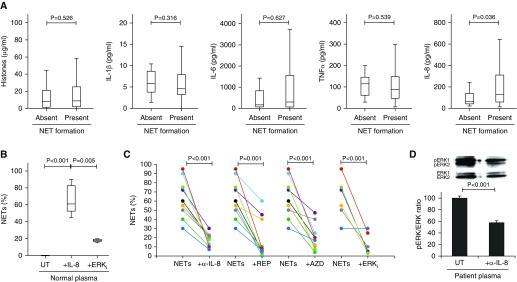
Figure 3.
IL-8 contributes to the neutrophil extracellular trap (NET)-forming capacity of critically ill patient plasma, and this capacity is partially blocked by anti–IL-8 and anti–mitogen-activated protein kinase (anti-MAPK) treatment. (A) Quantification of circulating factors known to stimulate NET formation (histones, IL-1β, IL-6, IL-8, and tumor necrosis factor [TNF]-α) in patient plasma on ICU admission demonstrated that IL-8 was elevated in patients who were able to induce NET formation (ANOVA; P < 0.05) (n = 341). (B) Incubation of 100 pg/ml IL-8 in normal plasma with normal healthy neutrophils for 4 hours induced NET formation compared with normal plasma alone (n = 10), which was blocked by inhibiting MAPK activation with U0126 (extracellular signal-regulated kinase inhibitor [ERKi]) (n = 3) (ANOVA; P < 0.05). (C) Preincubation of normal neutrophils with either anti–IL-8 monoclonal antibody (α-IL-8) (n = 10), reparixin (REP) (n = 10), AZD5069 (AZD) (n = 10), or MAPK inhibitor U0126 (ERKi) (n = 6) before treatment with plasma of patients with sepsis partially blocked NET formation (ANOVA; P < 0.05). (D) Western blot analysis of ERK activation (pERK/ERK ratio) in normal neutrophils incubated for 15 minutes with plasma of patients with sepsis preincubated without (UT) or with anti–IL-8 monoclonal antibody (α-IL-8) (n = 3) (ANOVA; P < 0.05).