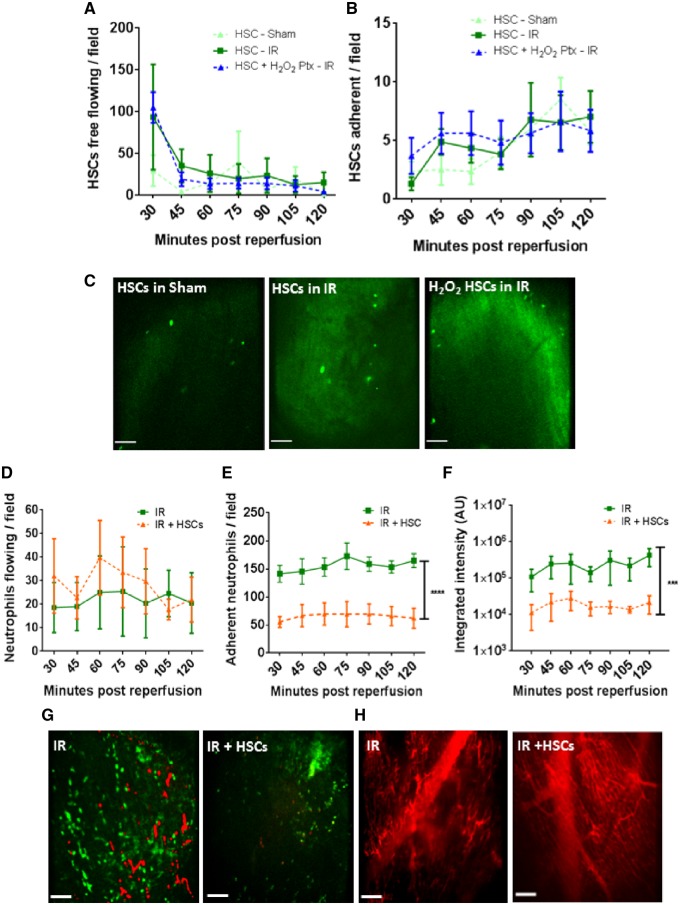
Figure 4.
Despite poor HSPC retention within IRI hearts, vasculoprotective effects are identified. (A) Twenty to 30 free flowing HSPCs observed circulating through myocardial microvessels at all time points in sham mice. However, in IRI hearts, an almost four-fold increase is noted at 30 min post-reperfusion. Pre-treatment of HSPCs with H2O2 does not enhance their homing to injured heart. (B) Adhesion of naïve or pre-treated HSPCs is not increased as a result of injury but gradually rises in all groups. (C) Representative intravital images show a similar retention of intra-arterially injected exogenous CFSE-labelled HSPCs in all groups. (D) HSPCs do not affect the free flow of neutrophils through the injured heart but do decrease (E) neutrophil adhesion (****P < 0.0001 vs. IR with significant differences at all time points; n ≥ 4). (F) Presence of platelet aggregates and microthrombi is also significantly reduced (***P < 0.001 vs. IR with significant differences at all time points; n ≥ 4). Two-way ANOVA with Sidak’s multiple comparison test used for all analysis. (G) Representative intravital images of injured heart showing a reduction in endogenous neutrophils and platelet presence when compared with non-treated injured hearts. Green, neutrophil (PE+anti-Gr-1ab); Red, endogenous platelets (APC+anti-CD41ab). (H) Improvement in capillary perfusion subsequent to cellular therapy as determined using FITC-BSA. Scale bars represent 100 µm.