Figure 3.
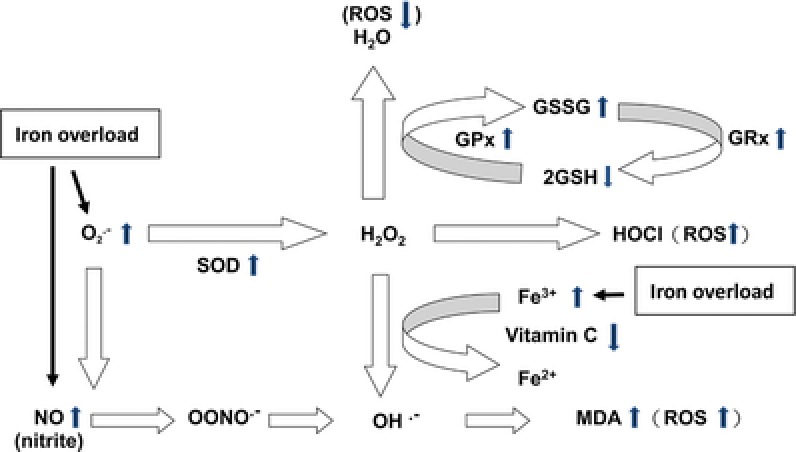
The possible metabolic pathway related to oxidative stress in patients with Hb H disease with iron overload. Iron overload causes the increase of superoxide () and nitric oxide (NO) in patients with Hb H disease. Increase of leads to compensatory increase of superoxide dismutase (SOD), and causes increase of hydrogen peroxide (H2O2) The increased hydrogen peroxides activate regulatory antioxidant system in the erythrocytes, resulting increased glutathione peroxidase (GPx), glutathione reductase (GRx), decreased reduced glutathione (GSH) and increased oxidized glutathione (GSSG) to reduce the excessive ROS. Furthermore, highly toxic, reactive hydroxyl radicals (OH.−) can be formed due to excessive free radicals (, NO, or H2O2), and leads to lipid peroxidation and generation of malondialdehyde (MDA). In addition, plasma vitamin C may be depleted due to iron overload and formation of excessive radicals (H2O2).
