Abstract
Background and Aims:
In the United States, availability of prescription opioids has decreased in recent years. Whether there have been corresponding changes in the likelihood of persons with prescription opioid use disorder (POUD) to engage in illegal behaviors related to drug use remains unknown. We examined changes in prevalence of illegal behaviors between persons with and without POUD over time, and how transactions for obtaining opioids have changed among persons with POUD over time.
Design:
Temporal trend analysis of repeated cross-sectional data.
Setting:
United States household dwelling population from all 50 states and District of Columbia.
Participants:
Adult subsamples from the 2002–2014 National Survey of Drug Use and Health (n=5,393 persons with POUD; n=486,768 persons without POUD).
Measurements:
Outcome variables were selected illegal behaviors and sources of opioids used non-medically. POUD was defined using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, criteria. Time was treated as a continuous variable. The variable of interest for each illegal behavior analysis was the interaction between POUD diagnosis and time. Covariates included age, sex, and race/ethnicity.
Findings:
Over the 13-year period examined, the adjusted interaction odds ratio (AIOR) describing the change in association between POUD and selling illicit drugs increased by a factor of 2.41 (95% CI: 1.56–3.71, p<.001). Similar trends were noted for stealing (AIOR 2.12, 95% CI: 1.31–3.44, p=.002) and for lifetime history of arrest (AIOR 1.53, 95% CI: 1.06–2.19, p=.021). Persons with POUD became less likely to receive opioids for free from friends and family (AOR 0.42, 95% CI: 0.25–0.71, p=.001) and more likely to buy them from friends and family (AOR 3.29, 95% CI: 1.76–6.13, p<.001) from 2005–2014.
Conclusions:
In the United States, against a backdrop of a decreasing prescription opioid supply, rates of some crimes potentially related to drug use increased among persons with prescription opioid use disorder (POUD) compared with those without POUD from 2002–2014.
Keywords: opioid use disorder, prescription opioid use disorder, illegal behavior, crime, non-medical opioid source
Introduction
It is generally accepted that the United States’ relative oversupply of prescription opioids during the past 20 years has played a significant causal role in the current U.S. opioid epidemic (1, 2). The number of opioid prescriptions in the United States quadrupled from 1999 to 2008, paralleling the rise in opioid-related deaths during this period (3). As awareness of the potential danger of prescription opioids grew, multiple interventions were implemented to combat opioid overprescribing and misuse. For example, prior to 2002, 17 states had prescription drug monitoring programs (PMDPs); since 2002, an additional 32 states implemented PMDPs (4). In addition, an increasing number of states issued opioid prescribing guidelines (e.g., (5)) and placed restrictions on pain management clinics (6). Finally, an abuse-deterrent formulation of Oxycontin was introduced in 2010 (7).
National data trends indicate these interventions have had their intended consequences. After documented increases in the number of U.S. opioid prescriptions from 1999–2010 (3, 8), the number of prescriptions stabilized beginning in 2010 and from 2012–2017 steadily declined (8–12). In addition, the average per capita opioid dose increased from 2006–2010, then declined from 2010–2015 (12). Finally, the prevalence of persons who use prescription opioids for non-medical reasons has decreased in recent years (13, 14).
A changing prescription opioid market, however, carries potential for unintended consequences as well, especially for those with prescription opioid use disorder (POUD). Indeed, a temporal association between a decreased supply of prescription opioids and increased prevalence of heroin use among persons with POUD has been reported (14, 15), and persons with POUD have noted that heroin became cheaper and more available than prescription opioids following the introduction of the abuse-deterrent formulation of Oxycontin (15, 16).
Another potential unintended consequence of a tightening prescription opioid market is an increase in rates of other illegal behaviors and justice system involvement in persons with POUD. Specifically, one could hypothesize that as the prescription opioid supply has become more restricted, persons with POUD have become more likely to engage in acquisitive crime and illegal transactions to maintain their addiction. While previous studies have demonstrated associations between illegal behaviors and justice system involvement in persons with an opioid use disorder (OUD) (17–19), these studies have included persons with heroin use disorder (HUD). As heroin use itself is illegal, conclusions that can be drawn about the relationship between POUD and the justice system are limited. Interestingly, one recent cross-sectional study found that more than 50% of persons with POUD without co-morbid heroin use reported a lifetime history of justice system involvement and 20% reported being arrested within the past year (20). Whether this overlap has been affected by the decreasing supply of prescription opioids, however, is not known and has public health and policy implications as prisons contemplate their approach to treating inmates with OUD and policy makers consider increasing the severity of legal punishment for persons who commit drug-related crimes (21–24).
Another possible consequence of a changing opioid market is that the sources from where persons with POUD obtain opioids used for non-medical reasons may have changed. Earlier cross-sectional studies have shown that the majority of persons who misuse prescription opioids obtain them for free from friends or family or receive them from a physician prescription (25–27). While persons with POUD are also most likely to obtain opioids from these two sources (27), they are also disproportionately likely to obtain prescription opioids via illicit means compared to non-medical users without POUD (13). Whether the relative importance of sources of opioids for non-medical reasons has changed over time for persons with POUD has not been previously reported.
Using nationally representative data, we aimed to 1) assess changes in the strength of associations between POUD and illegal behaviors over time, and 2) examine changes in prevalence of sources of prescription opioids used for non-medical reasons among persons with POUD over time.
Methods
Data Source
Data were obtained from the 2002–2014 National Survey on Drug Use and Health (NSDUH). NSDUH is directed by the Substance Abuse and Mental Health Services Administration and contracted through RTI, International. The survey is conducted annually and measures substance use patterns in the U.S. civilian, noninstitutionalized, domiciled population aged 12 and older. NSDUH utilizes a 50-state design with an independent multistage area probability sample for each state and the District of Columbia. Informed consent is obtained prior to participation. RTI fieldworkers interview participants; questions about potentially sensitive behaviors, including drug use and illegal activities, are administered via audio-computer-assisted self-interview to maximize confidentiality. Detailed information about survey methodology is available elsewhere (28). Data collection procedures were approved by the Institutional Review Board at RTI. Public use NSDUH files for the time period of interest were obtained from the Interuniversity Consortium for Social and Political Research (29).
We selected 2002 as the start of the observation period as prior surveys had significant methodological differences. We selected 2014 as the end of the observation period as opioid use questions were redesigned in the 2015 NSUDH precluding comparisons after 2014. The selection from 2002–2014 thus allowed us to capture the broadest time period possible that would include the years during which the prescription opioid supply was changing for which comparable year-to-year data were available. Participants aged 18 and older were included in analyses. Survey response rates from 2002 to 2014 ranged from 58.3% to 71.3%.
Variables
Past-year Prescription Opioid Use Disorder
POUD was defined by NSDUH using Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for prescription opioid abuse or dependence. Of the 5,393 persons with POUD, 494 persons (9.30%, 95% CI 8.03–10.57) also met criteria for HUD. Because comorbid HUD can be viewed as a marker of disease severity in POUD (30–32), these persons were included in the main analyses, although heroin use was adjusted for in supplementary analyses.
Persons without POUD comprised the comparison general population “No POUD” group. Of the 487,438 persons without POUD, 670 (0.08%, 95% CI 0.08–0.10) met criteria for HUD. As the goal of analyses was to compare persons with POUD to a general population without any OUD, these 670 persons were excluded from main analyses, but were included in descriptive analyses measuring POUD prevalence over time.
Time and Time-by-Prescription Opioid Use Disorder Interactions
Time was examined as a continuous variable. Changes in the strength of association between POUD and each dependent variable was measured by the interactions between time and POUD status.
Illegal Behavior and Arrest Outcome Variables
Past-year history of the following were examined as dichotomous (yes/no) variables: selling illicit drugs, stealing or trying to steal item(s) worth more than $50, and attacking someone with the intent to cause harm. Lifetime history of arrest and past-year history of arrest were examined as dichotomous variables.
Past-year heroin use was examined as a dichotomous variable. A dichotomous variable for past-year non-heroin illicit drug use was created as a composite of the following NSDUH variables: past-year use of hallucinogens, inhalants, or cocaine; or past-year non-medical use of sedatives, tranquilizers or stimulants. Given the relatively high prevalence of recreational cannabis use as well as recent changes in cannabis legalization in multiple states, cannabis use was not included in the variable.
Other past-year substance use disorder variables
To examine whether any changes associations between illegal behaviors and POUD were specific to opioids or not, post-hoc analyses examined changes in associations between illegal behaviors and two other substance use disorders: alcohol use disorder and cocaine use disorder. Past-year alcohol use disorder and past-year cocaine use disorder were defined using DSM-IV criteria for alcohol abuse or dependence and cocaine abuse or dependence, respectively.
Source of Non-Medical Prescription Opioids Outcome Variables
All NSDUH participants who reported past-year prescription opioid use for non-medical reasons were asked about their most recent source of prescription opioids used for non-medical reasons. Responses to this question included: one doctor, more than one doctor, writing a fake prescription, stealing a prescription opioid from a physician’s office or clinic or hospital or pharmacy, obtaining from friends and family for free, buying from friend or family, taking from friend or family without asking, buying from a drug dealer or other stranger, obtaining from the internet, and some other way. Responses were recoded into six categories: prescription from one or more physician(s), stolen (from physician’s office or friends/family), obtained for free from friends or family, bought from friends or family, bought from a drug dealer or stranger, or other (combined writing fake prescription, internet, other). Questions about prescription opioid sources were not asked prior to 2005, thus the time period for these analyses was from 2005 to 2014.
Covariates
Covariates included sex, age, and race/ethnicity. Age was treated as a categorical variable with the following four groups: 18–25, 26–34, 35–49, and 50 years or older. Categories for race/ethnicity were defined by NSDUH as follows: White; Black; Hispanic; Native American or Alaskan Native; Asian (combined categories of Asian and Native Hawaiian/Other Pacific Islander); and multiracial.
Statistical Analyses
Analyses were conducted using SAS version 9.4 and STATA version 14 survey procedures so that weights and survey design variables were utilized to account for the NSDUH’s complex sample design.
Descriptive Analyses
Descriptive statistics were used to measure prevalence of POUD over time; bivariate logistic regression to examine changes in POUD prevalence over time.
Descriptive statistics were used to measure prevalence of demographics and each of the selected illegal behaviors over time within each group (POUD and No POUD). Descriptive statistics were also used to measure prevalence of sources of prescription opioids within the POUD group. To simplify data presentation, demographic and illegal behavior prevalence data were averaged into three multi-year time periods: 2002–2005, 2006–2009, and 2010–2014. Source prevalence data were averaged into two multi-year time periods: 2005–2009 and 2010–2014.
Rao-Scott chi square tests were used to test for differences in demographic variables between POUD and No POUD groups within each of the three multi-year time periods. To assess the between-group difference in odds for each illegal behavior within each of the three multi-year periods, we modeled each illegal behavior as a function of POUD status while adjusting for covariates. The resultant between-group AORs reflected the change in odds for each illegal behavior attributable to POUD within a particular time period.
To measure the changes in prevalence of each illegal behavior over time within each group, we modeled each illegal behavior as a function of time (treated as a continuous variable) while adjusting for covariates, with resultant within-group adjusted odds ratios (AORs) reflecting the overall change in odds during the 13-year time period for each group.
Primary Analyses
For all primary analyses, time was treated as a continuous variable. To assess changes in the strength of associations between POUD and illegal behaviors over time while controlling for general population trends, each of the seven illegal behaviors was modeled using multivariable logistic regression. Unadjusted analyses modeled each illegal behavior as a function of POUD status, time, and an interaction term POUD status*time. Adjusted analyses controlled for covariates. The trend difference between POUD and No POUD groups for each illegal behavior was captured by the interaction term POUD status*time, which measured the adjusted interaction OR (AIOR). Thus, the AIOR represented the total proportional change over the 13-year time period in the odds ratio describing the association between POUD and the illegal behavior.
Recognizing illicit substance use as a risk factor for justice system involvement (19), past-year non-heroin illicit drug use was included as an additional covariate in supplementary analyses. To account for the possibility of heroin use contributing to the relationship between POUD and illegal behaviors, supplementary analyses also included models that adjusted for both past-year heroin use and past-year non-heroin illicit drug use.
Finally, multivariable regression was used to examine changes in sources of prescription opioids used for non-medical reasons over time within the POUD group, modeling source as a function of time while adjusting for covariates. Models were adjusted for past-year non-heroin illicit drug use and past-year heroin use in supplementary analyses.
Post-hoc Analyses
To examine if the observed changes in the associations between POUD and illegal behaviors over time were specific to POUD or indicative of a broader association between presence of any substance use disorder and illegal behaviors, in post-hoc analyses we examined associations between two other selected substance use disorders and illegal behaviors over time. Multivariable logistic regression was used to measure the strength of the associations between alcohol use disorder and illegal behaviors over time, and between cocaine use disorder and illegal behaviors over time. Unadjusted and adjusted models were identical to those examining the strength of associations between POUD and illegal behaviors over time, excepting substance use disorder. To determine if co-morbid POUD was contributing to results, models were also adjusted for POUD status.
Results
Demographics
The demographic composition of the POUD and the No POUD groups are described in Table 1. Averaged prevalence data are presented in three time groups: 2002–2005, 2006–2009, and 2010–2014. Compared to the No POUD group, the POUD group was more likely to be male, younger, and to identify as either white or Native American or Alaskan Native, and less likely to identify as Black or Asian at every time point (see Table 1).
Table 1.
Demographics of Study Population.
| POUD (Prevalence, 95% CI) | No POUD (Prevalence, 95% CI) | |||||
|---|---|---|---|---|---|---|
| 2002–2005 n=1384 |
2006–2009 n=1779 |
2010–2014 n=2230 |
2002–2005 n=146,381 |
2006–2009 n=147,934 |
2010–2014 n=192,453 |
|
| Sex | ||||||
| Male | 54.5 (50.0, 59.0) | 57.7 (54.0, 61.3) | 60.1 (56.4, 63.8) | 48.0 (47.6, 48.5) | 48.2 (47.8, 48.6) | 48.1 (47.7, 48.5) |
| Female | 45.5 (41.0, 50.0) | 42.3 (38.7, 46.0) | 39.9 (36.2, 43.7) | 52.0 (51.5, 52.4) | 51.8 (51.4, 52.2) | 51.9 (51.5, 52.3) |
| Age | ||||||
| 18–25 | 37.2 (34.0, 40.4) | 38.0 (34.5, 41.4) | 31.8 (29.1, 34.5) | 14.8 (14.5, 15.0) | 14.6 (14.3, 14.9) | 14.6 (14.3, 14.8) |
| 26–34 | 22.1 (18.5, 25.8) | 24.7 (21.4, 28.0) | 29.8 (26.6, 33.1) | 16.3 (16.0, 16.6) | 15.8 (15.5, 16.1) | 15.6 (15.4, 15.9) |
| 35–49 | 29.7 (25.4, 33.9) | 27.0 (22.8, 31.2) | 21.6 (18.3, 24.9) | 30.4 (30.0, 30.9) | 28.9 (28.5, 29.3) | 26.1 (25.8, 26.4) |
| 50+ | 11.0 (6.6, 15.5) | 10.4 (6.8, 13.9) | 16.8 (13.1, 20.5) | 38.5 (38.0 39.1) | 40.7 (40.1, 41.4) | 43.7 (43.2, 44.3) |
| Race/ethnicity | ||||||
| White | 74.7 (71.0, 78.4) | 75.4 (71.9, 78.8) | 72.8 (69.4, 76.1) | 70.6 (70.1, 71.1) | 68.9 (68.3, 69.5) | 66.4 (65.9, 66.9) |
| Black | 8.1 (5.6, 10.6) | 8.3 (5.5, 11.0) | 9.5 (7.1, 11.8) | 11.2 (10.8, 11.6) | 11.5 (11.1, 11.9) | 11.6 (11.3, 12.0) |
| Hispanic | 11.4 (8.9, 13.8) | 12.6 (10.1, 15.1) | 12.4 (9.7, 15.2) | 12.3 (11.9, 12.7) | 13.4 (13.0, 13.8) | 14.8 (14.4, 15.1) |
| Asian | 3.0 (1.2, 4.8) | 1.9 (0.8, 2.9) | 2.4 (1.3, 3.5) | 4.4 (4.1, 4.6) | 4.7 (4.4, 5.0) | 5.3 (5.1, 5.6) |
| Native American/Alaskan Native | 1.5 (0.4, 2.7) | 0.6 (0.3, 0.9) | 1.3 (0.4, 2.1) | 0.5 (0.5, 0.6) | 0.5 (0.4, 0.6) | 0.5 (0.5, 0.6) |
| Multiracial | 1.3 (0.4, 2.1) | 1.2 (0.6, 1.9) | 1.7 (1.0, 2.3) | 1.0 (0.9, 1.1) | 1.1 (1.0, 1.1) | 1.4 (1.3, 1.4) |
Abbreviations: POUD, prescription opioid use disorder; CI, confidence interval.
Note: Rao-Scott chi square tests used for comparisons. All between-group comparisons were significant at the p<.01 level.
Prevalence of Prescription Opioid Use Disorders over Time
Prevalence estimates for POUD over time are shown in Figure 1. POUD prevalence in the general population increased from 0.63% in 2002 to 0.71% in 2014, which resulted in an overall odds increase of 44% over the 13 year period (OR= 1.44, 95% CI 1.24–1.68, p<.001). To examine the changes in co-morbid HUD and POUD over time, we subdivided POUD into two groups: POUD without co-morbid HUD and POUD with co-morbid HUD. Though not as common as POUD without co-morbid HUD, the prevalence of POUD with co-morbid HUD increased significantly from 2002 to 2014 (OR=5.29, 95% CI 3.13–8.94, p<.001).
Figure 1.
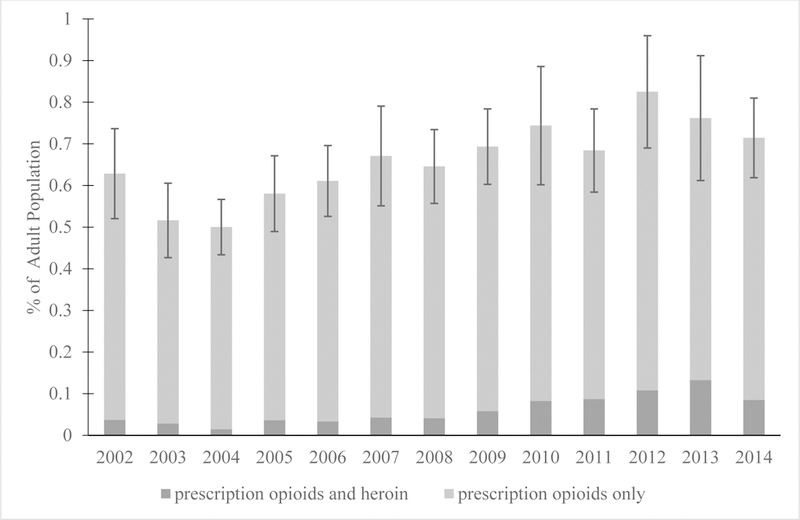
Prevalence of prescription opioid use disorder in the U.S. domiciled, non-institutionalized, non-incarcerated population aged 18 or older over time. For example, in 2014, 0.71% of adult population had prescription opioid use disorder; 0.63% of population had prescription opioid use disorder without co-morbid heroin use disorder while 0.08% had prescription opioid use disorder and heroin use disorder. Error bars represent 95% confidence intervals for total prescription opioid use disorder prevalence.
Illegal Behaviors
Prevalence of illegal behaviors in the POUD and No POUD groups during time period of interest are presented in Table 2. Averaged prevalence estimates are shown for 2002–2005, 2006–2009, and 2010–2014. The AORs for association between time and each illegal behavior within each group are shown in Table 2.
Table 2.
Changes in prevalence of illegal behaviors over time in persons with and without POUD, 2002–2014.
| POUD (Prevalence, 95% CI) | No POUD (Prevalence, 95% CI) | |||||||
|---|---|---|---|---|---|---|---|---|
| 2002–2005 n=1,384 |
2006–2009 n=1,779 |
2010–2014 n=2,230 |
AOR (95% CI) | 2002–2005 n=146,381 |
2006–2009 n=147,934 |
2010–2014 n=192,453 |
AOR (95% CI) | |
| Illegal Behavior | ||||||||
| Sold illicit drugs | 19.6 (15.6, 23.6) | 22.6 (19.6, 25.6) | 27.4 (24.4, 30.4) | 1.9 (1.2, 2.9)** | 1.6 (1.5, 1.6) | 1.6 (1.5, 1.7) | 1.4 (1.3, 1.4) | 0.8 (0.8, 0.9)*** |
| Stole >$50 | 10.6 (8.1, 13.0) | 13.2 (10.9, 15.6) | 14.9 (12.3, 17.5) | 1.8 (1.1, 2.8)* | 0.84 (0.79, 0.90) | 1.0 (0.90, 1.0) | 0.80 (0.74, 0.86) | 0.9 (0.8, 1.0) |
| Attacked with intent to harm | 12.9 (10.7, 15.1) | 12.9 (10.8, 14.9) | 10.7 (8.8, 12.5) | 0.7 (0.5, 1.0) | 1.4 (1.4, 1.5) | 1.4 (1.3, 1.5) | 1.1 (1.1, 1.2) | 0.7 (0.7, 0.8)*** |
| Arrest (ever) | 48.3 (43.8, 52.8) | 48.8 (44.5, 53.1) | 58.0 (54.7, 61.3) | 1.7 (1.2, 2.4)** | 16.8 (16.5, 17.1) | 17.2 (16.9, 17.6) | 17.8 (17.5, 18.1) | 1.2 (1.1, 1.2)*** |
| Arrest | 19.9 (16.3, 23.5) | 19.3 (16.2, 22.3) | 21.2 (18.3, 24.2) | 1.1 (0.69, 1.50) | 2.5 (2.4, 2.7) | 2.6 (2.5, 2.7) | 2.3 (2.2, 2.4) | 0.9 (0.8, 1.0)** |
| Heroin use | 6.4 (3.3, 8.4) | 8.8 (6.7, 11.0) | 16.1 (13.6, 18.5) | 1.5 (2.8, 7.8)*** | 0.06 (0.04, 0.07) | 0.08 (0.05, 0.10) | 0.08 (0.07, 0.10) | 1.8 (1.1, 2.8)* |
| Non-heroin illicit drug use | 59.1 (54.0, 64.2) | 65.3 (61.4, 69.2) | 64.9 (61.2, 68.5) | 1.5 (1.0, 2.1)* | 5.1 (4.9, 5.3) | 4.9 (4.8, 5.1) | 4.7 (4.5, 4.8) | 1.0 (0.9, 1.0) |
Note: Variables reflect past-year history unless otherwise noted. Numbers rounded to two decimal places for prevalence less than 1%.
Abbreviations: POUD, prescription opioid use disorder; CI, confidence interval; AOR, adjusted odds ratio. AORs represent the change in odds of engaging in each illegal behavior over the total 13 year time period within each group (POUD vs No POUD) after adjusting for sex, age, and race/ethnicity.
p<.05,
p<.01,
p<.001.
Overall, each illegal behavior variable measured was more prevalent in the POUD group than in the comparison group at each time point measured, and AORs were larger for the 2010–2014 time period than for the 2002–2005 period for each illegal behavior (Table 3). For example, within the 2002–2005 time period, persons with POUD had 9.6 greater odds of selling illicit drugs compared to the No POUD group; within the 2010–2014 time period, the difference in odds increased to 18.6 (Table 3).
Table 3.
The association of POUD and prevalence of engaging in illegal behaviors by time.
| 2002–2005 AOR (95% CI) |
2006–2009 AOR (95% CI) |
2010–2014 AOR (95% CI) |
|
|---|---|---|---|
| Illegal Behavior | |||
| Sold illicit drugs | 9.6 (7.2, 12.9)*** | 11.7 (9.7, 14.0)*** | 18.6 (15.4, 22.5)*** |
| Stole >$50 | 9.2 (6.9, 12.2)*** | 10.7 (8.5, 13.5)*** | 16.3 (13.1, 20.2)*** |
| Attacked with intent to harm | 6.2 (5.0, 7.8)*** | 6.4 (5.2, 7.8)*** | 7.2 (5.8, 9.0)*** |
| Arrest (ever) | 4.2 (3.4, 5.3)*** | 4.1 (3.4, 4.8)*** | 5.9 (5.0, 6.9)*** |
| Arrest | 6.7 (5.1, 8.8)*** | 5.9 (4.8, 7.2)*** | 7.8 (6.3, 9.6)*** |
| Heroin use | 79.6 (46.7, 135.7)*** | 85.3 (57.2, 127.2)*** | 145.8 (106.2, 200.0)*** |
| Non-heroin illicit drug use | 19.9 (15.2, 26.0)*** | 26.0 (20.9, 32.3)*** | 29.4 (24.2, 35.7)*** |
Note: Variables reflect past-year history unless otherwise noted.
Abbreviations: POUD, prescription opioid use disorder; AOR, adjusted odds ratio; CI, confidence interval. Each AOR represents the increased odds for each multi-year time period after adjusting for sex, age, and race/ethnicity.
p<.05,
p<.01,
p<.001.
The unadjusted IORs and AIORs estimating net changes in associations between POUD and each illegal behavior from 2002–2014 are shown in Table 4. For full results of each model, see Supplementary Table 1. Persons with POUD had an increased change in odds of selling illicit drugs, stealing, having a lifetime history of arrest, engaging in non-heroin illicit drug use, and engaging in heroin use relative to the general population. As an illustrative example of the interaction effect, the modeled trend difference for selling illicit drugs is shown in Figure 2. There was no significant trend difference between groups for attacking another person with intent to harm or for past-year arrest.
Table 4.
Changes in strength of associations between POUD and illegal behaviors from 2002–2014.
| Illegal Behavior | Unadjusted IOR (95% CI) | AIOR (95% CI) |
|---|---|---|
| Sold illicit drugs | 2.09 (1.44, 3.05)*** | 2.41 (1.56, 3.71)*** |
| Stole > $50 | 1.83 (1.18, 2.84)** | 2.12 (1.31, 3.44)** |
| Attacked with intent to harm | 0.99 (0.68, 1.43) | 1.03 (0.70, 1.51) |
| Arrest (ever) | 1.61 (1.17, 2.21)** | 1.53 (1.06, 2.19)* |
| Arrest | 1.24 (0.85, 1.80) | 1.23 (0.80, 1.89) |
| Heroin use | 2.48 (1.30, 4.75)** | 2.61 (1.32, 5.15)** |
| Non-heroin illicit drug use | 1.49 (1.06, 2.10)* | 1.66 (1.10, 2.52)* |
Note: Variables reflect past-year history unless otherwise noted.
Abbreviations: POUD, prescription opioid use disorder; CI, Confidence interval; IOR, interaction odds ratio; AIOR, adjusted interaction odds ratio. Each interaction odds ratio reflects the total 13-year change in the odds for each illegal behavior by POUD status, as measured by the interaction term POUD status*time.
AIORs were adjusted for sex, age and race/ethnicity.
p<.05,
p<.01,
p<.001.
Figure 2.
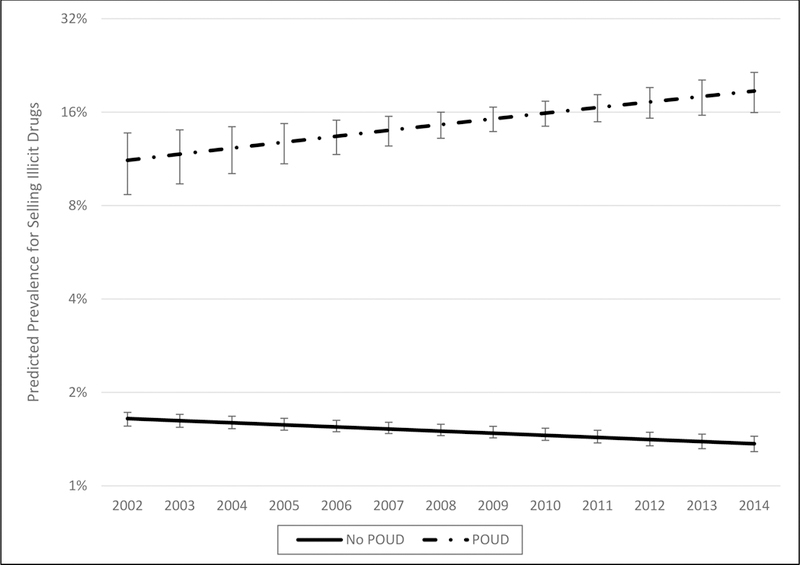
Modeled prevalence of past-year history of selling illicit drugs from 2002–2014 by prescription opioid use disorder status, predicted from logistic regression. Note that Y axis is plotted on log-based 2 scale. Error bars represent 95% confidence intervals for predicted prevalence. Abbreviations: POUD, prescription opioid use disorder.
Supplementary analyses that adjusted for past-year non-heroin illicit drug use did not change AIORs substantially, although the trend difference for lifetime history of arrest was no longer nominally significant (See Supplementary Table 2). When models were adjusted for both past-year heroin use and past-year non-heroin illicit drug use, the difference in the change in odds of selling illicit drugs remained significant (Supplementary Table 2).
Post-hoc analyses examining changes in associations between alcohol use disorder and illegal behaviors over time showed that persons with alcohol use disorder became significantly less likely to have a history of arrest compared to the general population from 2002–2014; there were no other significant trend differences (Supplementary Table 3). Analyses for cocaine use disorder resulted AIORs that were generally smaller than those for POUD, and after adjusting for POUD, did not meet the threshold for statistical significance (Supplementary Table 3).
Source of Prescription Opioids
Prevalence data for sources of non-medical opioids within the POUD group are displayed in Table 5. Data are shown in two aggregated time intervals of 2005–2009 and 2010–2014; AORs measuring changes in source over time among persons with POUD are also shown in Table 5. Rank-order of sources of non-medical opioids remained stable over time. The most prevalent source was free from friends and family, followed by prescription from physician(s). The prevalence of obtaining prescription opioids from friends or family for free decreased significantly over time, and there was a significant increase in prevalence of buying opioids from friends or family. There were no significant changes in prevalence of obtaining prescription opioids from physician(s), stealing, or drug dealers over time. Results were largely unchanged after adjusting for past-year non-heroin illicit drug use and past-year heroin use (Supplementary Table 4).
Table 5.
Changes in prevalence of opioid source over time among persons with POUD, 2005–2014.
|
2005–2009 (n=1,479) |
2010–2014 (n=1,495) |
||
|---|---|---|---|
| Source | Prevalence (95% CI) | Prevalence (95% CI) | AOR (95% CI) |
| Free from friends/family | 40.45 (36.21, 44.69) | 30.71 (26.80, 34.61) | 0.42 (0.25, 0.71)** |
| Prescription from physician(s) | 19.36 (16.20, 22.52) | 25.68 (21.91, 29.44) | 1.56 (0.80, 3.04) |
| Bought from friends/family | 15.24 (12.39, 18.09) | 22.96 (19.75, 26.18) | 3.29 (1.76, 6.13)*** |
| Bought from drug dealer/stranger | 14.09 (10.64, 17.53) | 12.55 (10.58, 14.51) | 1.27 (0.55, 2.96) |
| Stolen | 6.86 (5.03, 8.69) | 5.53 (3.37, 7.69) | 0.40 (0.15, 1.05) |
| Other | 4.01 (2.42, 5.59) | 2.58 (1.55, 3.61) | 0.36 (0.12, 1.03) |
Note: Data on sources of non-medical opioids were not collected prior to 2005; reported AORs are for 10-year period for which data were available.
Abbreviation: POUD, prescription opioid use disorder; CI, confidence interval; AOR, adjusted odds ratio. Models adjusted for sex, age, and race/ethnicity.
p<.01,
p<.001.
Discussion
Based on estimates from a large, nationally representative sample, persons with POUD were more likely than persons without POUD to engage in illegal behaviors at each time point from 2002–2014. In addition, persons with POUD became increasingly likely to sell illicit drugs, steal, have lifetime history of arrest, and to use heroin and other illicit drugs compared to their non-POUD counterparts over this time period. Results were substantively unchanged after adjusting for past-year non-heroin illicit drug use, suggesting that the increase in prevalence of illegal behaviors was specific to opioids. Further supporting the specificity to opioids was the lack of increased associations between other substance use disorders and illegal behaviors during this time period. Most of the associations between POUD and illegal behaviors appeared to be driven by heroin use; however, POUD was associated with an increased prevalence of selling drugs over time even after adjusting for past-year heroin use, suggesting observed increases in this illegal behavior was specific to misuse of prescription opioids. Finally, persons with POUD became significantly less likely to obtain prescription opioids for free from friends and family and significantly more to buy them from friends and family over time.
To our knowledge, this study is the first to examine associations between POUD and illegal behaviors over time while controlling for trends in the general population. The greater prevalence of illegal behaviors among the POUD group compared to the general population at every time point indicates the association between POUD and engagement in illegal activities is longstanding. This is especially notable as prescription opioids are licit substances, commonly received from physicians, and thus may not be thought of intuitively as conferring an increased risk of engagement in illegal behaviors. Further, our findings suggest that opioid supply-side interventions may have had the unintended consequence of increased prevalence of illegal behaviors and justice system involvement among persons with POUD. While methodological changes in the NSDUH precluded trend analyses of associations between POUD and illegal behaviors for years after 2014, there have been continued supply-side interventions in more recent years, including a continued decrease in the number of opioid prescriptions (11), the release of the 2016 CDC Guideline for Prescribing Opioids for Chronic Pain (33) and the 2017 Veteran’s Administration and Department of Defense for Clinical Practice Guidelines opioid prescribing (34). Whether these additional interventions are associated with further increases in illegal behaviors in persons with POUD is an important area of future study.
Our findings have several policy and public health implications. Notably, our results indicate that the illegal behaviors in which persons with POUD have become increasingly likely to engage are consistent with the motivation to maintain their use disorder. Our finding that persons with POUD have become increasingly likely to sell illicit drugs, coupled with the finding that they have become more likely to buy opioids from friends and family, are relevant to recent policy debates regarding increased severity of legal punishment for illicit drug selling (24). Our results suggest that for persons with POUD, illicit sales are becoming increasingly likely to occur among friends and family, and that persons with POUD are increasingly likely to sell illicit drugs. The latter result raises the larger issue of whether some persons with POUD would be better served by effective addiction treatment instead of increased legal punishments. Indeed, the United States spent 7.7 billion dollars on justice system costs related to POUD in 2013; less than half of this amount was spent on POUD treatment (35).
Our findings that heroin and other illicit drug use has increased in recent years among persons with POUD are consistent with those of previous studies (14, 15), and provide further evidence that persons with prescription opioid addiction have moved towards more potent and potentially dangerous opioids and other illicit drugs to maintain their addiction. Our finding that heroin use significantly increased over time among persons in general population, specifically in persons without a prescription opioid or heroin use disorder may reflect another unintended consequence of a decreasing prescription opioid supply availability in the context of increased heroin supply.
Limitations
Although we present data from the longest time period possible, methodological changes in the NSDUH preclude examination beyond 2014, and thus how trends in illegal behaviors and sources of non-medical opioids have changed in more recent years is not known. As with any observational study, causal relationships cannot be inferred. However, our findings provide important information on changes in behaviors on a population level over time. Finally, as NSDUH excludes persons who are currently incarcerated, our prevalence data for justice system involvement are likely underestimates.
Conclusions
Our findings indicate a potential unintended consequence of the tightening prescription opioid market is an increased likelihood of persons with POUD to engage in illegal behaviors that are potentially related to their drug use. Public health officials and policy makers should consider these trends when deciding how best to allocate resources to combat the opioid epidemic.
Supplementary Material
Acknowledgments
This work was supported by grants from the National Institutes of Health: T32DA007261-17 (Dr. Mintz), R21 AA024888-01 (Dr. Hartz), R21 DA044744 (Drs Grucza and Hartz), UL1 TR002345 (Dr. Hartz), U10AA008401 (Dr. Bierut) R01DA036583 (Dr. Bierut) and R21AA02568901 (Dr. Borodovsky).
Footnotes
Declaration of Competing Interests: Dr. Bierut is listed as an inventor on Issued U.S. Patent 8,080,371, “Markers for Addiction” covering the use of certain SNPs in determining the diagnosis, prognosis, and treatment of addiction. Dr. Borodovsky is on the board of directors and the treasurer of the non-profit scientific research organization MySafeRx Inc. Dr. Borodovsky does not receive any compensation from MySafeRx Inc.
References
- 1.Modarai F , Mack K , Hicks P , Benoit S , Park S , Jones C et al. Relationship of opioid prescription sales and overdoses, North Carolina, Drug Alcohol Depend 2013: 132: 81–86. [DOI] [PubMed] [Google Scholar]
- 2.Kenan K , Mack K , Paulozzi L Trends in prescriptions for oxycodone and other commonly used opioids in the United States, 2000–2010, Open Med 2012: 6: e41–47. [PMC free article] [PubMed] [Google Scholar]
- 3.Paulozzi LJ , Jones CM , Mack KA , Rudd RA Vital Signs: Overdoses of Prescription Opioid Pain Relievers-United States, 1999–2008 (Reprinted from MMWR, vol 60, pg 1487–1492, 2011), Jama-J Am Med Assoc 2011: 306: 2444–2446. [Google Scholar]
- 4.History of Prescription Drug Monitoring Programs: March 2018. Prescription Drug Monitoring Program Training and Technical Assistance Center; 2018. [Google Scholar]
- 5.Franklin G , Sabel J , Jones CM , Mai J , Baumgartner C , Banta-Green CJ et al. A comprehensive approach to address the prescription opioid epidemic in Washington State: milestones and lessons learned, Am J Public Health 2015: 105: 463–469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention Office for State T., Local and Territorial Support. Menu of Pain Management Clinic Regulation. [Google Scholar]
- 7.Statement of Purdue Pharma L.P. Regarding FDA’s Approval of Reformulated OxyContin® (oxycodone HCl controlled-release) Tablets; 2010. [Google Scholar]
- 8.Dart RC , Surratt HL , Cicero TJ , Parrino MW , Severtson SG , Bucher-Bartelson B et al. Trends in opioid analgesic abuse and mortality in the United States, N Engl J Med 2015: 372: 241–248. [DOI] [PubMed] [Google Scholar]
- 9.Levy B , Paulozzi L , Mack KA , Jones CM Trends in Opioid Analgesic-Prescribing Rates by Specialty, U.S., 2007–2012, Am J Prev Med 2015: 49: 409–413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Delgado MK , Shofer FS , Patel MS , Halpern S , Edwards C , Meisel ZF et al. Association between Electronic Medical Record Implementation of Default Opioid Prescription Quantities and Prescribing Behavior in Two Emergency Departments, J Gen Intern Med 2018: 33: 409–411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Disease Control and Prevention. U.S. Opioid Prescribing Rate Maps; 2018. [Google Scholar]
- 12.Guy GP Jr. , Zhang K , Bohm MK , Losby J , Lewis B , Young R et al. Vital Signs: Changes in Opioid Prescribing in the United States, 2006–2015, MMWR Morb Mortal Wkly Rep 2017: 66: 697–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Han B , Compton WM , Jones CM , Cai R Nonmedical Prescription Opioid Use and Use Disorders Among Adults Aged 18 Through 64 Years in the United States, 2003–2013, JAMA 2015: 314: 1468–1478. [DOI] [PubMed] [Google Scholar]
- 14.Jones CM The paradox of decreasing nonmedical opioid analgesic use and increasing abuse or dependence - An assessment of demographic and substance use trends, United States, 2003–2014, Addict Behav 2017: 65: 229–235. [DOI] [PubMed] [Google Scholar]
- 15.Cicero TJ , Ellis MS Abuse-Deterrent Formulations and the Prescription Opioid Abuse Epidemic in the United States: Lessons Learned From OxyContin, JAMA Psychiatry 2015: 72: 424–430. [DOI] [PubMed] [Google Scholar]
- 16.Cicero TJ , Ellis MS , Surratt HL Effect of abuse-deterrent formulation of OxyContin, N Engl J Med 2012: 367: 187–189. [DOI] [PubMed] [Google Scholar]
- 17.Fisher WH , Clark R , Baxter J , Barton B , O’Connell E , Aweh G Co-occurring risk factors for arrest among persons with opioid abuse and dependence: implications for developing interventions to limit criminal justice involvement, J Subst Abuse Treat 2014: 47: 197–201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Harris EE , Jacapraro JS , Rastegar DA Criminal charges prior to and after initiation of office-based buprenorphine treatment, Subst Abuse Treat Prev Policy 2012: 7: 10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bronson J , Stroop J , Zimmer S Berzofsky M , Drug use, dependence, and abuse among state prisoners and jail inmates, 2007–2009 In: Bureau of Justice Statistics, editor, Washington, D.C.; 2017. [Google Scholar]
- 20.Winkelman TNA , Chang VW , Binswanger IA. Health, Plysubstance Use, and Criminal Justice Involvement Among Adults With Varying Levels of Opioid Use, JAMA Network Open 2018: 1: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Williams T Opioid Users are Filling Jails. Why Don’t Jails Treat Them? New York Times, New York, New York: The New York Times Company; 2017. [Google Scholar]
- 22.Nunn A , Zaller N , Dickman S , Trimbur C , Nijhawan A , Rich JD Methadone and buprenorphine prescribing and referral practices in US prison systems: results from a nationwide survey, Drug Alcohol Depend 2009: 105: 83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Green TC , Clarke J , Brinkley-Rubinstein L , Marshall BDL , Alexander-Scott N , Boss R et al. Postincarceration Fatal Overdoses After Implementing Medications for Addiction Treatment in a Statewide Correctional System, JAMA Psychiatry 2018: 75: 405–407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zezima K , Dawsey J Trump administration studies seeking the death penalty for drug dealers. The Washington Post, Washington, DC: Fred Ryan; 2018. [Google Scholar]
- 25.Jones CM , Paulozzi LJ , Mack KA Sources of Prescription Opioid Pain Relievers by Frequency of Past-Year Nonmedical Use: United States, 2008–2011, Jama Internal Medicine 2014: 174: 802–803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Schepis TS , McCabe SE , Teter CJ Sources of opioid medication for misuse in older adults: results from a nationally representative survey, Pain 2018: 159: 1543–1549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Han B , Compton WM , Blanco C , Crane E , Lee J , Jones CM Prescription Opioid Use, Misuse, and Use Disorders in U.S. Adults: 2015 National Survey on Drug Use and Health, Ann Intern Med 2017: 167: 293–301. [DOI] [PubMed] [Google Scholar]
- 28.National Survey on Drug Use and Health: Codebook; 2014. [Google Scholar]
- 29.Interuniversity Consortium for Social and Political Research. National Survey of Drug Use and Health (NSDUH) Series,; 2016. [Google Scholar]
- 30.Becker WC , Sullivan LE , Tetrault JM , Desai RA , Fiellin DA Non-medical use, abuse and dependence on prescription opioids among U.S. adults: Psychiatric, medical and substance use correlates, Drug and Alcohol Dependence 2008: 94: 38–47. [DOI] [PubMed] [Google Scholar]
- 31.Cicero TJ , Ellis MS , Surratt HL , Kurtz SP The Changing Face of Heroin Use in the United States A Retrospective Analysis of the Past 50 Years, Jama Psychiatry 2014: 71: 821–826. [DOI] [PubMed] [Google Scholar]
- 32.Lankenau SE , Teti M , Silva K , Bloom JJ , Harocopos A , Treese M Patterns of prescription drug misuse among young injection drug users, J Urban Health 2012: 89: 1004–1016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Dowell D , Haegerich TM , Chou R CDC Guideline for Prescribing Opioids for Chronic Pain--United States, 2016, JAMA 2016: 315: 1624–1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Clinical Practice Guideline for Opioid Therapy for Chronic Pain: Department of Veterans Affairs and Department of Defense; 2017, p. 1–198. [Google Scholar]
- 35.Florence CS , Zhou C , Luo F , Xu L The Economic Burden of Prescription Opioid Overdose, Abuse, and Dependence in the United States, 2013, Med Care 2016: 54: 901–906. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


