Abstract
PURPOSE
To understand the role of Maryland Head Start (HS) programs in asthma care and identify resources and needs to improve health outcomes.
METHODS
A qualitative needs assessment was conducted with Maryland HS staff (n=35) and parents/caregivers of enrolled children with asthma (n=16) from all 14 grantee programs in Maryland. Focus group discussions and interviews addressed strengths and challenges in current asthma control and opportunities for integration of an asthma care program into HS services. Transcripts were thematically analyzed using a modified Framework approach.
RESULTS
HS programs actively communicate with families about asthma management and facilitate communication between families and primary care providers (PCPs). Both HS staff and families reported a strong trusting relationship allowing HS staff to provide asthma management support. HS needs strong linkages with supportive services and PCP offices to engage families, address environmental triggers, and educate staff. While families across the state report interest in peer education on asthma through HS, there were some region-specific asthma care barriers for urban and rural programs.
CONCLUSION
This needs assessment confirmed interest among all stakeholders in integrating asthma care through HS and identified communication strategies, supportive infrastructure, and addressing regional access to care as key elements for program design.
PURPOSE
Asthma is a chronic disease disproportionately affecting low-income minority children. Black, non- Hispanic children have nearly twice the asthma prevalence rate compared to other racial and ethnic groups (Akinbami, Moorman, Bailey, Zahran, King, et al 2012; CDC 2013). Of children with asthma who visit the emergency department, 48% reside in an urban area and 62% reside in the lowest-income communities (Wier, Yu, Owens, Washington 2013). Children under the age of 5 experience the greatest hospitalization rates for asthma compared to other age groups (Walsh, Kelly, Morrow 1999). Asthma also has negative impacts on child development, physical activities, and school attendance (CDC 2016; Clack 2010; Gern, Rosenthal, Sorkness, Lemanske Jr 2005). Over half of missed school days are asthma-related and significant absenteeism from school is correlated with delayed school readiness and less optimal academic achievements (Davis, Gordon, Burns 2011; Moonie, Sterling, Figgs, Castro 2006). Finally, asthma may negatively impact family income, as parents or caregivers need to miss work to care for sick children (Gern, Rosenthal, Sorkness, Lemanske Jr 2005).
Head Start (HS) is a federal preschool program for low-income children that has the potential to uniquely address the needs of hard-to-reach high risk children with asthma. HS is mandated to support the health of students and has existing programs to improve health for low-income children and families and addressing health inequities and health promotion efforts (Head Start Early Childhood 2018). Health and parent involvement are already key components of HS’s mission and their “Parent, Family, and Community Engagement Framework” emphasizes the provision of robust services for families at HS programs and through home visiting (Head Start Early Childhood 2018). Through positive and goal-oriented relationships, this framework aims to improve child and family outcomes (health, school success, family relationships) through program partnerships, teaching and learning, and continuous quality improvement (Head Start Early Childhood 2018). Given the explicit focus of HS on improving the health and well-being of low-income children, HS would be a valuable community setting for improving asthma outcomes in low-income children.
While HS has a history of intervening on issues related to lead exposure and oral health, there have been limited policies and programs on asthma care, with variable resource distribution. Moreover, HS programs are run by different grantee agencies that may have variable policies and practices when it comes to supportive services for asthma care. National HS Performance Standards do not currently provide explicit guidelines when it comes to asthma management apart from having medication administration authorization and appropriate medication on site for children that may need it during program hours- the usual standards for a wide range of health conditions. Before asthma outcomes can be addressed in Head Start, it is essential to better understand how existing policies and resources at individual programs can best be utilized to enhance asthma care programs. Additionally, the organizational and community contexts that could influence implementation of asthma programs in HS also need to be identified. Systematic assessments of contextual barriers and facilitators for implementing new interventions are increasingly recognized as an important step in successful program planning (Damschroder, Aron, Keith, Kirsh, Alexander, et al. 2009). The Consolidated Framework for Implementation (CFIR) outlines five domains to consider when identifying barriers and facilitators for implementation: outer setting (administration, setting, resources) inner setting (team characteristics, culture, communication), individual (staff knowedge, attitudes and beliefs) intervention characteristics and process of implementation.
In this paper, we report the results of an asthma care needs assessment using qualitative methods based on the CFIR framework in HS programs across Maryland in order to inform the design of an asthma care and education program that would be implemented in HS. The objectives of this study were to: 1) evaluate Maryland HS programs’ current role in supporting families with asthma management and care coordination; 2) identify opportunities and challenges for delivering an asthma care intervention through HS; and 3) to understand communication pathways between families, HS programs, and primary care providers (PCPs) for asthma care.
METHODS
In this formative qualitative study, we conducted one time focus group discussions (FGDs) and in-depth interviews (IDI) with Head Start staff, administrators, and parents/caregivers of enrolled children with asthma. FGDs and IDIs lasted approximately 1 hour and were conducted in a private space with consented participants only. Four FGDs took place during the Maryland Head Start Association (MHSA) Fall Conference in December 2015. The MHSA Fall Conference is open statewide to HS staff and family members. The research team collaborated with MHSA to send out recruitment emails to all registered conference attendees at multiple time points leading up to the conference. The exact number of individuals who received this information via email is unknown as the research team was only directly contacted by interested individuals. Interested participants received additional details over the phone or during the conference and consented prior to participating in a FGD or IDI. The MHSA provided time during breakout sessions of the Fall Conference for FGDs to take place. Three additional FGDs took place at the location of HS programs in two counties, two were composed of HS staff exclusively and one solely with parents/caregivers of enrolled children with asthma. IDI were conducted with three additional HS staff members at their respective HS program location.
Participants
All HS staff were eligible to participate either at MHSA or their HS locations. All family members at MHSA were also eligible to participate, regardless of their child’s asthma status. The single FGD at a HS program with family members only included parents/caregivers of enrolled children who had an asthma diagnosis. Participants in IDIs were selected based on the relevance of their position to asthma control programs in HS using purposeful sampling. The sample included participants from all 14 active HS grantee agencies in the state of Maryland, which together serve nearly 9000 children. One additional HS grantee agency existing in Maryland was not represented due to suspension of funding and closure of all HS program activities during the course of interviews.
Data collection
FGDs were facilitated by an experienced facilitator who was member of the study team (JCK) following a semi-structured interview guide informed by the Consolidated Framework for Implementation Research (CFIR) (Damschroder, Aron, Keith, Kirsh, Alexander, et al. 2009). The CFIR outlines 26 constructs that are associated with effective implementation in published studies, organized under five domains: intervention characteristics, outer setting, inner setting, characteristics of individuals, and process of implementation (Damschroder, Aron, Keith, Kirsh, Alexander, et al. 2009). The developers intended the CFIR to enable comparison of “what works” in implementation across contexts (Damschroder, Aron, Keith, Kirsh, Alexander, et al. 2009), and it is now one of the most widely used implementation research frameworks (Kirk, Kelley, Yankey, Birken, Abadie, Damschroder 2016). Topics covered included asthma needs within HS, current asthma care strategies and resources, engagement of families, housing and environmental trigger needs, family needs, and coordination with PCPs. Participants were aware that one of the goals of the needs assessment was to inform the development of a statewide asthma management program for Maryland HS. Additional topics emerged during the course of interviews and were added to the FGD guide including HS physical environment with specific attention to asthma triggers and family centered challenges with managed care organizations. A total of 51 HS staff and parents/caregivers were interviewed. An additional 6 HS staff consented to be interviewed, but were unable to be contacted to complete an IDI or FGD. FGDs and IDIs were audio-recorded for transcription. During some interviews, staff declined audio recording and detailed notes were taken. Field notes were also taken during audio recorded interviews. All participants were asked to complete a demographic survey. The study was approved by Johns Hopkins School of Medicine Institutional Review Board (protocol # IRB00076727).
Analysis Strategies
Data analysis followed an adapted Framework approach (Ritchie, Spencer 1994). Transcripts were coded by a single coder (ER) using NVIVO according to a codebook that was agreed upon by all investigators after reaching data saturation from FGDs and IDIs (Nvivo 2012). ER developed the codebook inductively following familiarization with the data and through discussions with all investigators to further refine and resolve discrepancies. After coding, thematic memos were developed for each code by ER and JCK. The first set of memos focused on one of three stakeholders—HS families, HS staff, and PCPs—and summarized data related to their needs, barriers, facilitators and resources related to asthma care for HS children. Additional memos summarized the existing communication pathways between stakeholders and participants’ recommendations for improving communication to facilitate asthma care. After memos were reviewed by MNE and JCK, tables were developed by ER and JCK to summarize findings with representative quotes and to streamline themes and findings.
RESULTS
Focus group and interview participants were 92% female, 37% Caucasian and 35% African American (N=51, see Table 1). Demographic surveys were completed by 41 (80%) Head Start staff and caregivers. While 43% of respondents had a bachelor’s degree or higher, 20% reported only a high school education. Participants’ role in Head Start included parent or family members (31%), teachers and teacher assistants (25%), and family service coordinators (14%). Other HS staff participants included health coordinators, nurses, directors, family resource workers, education specialists, and child development manager.
Table 1.
Demographic Information (n=51)
| Characteristic | N (%) |
|---|---|
| Gender | |
| Male | 4 (8.0%) |
| Female | 47 (92.0%) |
| Age | |
| 18–30 years | 8 (15.7%) |
| 31–50 years | 20(39.2%) |
| 51–70 years | 13 (25.5%) |
| Unknown | 10 (19.6%) |
| Race | |
| Caucasian | 19 (37.3%) |
| African American | 18 (35.3 %) |
| Hispanic, Latino, or Spanish Origin | 1 (2.0%) |
| Other | 1 (2.0%) |
| More than 1 race | 3 (5.9%) |
| Unknown/Prefer not to answer | 9 (17.7%) |
| Education | |
| Some high school | 3 (5.9%) |
| High School Diploma/ GED | 8 (15.7%) |
| Associate Degree | 5 (9.8%) |
| Bachelor’s Degree | 11 (21.6%) |
| Post Graduate | 11 (21.6%) |
| Other | 2 (3.9%) |
| Unknown | 11 (21.6%) |
| Head Start Role | |
| Family Service Coordinator | 7 (13.7%) |
| Teacher | 12 (23.5%) |
| Teacher’s Assistant | 1 (2.0%) |
| Health Coordinator | 2 (3.9%) |
| Nurse Manager | 1(2.0%) |
| Parent/Family Member | 16 (31.4%) |
| Head Start Director | 4 (7.8%) |
| Other | 8 (15.7%) |
| Length with Head Start | |
| <1 year | 2 (3.9%) |
| 1–2 years | 10 (19.6%) |
| 3–5 years | 4 (7.8%) |
| 5–10 years | 10 (19.6%) |
| 10+ years | 8 (15.7%) |
| Unknown or Not Applicable1 | 17 (33.3%) |
Note: Unknown data is attributed to participants in the pilot focus group (n=8) not being surveyed on their detailed demographic information and surveyed participants choosing to not answer all questions.
Some participants, specifically focus groups comprised of solely Head Start parents, were not asked this question contributing to a higher number of unknown responses or non-applicable.
Communication Pathways for Asthma Care
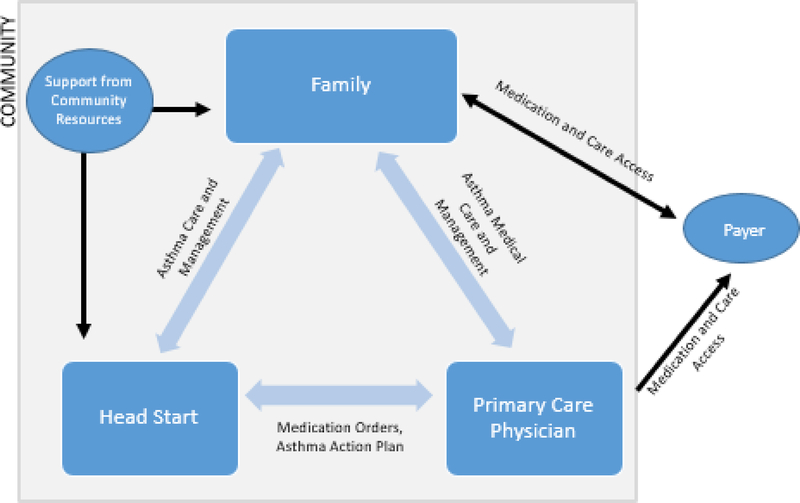
Figure 1 illustrates the existing communication pathways and relationships between the three major stakeholders: families, HS programs, and PCPs for asthma care. All three stakeholder groups communicate within the community setting, while the payer provides critical access to medical care and prescription drug coverage which is relied upon not only by the families, but also by the treating PCP. Within the community, participants identified limited awareness of existing resources that can provide supportive services to both families and HS programs in asthma care. These supportive services included educational resources or tangible goods such as integrated pest management or cleaning supplies. HS families primarily receive support in asthma care from HS and their PCPs. The PCP provides medical care and a treatment plan for the family to follow and the HS program supports the family in following the plan either by providing educational resources or helping with navigating the health care system and locating appropriate medical care. HS will also provide acute asthma care on site should a child have an exacerbation at the program. Some HS programs communicate directly with PCP offices in their community to request medication orders and a confirmed asthma action plan from the treating PCP for the child’s asthma care. Each stakeholder group reported strengths and challenges with current asthma care, self-management practices, and within communication pathways that present potential opportunities for intervening to improve asthma care. These findings are summarized in Table 2 and are described in the following sections, organized by stakeholder group.
Figure 1:
Relationships between Families, Head Start Programs, and Primary Care Physicians for Asthma Care Conceptual diagram of the asthma management network existing in Maryland HS programs and how it is connected within the local community and external infrastructures such as the payer.
Table 2.
Opportunities and challenges for supporting asthma management through Head Start Programs: Summary of primary points that arose from qualitative interviews with HS staff and parents/caregivers of enrolled children.
| Agency/ Partner | Strengths and Opportunities | Needs and Challenges |
|---|---|---|
| Head Start Programs | • Engaged in helping families with asthma management and relationship with primary care provider • Can provide some asthma care on site • Have policies for some environmental issues that trigger asthma in the classroom • Can provide smoking cessation training or counseling on second hand smoke • Assists families in advocating for themselves with the PCP • Staff often develop strong relationships with families • Programs have successful family education programs |
• Faces challenges engaging some parents in supplemental events • Some environmental triggers present at sites (e.g., bleach for cleaning, second-hand smoke carried on children’s belongings) • Staff need training on recognizing asthma symptoms and administering medications • High staff turnover |
| Families | • Some parents are proactive in communicating with the Head Start teacher about their child’s asthma • Families often develop strong relationships with and trust Head Start staff • Participate in Head Start parent education programs when it’s convenient and incentives are provided such as food and childcare during educational programs • Interested in peer education about asthma |
• Don’t always provide information about child’s health to Head Start • Some parents have low health literacy and don’t understand diagnosis • Some families perceive asthma to be common and not a serious concern • Some parents don’t know what questions to ask doctors or how to advocate for their child • Lack knowledge on symptom recognition, medication administration, and trigger • Children staying in multiple homes complicates asthma medication management |
| Primary Care Providers | • Can help families navigate insurance coverage and fill prescriptions • Attempt to reduce the need for specialty care |
• Health education from providers is often insufficient or rushed • Limited access to PCP for families in rural areas and families that don’t speak English • Delays in providing AAPs and on-site medications; limited awareness of the importance of AAPs to Head Start |
| Payer | • Wide access to coverage for children • Prescription drug coverage- no or low cost |
• Insurance won’t cover multiple prescriptions required to have on hand at home and at school • Coverage can lapse when families move or income increases |
Head Start Programs: Strengths and Challenges in Asthma Care
HS staff felt they had very close relationships with families and that HS provides a source of support for asthma case management, particularly for families that were facing barriers with their PCP. Staff members described facilitating appointments for families as well as reaching out to PCPs during acute exacerbations. There was recognition that not all programs were actively facilitating communication between families and PCPs and that perhaps this is something that should be done more universally. One HS program that utilizes health coordinators described how teachers and families are involved in planning for the child’s asthma care in advance of the school year and when absenteeism is frequent for the child due to exacerbations. In this program, enrolling families consent to have the health coordinator communicate with the child’s PCP directly to collaboratively resolve issues or discuss the child’s health:
“Teachers come in and then we create together a health plan specifically for that child and then everything is sent to the family doctor. Then the family doctor signs off on it and makes sure that everything that we put in there is correct” (Disability Specialist, FGD4)
HS programs expressed interested in building relationships with clinics that cared for a large proportion of enrolled students. Most of Head Start’s low-income families are enrolled in Medicaid insurance and were often limited to community providers that accept Medicaid. Staff at some programs described how they had already established rapport with a clinic that serves predominantly Medicaid patients and this greatly helped to facilitate completion of asthma-related paperwork or medication refills for the child. Staff at HS programs that had not established relationships with PCP offices noted this as a barrier to supporting asthma management.
A barrier to asthma care identified by HS staff at all locations included insufficient resources for staff training on asthma or access to nurses. HS staff felt there was a lack of asthma education not only on how to provide treatment, but also with recognizing asthma symptoms. Staff felt concerned or anxious that they would be in a classroom and not be able to tell when a child was having an asthma attack due to their lack of knowledge:
“I don’t have anybody in my family that has asthma, I’m not very familiar with asthma, so I really honestly depend on people who are familiar with what asthma looks and sounds like to let me know.” (Teacher, FGD2)
In addition to asthma education for all staff, HS programs reported a need for repeated education during the school year due to high turnover rates. HS staff felt that when asthma education was provided, there was a possibility there would be gaps in asthma knowledge due to newer staff joining partway through the school year. Some staff also expressed a desire to have refresher trainings during the year for staff and families in order to reinforce messages regarding asthma symptoms and severity.
Some HS programs were able to overcome asthma care barriers through focused use of resources or development of specific policies to care for asthma. For example, one program outlined their policy of nurse case managers contacting the PCP when acute care was provided at HS. The nurse case manager would then discuss a plan for treating the child and also how to identify and address any potential environmental triggers in HS that may have caused the exacerbation.
Working with Families: Strengths and Challenges to Asthma Care
Participants described strong relationships that often develop between families and HS staff. The high degree of trust many families have with HS staff presents an opportunity for families to accept asthma education and support provided through the HS program. Participants also said that parental engagement in after-school activities, such as health education events, can be high, particularly when the events are perceived by families to be fun—with games, “make and takes” or clothing exchanges—or social, so that they “get something out of it in terms of just being around some other people who are sharing the same thing” (Health Coordinator, IDI). Head Start staff noted several approaches they have successfully used to reduce barriers for families to participate in events, including selecting the most preferred times (usually evening), providing childcare, and providing meals. Another effective parent engagement strategy at one program was a “passport book” that gave parents credit for attending events that they could then trade for consumer items.
Participants identified parental engagement in their child’s care as critical to asthma care and at home management, including proactively communicating with school staff and healthcare providers. Among caregivers of children with asthma, some described how they are already proactive in managing their child’s asthma and communicating with Head Start teachers or social workers regarding their child’s asthma:
“I’ve found that communication with the educators is extremely important with [my child]. Because I’ll say well, the weather . . . the humidity is high and he’s going to be outside and I already gave him the Benadryl and I already gave him the hydroxy. . . and I already gave him this and so you’ll just have to watch him.” (Caregiver, FGD 7)
At the same time, participants noted that many families have barriers preventing them from being engaged in their child’s care. A frequently mentioned barrier to engagement was caregivers not knowing how to advocate for their children with healthcare providers or insurance companies. Time constraints were another factor perceived to limit family engagement. For example, a staff member from a program in rural Western Maryland noted that most parents commute long distances to work and don’t have time in the morning to complete nebulizer treatments.
The most common barrier for families’ asthma management noted by participants was low levels of health literacy and/or understanding of asthma. Many described parents as lacking knowledge about their child’s diagnosis, or what steps they should take to manage their child’s asthma. Participants suggested that parents need more education in three areas in particular: symptom recognition, medication administration, and reducing triggers. Parents and HS staff recommended that health education for parents should be made understandable, with limited “medical jargon.” Participants frequently noted the potential for families to feel overwhelmed during rapid education received in a provider’s office, and to not know what questions to ask. Family members responded positively to the option of a peer support for asthma control, a form of education that could be more accessible and relatable: “that’s how we learn about information . . . from gossip and from each other” (Caregiver, FGD 7).
A barrier related to low-levels of knowledge identified by many participants is families not underestimating the potential for serious health risks. Several participants described parents as lacking concern about asthma:
“Because of their lack of education, they don’t take [asthma] as serious as it should be . . . they still smoke and say they don’t want the child to have treatment at school . . . I just don’t think some of them realize that their child could die from something like this.” (Family Service Coordinator, FGD 5)
Additional factors that participants said contribute to lack of concern about asthma included perceiving asthma to be a common “everyday thing,” and having more pressing issues in the family such as drug abuse or financial strain.
Working with Primary Care Physicians: Strengths and Challenges to Asthma Care
HS staff viewed PCPs as critical partners in assuring children’s long term health and academic success. Staff from some HS programs reported that their programs had developed strong relationships with pediatricians serving HS students. One Health Manager described having only “a handful of pediatricians and I talk to all of them almost every day” (FGD4). Another program described plans for the subsequent year to have health coordinators visit clinics in person and provide a house plant as a means of introduction and an opportunity to review HS specific health forms. Positive relationships with PCPs facilitated activities such as medication refills and timely completion of forms.
There was an expressed interest in having a regularly scheduled time when families could see specialty care providers in their area, particularly because of transportation limitations. One parent from a rural county described having specialists visit their area once a week or once a month on a set schedule. Transportation to access medical care seems to be an issue in urban, suburban, and rural areas for differing underlying reasons. Urban areas may be limited by public transportation if PCPs are not located within a walkable distance, while rural area families described limitations with having a single vehicle in the household or limited access to public transport. There are also gaps in provision of interpreter services to facilitate care within clinics as well as soliciting about transportation barriers or other access to care issues.
When asked about challenges communicating with PCPs, HS staff most frequently mentioned issues with asthma action plans (AAPs) and a perception that PCPs were unaware of differences between HS and public schools. Staff detailed experiences of AAPs being returned unsigned, with significant delays following a request, or the incorrect paperwork being completed. While HS staff recognize that clinicians have heavy patient loads, staff expressed uncertainty about PCPs knowledge that children are unable to attend the HS program until all documentation and medicines for asthma are received and reviewed. Navigating insurance policies also presented challenges for HS staff and families, particularly with regard to accessing asthma medicines and spacers. HS staff and families detailed experiences of being denied by insurance to receive a second inhaler or spacer for the purpose of having medicine at the HS program. It is the policy of HS that medicines remain on site and are not taken to and from home on a daily basis.
Families felt that PCPs were not providing adequate asthma education or time during regular appointments. Parents described being “rushed out of the door” with overwhelming amounts of information that they struggled to fully comprehend, such as understanding the differences between controller and rescue medications.
“The doctor starts telling us to do this, this, this and this, and if we don’t have this notepad writing it down and dictating everything that he says they get lost.” (Parent, FGD 5)
Additionally, families felt that care providers gave overly technical descriptions and information that they were not always able to interpret. Families did not feel they could ask questions in a clinical setting both due to the feeling of being rushed out and also since they did not want to experience judgement for not understanding the information.
“Sometimes educated folks forget and they speak up here. They speak at a higher level and then people can’t understand you. Well, people are not always going to tell you that I have no idea what the heck you talking about…because they don’t want to be embarrassed or threatened” (Parent, FGD 7)
Recommendations for Asthma Care Program Implemented in National Head Start
Panel 1 presents design recommendations for a nation-wide HS asthma care program informed by the results of this needs assessment. Recommendations for an asthma care intervention would include peer community health workers (CHWs), supportive services for HS staff, and improved communication between HS, families, and PCPs. CHWs would educate families and link them with community services, staff support would improve their knowledge and skills for managing and caring for asthma in the classroom, and communication between HS and PCPs can help families address barriers accessing care and managing paperwork. Designating peer CHWs rather than CHWs outside of HS would prove particularly valuable as it could provide buy-in from HS programs to participate in the intervention as it supports the “Parent, Family, and Community Engagement Framework” through provision of job training services for families that have relevant experiences and connections with other HS families. Job training services for caregivers of children with asthma may also help address economic and psychosocial barriers to optimal asthma care and management. These recommendations are applicable across the country as HS serves a low-income population that faces similar challenges. Tailoring intervention delivery for urban, suburban, or rural settings can be implemented in order to maximize reach. For example, transportation and access to PCPs is a barrier in all areas, however public transport and quantity of PCPs is greater in urban areas versus rural, so strategies to help improve access to care will differ.
Panel 1. Recommendations for design of a nation-wide Head Start asthma care and education program.
Peer community health workers conduct home visits to provide education, home environment assessment, and referral to asthma management resources
Supportive services and asthma training for Head Start staff
Improved communication strategies between Head Start staff, families, and PCP offices
Job training services for parents to address socioeconomic barriers to asthma management and child health
DISCUSSION
The results of this qualitative needs assessment confirm that HS programs are well positioned to help families of preschool-aged children improve asthma care. Existing assets within HS programs that can be leveraged for an asthma acute care intervention include trusting relationships and frequent contacts with parents/caregivers, and existing processes to manage and intervene with preventive health issues. Some HS programs have already established strong communication channels with PCPs to help families navigate medical and paperwork needs. At the same time, resource and time constraints exist for all parties—HS staff, PCPs and families—and HS staff and families need additional education on asthma care.
The findings from this needs assessment about the asthma education needs of HS staff are consistent with research in other school settings. One study in Georgia examining teaching staff’s asthma knowledge and perception of asthma training found that teachers felt unprepared to manage asthma and yet they were expected to administer medication and take on this role due to insufficient nurses in public school systems, even though it is outside their scope of practice with almost 15% of staff administering medication without any training (Neuharth-Pritchett & Getch 2001). In addition to education on asthma care, HS staff also require support on other aspects related to asthma care coordination and management and on best strategies for educating HS families. Another study looking specifically at HS staff found that coordination of care, unreported asthma, and issues with medication administration were common challenges (Garwick, Seppelt, Riesgraf 2010). HS staff reported discrepancies between parent and PCP reports related to the child’s asthma care as well as parents having inadequate information about asthma care and management including recognizing severity, how to handle acute episodes, and prevention information (Garwick, Seppelt, Riesgraf 2010). Providers themselves may also need education around insurance coverage barriers and patient-centered communication (Mowrer, Tapp, Ludden, Kuhn, Taylor, et al 2015), which HS family coordinators could provide.
In addition to strengthening the asthma care knowledge of staff, a HS asthma care intervention must address the asthma education needs of families. Previous research has shown that caregivers of children with asthma have foundational knowledge gaps when it comes to asthma including under recognition of asthma severity, viewing asthma as acute and not chronic (Archibald, Caine, Ali, Hartling, Scott 2015), and suboptimal knowledge about asthma medications and their use (Callaghan-Koru, Riekert, Ruvalcaba, Rand, Eakin 2018). These knowledge gaps impact the way in which families manage asthma, often leading families to focus on responding to acute crises rather than prevention through long-term management (Garwick, Seppelt, Riesgraf 2010). Kakumanu and colleagues completed a review in 2017 to identify consensus recommendations in school-based asthma care and found that in addition to asthma education and environmental remediation, coordinated communication between the school and clinical care providers to support children with asthma was key in reducing exacerbations and improved asthma management including improved availability of asthma medicines (Kakumanu, Antos, Szfler, Lemanske Jr 2017). In a set of focus groups conducted with low-income minority families, Bellin and colleagues found that asthma management is complex and is most often shared across multiple caregivers (Bellin, Land, Newsome, Kub, Mudd, et al 2017). Families who are managing childhood asthma in the context of poverty have a demonstrated need for recurring asthma education and coordinated efforts between caregivers and PCPs (Bellin, Land, Newsome, Kub, Mudd, et al 2017). This coordination of asthma care and management is needed in order to manage asthma that tends to have a greater level of complexity and limitations related to at home management such as, housing instability, food insecurity, and community violence (Bellin, Land, Newsome, Kub, Mudd, et al 2017). Families living in poverty also have greater social stressors that can affect not only asthma management, but morbidity and quality of life as well (Bellin, Land, Newsome, Kub, Mudd, et al 2017).
A limitation of this qualitative assessment is that we only conducted interviews and FGDs with HS staff and family members and were unable to include PCPs. While some PCPs were contacted, interviews were not able to be scheduled due to lack of response and limited availability of PCPs. While this study did contact representatives from every HS program in the state of Maryland, the distribution of participants was not equal, so it is possible additional subjects or topics may have been brought up if there would have been additional participants from certain parts of the state.
LESSONS LEARNED
Head Start programs can help deliver health promotion activities to low-resource, high-risk families who experience health disparities. The results from this assessment suggest that health programs that will be implemented in Head Start or similar educational programs, should engage in coordinated efforts between families, the educational program, and primary care providers to effectively care for asthma. When engaging with community based organizations, it is best to visit site locations, to ensure public health professionals are getting a comprehensive image of how a program should be planned or evaluated within the community agency. Moreover, when looking at implementing programs across a broad geographic area, such as a state or country, it is important to obtain representation from urban, suburban, and rural populations who may experience similar challenges as a low-income high risk population, but experience some different barriers in asthma care.
This study used the Consolidated Framework for Implementation Research (CFIR) to guide development of interview and discussion guides. The CFIR is a typology of factors that influence implementation that are identified in theories and empirical studies (Damschroder, Aron, Keith, Kirsh, Alexander, et al 2009). While the CFIR specifies 26 unique constructs, these were too many to address directly in this exploratory assessment. Instead, the guides included questions or prompts for each of the five domains under which the CFIR constructs are organized: intervention characteristics, outer setting, inner setting, characteristics of individuals, and process. Referencing the CFIR during guide development and revisions ensured that the interviews elicited the full range of factors relevant to asthma care program implementation.
CONCLUSIONS
Families of children with asthma that are served by HS programs face many challenges in understanding the prevention and treatment of asthma exacerbations, managing complex administrative and paperwork requirements, and prioritizing asthma care in the presence of other concerns and stressors. HS programs provide a trusted and consistent point of contact that can be leveraged for supporting families in asthma care. The results of this study demonstrate that asthma care for Head Start children must engage a complex network where asthma is managed by HS staff, parent/caregiver, and the PCP. Although communication and coordination challenges exist within Head Start-Caregiver-PCP communication pathways, there are ways in which this network can effectively function for coordinated asthma care. Evaluation and program planning efforts should target all three stakeholder groups to maximize efforts to improve asthma care. By improving communication strategies and establishing supportive infrastructures—not only in the child’s home, but also in places where children learn and play—a HS asthma care program provides a promising model for improving asthma outcomes for the most at-risk children.
Supplementary Material
Highlights.
Asthma care can be integrated into Head Start with supportive infrastructure
Integrated HS asthma care programs will need to address regional barriers
HS programs actively engage on health and have trusting family relationships
Communication pathways between HS, families, and PCPs need strengthening
Families have interest in peer education for ongoing asthma education/support
Acknowledgments
Funded by National Institutes for Health Grant # U34 HL130752
Biography
Elizabeth Ruvalcaba
Research Manager at Johns Hopkins Adherence Research Center in the Division of Pulmonary and Critical Care Medicine, Department of Medicine at Johns Hopkins University. Ms. Ruvalcaba received her Master of Science in Public Health from the Johns Hopkins Bloomberg School of Public Health with a focus on Health Behaviors and Education. She manages several NIH and other sponsored trials looking at improved clinical management, adherence, and integration of care management in asthma, COPD, sickle cell disease, and cystic fibrosis.
Jennifer Callaghan-Koru
Assistant Professor of Public Health in the Department of Sociology, Anthropology, and Health Administration at the University of Maryland, Baltimore County. Dr. Callaghan-Koru received a PHD and MHS from the Johns Hopkins Bloomberg School of Public Health. The focus of Dr. Callaghan-Koru’s research is identifying and evaluating approaches for improving access to evidence-based interventions and reducing disparities for mothers and children in both high and low-resource settings. Her research utilizes qualitative and quantitative methods and draws from implementation science, social science, and program evaluation disciplines.
Cynthia Rand
Professor of Medicine in the Division of Pulmonary and Critical Care Medicine at the Johns Hopkins School of Medicine and Founder of the Johns Hopkins Adherence Research Center. She received her undergraduate degree from the University of California at Berkeley and her doctoral degree from the Johns Hopkins University. Her particular areas of research interest are the social-behavioral mediators of asthma management in minority communities and adherence issues in pulmonary medicine. She has been the PI of multiple pediatric intervention trials focused on improving adherence and reducing childhood asthma morbidity as well as reducing racial and ethnic health disparities.
Michelle Eakin
Associate Professor in the Division of Pulmonary and Critical Care Medicine at the Johns Hopkins School of Medicine, Co-Director of the Johns Hopkins Adherence Research Center. Dr. Eakin received her undergraduate degree from Brigham Young University and her Ph.D. in Clinical Psychology from University of Houston. Dr. Eakin’s research focuses on asthma disparities, COPD, adherence interventions, and qualitative/quantitative methods. She is particularly interested in studying the dissemination and implementation of interventions into community settings to reduce health disparities.
Footnotes
Declaration of Conflicting Interests Statement: The authors report no conflicts of interest. The authors alone are responsible for the content and writing of the paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Reference
- 1.Akinbami LJ, Moorman JE, Bailey C, Zahran HS, King M, et al. (2012). Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010 NCHS data brief, no 94. Hyattsville, MD: National Center for Health Statistics; 2012. [PubMed] [Google Scholar]
- 2.Archibald MM, Caine V, Ali S, Hartling L, Scott SD. (2015). What is left unsaid: an interpretive description of the information needs of parents of children with asthma. Res Nurs Health, 381, 19–28. [DOI] [PubMed] [Google Scholar]
- 3.Bellin MH, Land C, Newsome A, Kub J, Mudd SS, et al. (2017). Caregiver perception of asthma management of children in the context of poverty. J Asthma, 542, 162–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Callaghan-Koru JA, Riekert KA, Ruvalcaba E, Rand CS, Eakin MN. (2018). Home Medication Readiness for Preschool Children with Asthma. Pediatrics, 1423, epub [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Centers for Disease Control (CDC). (2013). Internet source cited 2019 Feb 14, Available from: https://www.cdc.gov/asthma/brfss/2013/child/tableC5.htm#modalIdString_CDCTable_0
- 6.Centers for Disease Control (CDC). (2016). Internet source cited 2017 Feb 14, Available from: https://www.cdc.gov/asthma/asthma_stats/default.htm
- 7.Clack G (2010). An offsite activity policy for asthma camp. Paediatric Nursing, 222, 22–26. [DOI] [PubMed] [Google Scholar]
- 8.Damschroder L, Aron D, Keith R, Kirsh S, Alexander J, Lowery J. (2009). Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implementation Science, 41, 50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Davis DW, Gordon MK, Burns BM. (2011). Educational Interventions for Childhood Asthma: A Review and Integrative Model for Preschoolers from Low-Income Families. Ped Nursing, 371, 31–8. [PubMed] [Google Scholar]
- 10.Garwick AW, Seppelt A, Riesgraf M. (2010). Addressing asthma management challenges in a multisite, urban Head Start program. Public Health Nurs, 274, 326–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gern JE, Rosenthal LA, Sorkness RL, Lemanske RF Jr. (2005). Effects of viral respiratory infections on lung development and childhood asthma. J Allergy Clinical immunology, 1154, 668–674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gleason M, Cicutto L, Hass-Howard C, Raleigh BM, Szefler. (2016). Leveraging Partnerships: Families, Schools, and Providers Working Together to Improve Asthma Management. Curr Allergy Asthma Rep, 16, 74. [DOI] [PubMed] [Google Scholar]
- 13.Head Start Early Childhood Learning and Knowledge Center (2018). Internet source cited 2019 Feb 14, Available from: https://eclkc.ohs.acf.hhs.gov/publication/head-start-parent-family-community-engagement-framework
- 14.Kakumanu S, Antos N, Szefler SJ, Lemanske RF Jr. (2017). Building school health partnerships to improve pediatric asthma care: the School-based Asthma Management Program. Curr Opin Allergy Clin Immunol. 172, 160–166. [DOI] [PubMed] [Google Scholar]
- 15.Kirk MA, Kelley C, Yankey N, Birken SA, Abadie B, Damschroder L. (2016). A systematic review of the use of the Consolidated Framework for Implementation Research. Implementation Science, 111, 72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moonie SA, Sterling DA, Figgs L, Castro M. (2006). Asthma Status and Severity Affects Missed School Days. J School Health, 761, 18–24. [DOI] [PubMed] [Google Scholar]
- 17.Mowrer JL, Tapp H, Ludden T, Kuhn L, Taylor Y, et al. (2015). Patients’ and providers’ perceptions of asthma and asthma care: a qualitative study. J Asthma, 529, 949–956. [DOI] [PubMed] [Google Scholar]
- 18.Neuharth-Pritchett S, Getch YQ. (2001). Asthma and the School Teacher: The Status of Teacher Preparedness and Training. J of School Nursing, 176, 323–328. [DOI] [PubMed] [Google Scholar]
- 19.NVivo qualitative data analysis Software; QSR International Pty Ltd; Version 10, 2012. [Google Scholar]
- 20.Ritchie J, Spencer L. (1994). Qualitative data analysis for applied policy research In Bryman A & Burgess R (Eds.), Analyzing qualitative data (pp. 173–194). London: Routledge. [Google Scholar]
- 21.Tong A, Sainsbury P, Craig J. (2007). Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care, 196, 349–357. [DOI] [PubMed] [Google Scholar]
- 22.Walsh KM, Kelly CS, Morrow AL. (1999). Head Start: A setting for asthma outreach and prevention. Family Community Health, 221, 28–37. [Google Scholar]; Wier LM, Yu H, Owens PL, Washington R. (2013). Statistical Brief #157:Overview of children in the Emergency Department, 2010. Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
- 23.Wier LM, Yu H, Owens PL, Washington R. (2013). Statistical Brief #157:Overview of children in the Emergency Department. Agency for Healthcare Research and Quality. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.