Abstract
This cohort study uses Medicare data to examine the incidence and prevalence of Alzheimer disease and all forms of dementia in individuals with Down syndrome.
The life span has profoundly increased for individuals with Down syndrome (DS), leading to a large, understudied population of middle-aged and older adults with DS.1 Clinical studies show individuals with DS are at higher risk and have earlier onset of dementia.2 Down syndrome is defined by trisomy of chromosome 21, the site of the amyloid precursor protein gene. Overexpression of amyloid precursor protein–produced β-amyloid is hypothesized to increase risk for Alzheimer disease (AD) dementia in individuals with DS.3 Autopsy and neuroimaging studies indicate that by age 40 years, virtually all adults with DS exhibit AD neuropathology.2 However, individuals can live decades with AD neuropathology prior to developing clinical symptoms.4 Research examining prevalence of dementia in individuals with DS has been largely confined to clinic-based convenience samples.3 Population-based epidemiological work is needed to clarify the extent of dementia in DS and illustrate the public health outcomes for the DS population, their families, and health service systems. We describe prevalence and incidence of dementia and AD in DS in a full Medicaid population of adults with DS in Wisconsin from 2008 through 2018.
Methods
We assessed Medicaid claims for adults (≥21 years) who ever had 2 DS claims over their lifetime (based on International Classification of Diseases, Ninth Revision and Tenth Revision codes) on 2 separate days during Medicaid enrollment. We analyzed claims from January 1, 2008, to December 31, 2018. This study was deemed exempt by the University of Wisconsin–Madison institutional review board, and informed consent was not necessary because of the deidentified nature of the data. Data were obtained under a limited data use agreement from the Wisconsin Department of Health Services. Further cohort details are as previously described.5
Dementia claims were extracted from codes for any dementia (with AD as a subset) from the Centers for Medicare & Medicaid Services Chronic Conditions Data Warehouse. We required 3 or more years of Medicaid enrollment for adults with DS to ensure validity of dementia claims6; therefore, beneficiaries entered the cohort at any point between 2008 and 2015. We categorized age at first and last claims (<40 years, 40-54 years, and ≥55 years) to account for confounding by age. We assessed prevalence by age category using log-binomial regression and used log-Poisson regression with a 1-year washout period to assess incident dementia claims and created Kaplan-Meier curves accounting for administrative censoring. We assessed whether dementia prevalence differed by sex using log-binomial regression. Statistical analysis was performed using SAS version 9.4 (SAS Institute). Statistical significance was assessed at an α = .05 level.
Results
The Table presents demographics, prevalence, and incidence of dementia and AD in individuals with DS. A total of 2968 individuals were included, of whom 1507 (50.8%) were male. The median (interquartile range) age at first claim was 39 (25-48) years.
Table. Demographic Statistics and Dementia Prevalence and Incidence Among 2968 Wisconsin Medicaid Enrollees With Down Syndrome and at Least 3 Years of Claims, 2008 Through 2018.
| Characteristic | Patients, No. (%) |
|---|---|
| Demographics | |
| Sex | |
| Male | 1507 (50.8) |
| Female | 1461 (49.2) |
| County typea | |
| Rural | 677 (22.8) |
| Urban | 2291 (77.2) |
| Age at first claim, y | |
| <40 | 1547 (52.1) |
| 40-54 | 1111 (37.4) |
| ≥55 | 310 (10.4) |
| Age at last claim, y | |
| <40 | 1017 (34.3) |
| 40-54 | 1013 (34.1) |
| ≥55 | 938 (31.6) |
| Administratively censored | 835 (28.1) |
| Prevalenceb | |
| Any dementia, No. per 1000 people (95% CI)c | |
| Total | 235 (220-251) |
| <40 | 40 (31-51) |
| 40-54 | 403 (375-433) |
| ≥55 | 610 (557-667) |
| Alzheimer disease, y | |
| Total | 149 (136-162) |
| <40 | 19 (13-27) |
| 40-54 | 273 (247-300) |
| ≥55 | 354 (305-412) |
| Incidence | |
| Any dementia, No. per 1000 person-years (95% CI)c | |
| Total | 27 (25-29) |
| <40 | 4 (3-5) |
| 40-54 | 49 (44-53) |
| ≥55 | 102 (87-119) |
| Alzheimer disease, y | |
| Total | 17 (15-19) |
| <40 | 2 (1-3) |
| 40-54 | 33 (30-37) |
| ≥55 | 56 (45-69) |
Rural and urban county designations were taken from Wisconsin Office of Rural Health.
The age category in this section was derived by the age at last claim.
Dementia and Alzheimer disease claims were determined using codes from Centers for Medicare & Medicaid Services Chronic Conditions Data Warehouse.
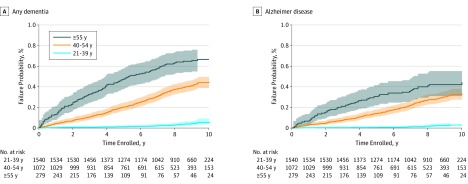
In the category of individuals aged 55 years or older, 490 of 938 had dementia claims (52.2%), 307 of 938 had AD claims (32.7%), and dementia incidence was 102 (95% CI, 87-119) cases per 1000 person-years. Among individuals aged 40 to 54 years, 190 of 1013 had dementia claims (18.8%), and dementia incidence was 49 (95% CI, 44-53) cases per 1000 person-years. The probability of an incident dementia claim was 40% (95% CI, 41%-47%) over 11 years of enrollment for adults with DS who were aged 40-54 years at cohort entry and 67% (95% CI, 60%-74%) for those 55 years and older at cohort entry (Figure). There were no sex differences for dementia among individuals younger than 40 years (prevalence ratio, 1.07 [95% CI, 0.63-1.81]) or among those 55 years and older (prevalence ratio, 0.94 [95% CI, 0.69-1.29]). Dementia prevalence was higher in female individuals than male individuals aged 40 to 54 years (prevalence ratio, 1.23 [95% CI, 1.02-1.50]).
Figure. Cumulative Incidence Functions for Incident Dementia Claim Among Medicaid Enrollees With Down Syndrome in Wisconsin, 2008 Through 2018.
Members enrolled in Medicaid for at least 3 years were included; a washout period of 1 year without a dementia claim was included.
Discussion
Our interpretation is limited by reliance on claims rather than direct observation and by the specificity of Wisconsin’s demographics, yet findings from a statewide health system confirm that both dementia and AD in individuals with DS present in claims data at rates similar to those ascertained from clinical samples.2,3 The hypothesized causative mechanism and similar eligibility requirements between state Medicaid programs for people with DS likely mean that other state Medicaid systems experience high incidence and prevalence of dementia and AD in individuals with DS. Dementia and AD prevalence and incidence in Medicaid beneficiaries with DS highlight the need to identify prodromal presentations and develop dementia services and supports for adults with DS as they age and continue to rely on Medicaid and Medicaid-funded assisted living or skilled nursing facilities.
References
- 1.Coppus AM. People with intellectual disability: what do we know about adulthood and life expectancy? Dev Disabil Res Rev. 2013;18(1):6-16. doi: 10.1002/ddrr.1123 [DOI] [PubMed] [Google Scholar]
- 2.Zigman WB, Lott IT. Alzheimer’s disease in Down syndrome: neurobiology and risk. Ment Retard Dev Disabil Res Rev. 2007;13(3):237-246. doi: 10.1002/mrdd.20163 [DOI] [PubMed] [Google Scholar]
- 3.Ballard C, Mobley W, Hardy J, Williams G, Corbett A. Dementia in Down’s syndrome. Lancet Neurol. 2016;15(6):622-636. doi: 10.1016/S1474-4422(16)00063-6 [DOI] [PubMed] [Google Scholar]
- 4.Sperling R, Mormino E, Johnson K. The evolution of preclinical Alzheimer’s disease: implications for prevention trials. Neuron. 2014;84(3):608-622. doi: 10.1016/j.neuron.2014.10.038 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rubenstein E, Bishop L. Is the autism boom headed for Medicaid? patterns in the enrollment of autistic adults in Wisconsin Medicaid, 2008-2018. Autism Res. 2019. doi: 10.1002/aur.2173 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Taylor DH Jr, Fillenbaum GG, Ezell ME. The accuracy of Medicare claims data in identifying Alzheimer’s disease. J Clin Epidemiol. 2002;55(9):929-937. doi: 10.1016/S0895-4356(02)00452-3 [DOI] [PubMed] [Google Scholar]