance and physical performance.
While mild, transient side effects were common, no serious adverse events reported by participants.
Acknowledgments
Funding source
The trial was funded by the U.S. Department of Health and Human Services Health Resources and Services Administration (HRSA), Bureau of Health Professions (BHPr), Division of Medicine and Dentistry (DMD), grant number R18HP15127. The content and conclusions of this manuscript are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by the U.S. government, HHS, HRSA, BHPr, or the DMD.
BL is supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under award number K01AT00896
Footnotes
Supplemental Information
Supplemental Tables S1.-S3.
Contributor Information
Michele Maiers, Wolfe-Harris Center for Clinical Studies, Northwestern Health Sciences University, Bloomington, MN, USA.
Jan Hartvigsen, Department of Sports Science and Clinical Biomechanics, and Nordic Institute of Chiropractic and Clinical Biomechanics, Campusvej 55, 5230 Odense M, Denmark.
Roni Evans, Integrative Health & Wellbeing Research Program at the Earl E. Bakken Center for Spirituality & Healing, University of Minnesota, 420 Delaware Street SE, Minneapolis, MN, USA.
Kristine Westrom, Northwestern Health Sciences University, Bloomington, Minnesota, USA..
Qi Wang, Clinical and Translational Science Institute, University of Minnesota, 717 Delaware St SE #140-26, Minneapolis MN USA.
Craig Schulz, Integrative Health & Wellbeing Research Program at the Earl E. Bakken Center for Spirituality & Healing, University of Minnesota, 420 Delaware Street SE, Minneapolis, MN, USA.
Brent Leininger, Integrative Health & Wellbeing Research Program at the Earl E. Bakken Center for Spirituality & Healing, University of Minnesota, 420 Delaware Street SE, Minneapolis, MN, USA.
Gert Bronfort, Integrative Health & Wellbeing Research Program at the Earl E. Bakken Center for Spirituality & Healing, University of Minnesota, 420 Delaware Street SE, Minneapolis, MN, USA.
References
- 1.Thomas E, Peat G, Harris L, Wilkie R, Croft PR. The prevalence of pain and pain interference in a general population of older adults: cross-sectional findings from the North Staffordshire Osteoarthritis Project (NorStOP). Pain. 2004;110:361–8. [DOI] [PubMed] [Google Scholar]
- 2.Hartvigsen J, Christensen K, Frederiksen H. Back pain remains a common symptom in old age. a population-based study of 4486 Danish twins aged 70–102. Eur Spine J 2003;12:528–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med 2001;135:313–21. [DOI] [PubMed] [Google Scholar]
- 4.Makris UE, Fraenkel L, Han L, Leo-Summers L, Gill TM. Restricting back pain and subsequent mobility disability in community-living older persons. J Am Geriatr Soc 2014;62:2142–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Laslett LL, Quinn SJ, Winzenberg TM, Sanderson K, Cicuttini F, Jones G. A prospective study of the impact of musculoskeletal pain and radiographic osteoarthritis on health related quality of life in community dwelling older people. BMC Musculoskelet Disord 2012;13:168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hartvigsen J, Christensen K, Frederiksen H. Back and neck pain exhibit many common features in old age: a population-based study of 4,486 Danish twins 70–102 years of age. Spine (Phila Pa 1976). 2004;29:576–80. [DOI] [PubMed] [Google Scholar]
- 7.Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388:1545–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pasquale MK, Dufour R, Schaaf D, Reiners AT, Mardekian J, Joshi AV, et al. Pain conditions ranked by healthcare costs for members of a national health plan. Pain Pract 2014;14:117–31. [DOI] [PubMed] [Google Scholar]
- 9.Ortman JM, Velkoff VA, Hogan H. An Aging Nation: The Older Population in the United States - Population Estimates and Projections: U.S. Department of Commerce Economics and Statistics Administration; May 2014. Report No.: P25–1140. [Google Scholar]
- 10.Hill J, Lewis M, Papageorgiou AC, Dziedzic K, Croft P. Predicting persistent neck pain: a 1-year follow-up of a population cohort. Spine (Phila Pa 1976). 2004;29:1648–54. [DOI] [PubMed] [Google Scholar]
- 11.Itz CJ, Geurts JW, van Kleef M, Nelemans P. Clinical course of non-specific low back pain: a systematic review of prospective cohort studies set in primary care. Eur J Pain 2013;17:5–15. [DOI] [PubMed] [Google Scholar]
- 12.Carey TS, Garrett JM, Jackman AM. Beyond the good prognosis. Examination of an inception cohort of patients with chronic low back pain. Spine (Phila Pa 1976). 2000;25:115–20. [DOI] [PubMed] [Google Scholar]
- 13.Descarreaux M, Blouin JS, Drolet M, Papadimitriou S, Teasdale N. Efficacy of preventive spinal manipulation for chronic low-back pain and related disabilities: a preliminary study. J Manipulative Physiol Ther 2004;27:509–14. [DOI] [PubMed] [Google Scholar]
- 14.Senna MK, Machaly SA. Does maintained spinal manipulation therapy for chronic nonspecific low back pain result in better long-term outcome? Spine (Phila Pa 1976). 2011;36:1427–37. [DOI] [PubMed] [Google Scholar]
- 15.Wong JJ, Cote P, Sutton DA, Randhawa K, Yu H, Varatharajan S, et al. Clinical practice guidelines for the noninvasive management of low back pain: A systematic review by the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur J Pain 2017;21:201–16. [DOI] [PubMed] [Google Scholar]
- 16.Cote P, Wong JJ, Sutton D, Shearer HM, Mior S, Randhawa K, et al. Management of neck pain and associated disorders: A clinical practice guideline from the Ontario Protocol for Traffic Injury Management (OPTIMa) Collaboration. Eur Spine J 2016;25:2000–22. [DOI] [PubMed] [Google Scholar]
- 17.Chou R, Deyo R, Friedly J, Skelly A, Hashimoto R, Weimer M, et al. Nonpharmacologic Therapies for Low Back Pain: A Systematic Review for an American College of Physicians Clinical Practice Guideline. Ann Intern Med 2017;166:493–505. [DOI] [PubMed] [Google Scholar]
- 18.National Institute for Health and Care Excellence. Low back pain and sciatica in over 16s: assessment and management - NICE guideline [NG59]. November 2016. [cited 2017 June 25]; Available from: https://www.nice.org.uk/guidance/ng59 [PubMed]
- 19.Balthazard P, de Goumoens P, Rivier G, Demeulenaere P, Ballabeni P, Deriaz O. Manual therapy followed by specific active exercises versus a placebo followed by specific active exercises on the improvement of functional disability in patients with chronic non specific low back pain: a randomized controlled trial. BMC Musculoskelet Disord 2012;13:162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Maiers M, Bronfort G, Evans R, Hartvigsen J, Svendsen K, Bracha Y, et al. Spinal manipulative therapy and exercise for seniors with chronic neck pain. Spine J 2014;14:1879–89. [DOI] [PubMed] [Google Scholar]
- 21.Vihstadt C, Maiers M, Westrom K, Bronfort G, Evans R, Hartvigsen J, et al. Short term treatment versus long term management of neck and back disability in older adults utilizing spinal manipulative therapy and supervised exercise: a parallel-group randomized clinical trial evaluating relative effectiveness and harms. Chiropr Man Therap 2014;22:26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bergman TF, Peterson DH, Lawrence DJ. Chiropractic Technique. New York: Churchill Livingstone; 1993. [Google Scholar]
- 23.Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976). 2000;25:2940–52; discussion 52. [DOI] [PubMed] [Google Scholar]
- 24.Roland M, Fairbank J. The Roland-Morris Disability Questionnaire and the Oswestry Disability Questionnaire. Spine (Phila Pa 1976). 2000;25:3115–24. [DOI] [PubMed] [Google Scholar]
- 25.Vernon H, Mior S. The Neck Disability Index: a study of reliability and validity. J Manipulative Physiol Ther 1991;14:409–15. [PubMed] [Google Scholar]
- 26.Knudtson MD, Klein BE, Klein R. Biomarkers of aging and falling: the Beaver Dam eye study. Arch Gerontol Geriatr. 2009;49:22–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Guralnik JM, Simonsick EM, Ferrucci L, Glynn RJ, Berkman LF, Blazer DG, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol 1994;49:M85–94. [DOI] [PubMed] [Google Scholar]
- 28.Guralnik JM, Ferrucci L, Simonsick EM, Salive ME, Wallace RB. Lower-extremity function in persons over the age of 70 years as a predictor of subsequent disability. N Engl J Med 1995;332:556–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Maiers MJ, Hartvigsen J, Schulz C, Schulz K, Evans RL, Bronfort G. Chiropractic and exercise for seniors with low back pain or neck pain: the design of two randomized clinical trials. BMC Musculoskelet Disord 2007;8:94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rundell SD, Sherman KJ, Heagerty PJ, Mock CN, Jarvik JG. The clinical course of pain and function in older adults with a new primary care visit for back pain. J Am Geriatr Soc 2015;63:524–30. [DOI] [PubMed] [Google Scholar]
- 31.Skou ST, Roos EM, Laursen MB. A Randomized, Controlled Trial of Total Knee Replacement. N Engl J Med 2016;374:692. [DOI] [PubMed] [Google Scholar]
- 32.Ostelo RW, Deyo RA, Stratford P, Waddell G, Croft P, Von Korff M, et al. Interpreting change scores for pain and functional status in low back pain: towards international consensus regarding minimal important change. Spine (Phila Pa 1976). 2008;33:90–4. [DOI] [PubMed] [Google Scholar]
- 33.Manchikanti L, Singh V, Falco FJ, Benyamin RM, Hirsch JA. Epidemiology of low back pain in adults. Neuromodulation. 2014;17 Suppl 2:3–10. [DOI] [PubMed] [Google Scholar]
- 34.Hartvigsen J, Natvig B, Ferreira M. Is it all about a pain in the back? Best Pract Res Clin Rheumatol 2013;27:613–23. [DOI] [PubMed] [Google Scholar]
- 35.MacDermid JC, Walton DM, Avery S, Blanchard A, Etruw E, McAlpine C, et al. Measurement properties of the neck disability index: a systematic review. J Orthop Sports Phys Ther 2009;39:400–17. [DOI] [PubMed] [Google Scholar]
- 36.Pool JJ, Ostelo RW, Hoving JL, Bouter LM, de Vet HC. Minimal clinically important change of the Neck Disability Index and the Numerical Rating Scale for patients with neck pain. Spine (Phila Pa 1976). 2007;32:3047–51. [DOI] [PubMed] [Google Scholar]
- 37.Fritz JM, Hebert J, Koppenhaver S, Parent E. Beyond minimally important change: defining a successful outcome of physical therapy for patients with low back pain. Spine (Phila Pa 1976). 2009;34:2803–9. [DOI] [PubMed] [Google Scholar]
- 38.Gatchel RJ, Mayer TG. Testing minimal clinically important difference: consensus or conundrum? Spine J 2010;10:321–7. [DOI] [PubMed] [Google Scholar]
- 39.Hurley MV, Walsh NE, Mitchell H, Nicholas J, Patel A. Long-term outcomes and costs of an integrated rehabilitation program for chronic knee pain: a pragmatic, cluster randomized, controlled trial. Arthritis Care Res (Hoboken). 2012;64:238–47. [DOI] [PubMed] [Google Scholar]
- 40.Villadsen A, Overgaard S, Holsgaard-Larsen A, Christensen R, Roos EM. Immediate efficacy of neuromuscular exercise in patients with severe osteoarthritis of the hip or knee: a secondary analysis from a randomized controlled trial. J Rheumatol 2014;41:1385–94. [DOI] [PubMed] [Google Scholar]
- 41.Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. J Am Geriatr Soc 2006;54:743–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Figure S1. Responder Analyses of Neck Disability Index
Note: More individuals in the short-term treatment group achieved ≥50% reduction in neck disability after 12 weeks of care, AOR=2.14 (1.01, 4.53), p=0.05
Supplemental Figure S2. Responder Analysis for Oswestry Disability Index (ODI)


