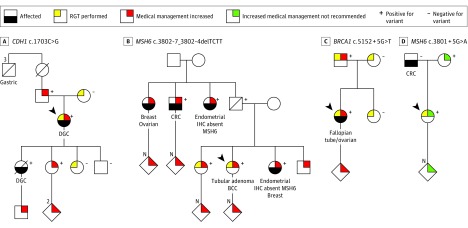
Figure 3. Pedigrees Demonstrating Clinical Management Changes From Selected Cases Undergoing RNA Genetic Testing.
A, The variant CDH1 c.1703C>G was identified by DNA genetic testing in an index patient meeting diagnostic criteria for hereditary diffuse gastric cancer (DGC; ie, 2 gastric cancer cases in the family, regardless of age, at least 1 confirmed DGC, and 1 case of DGC diagnosed at age <40 years). The variant was initially classified as a variant of uncertain significance, and subsequent to the reclassification to a likely pathogenic variant, the index patient was referred to the high-risk breast clinic for management of increased lobular breast cancer risk and consideration of risk-reducing bilateral mastectomy. The reclassification also impacted the clinical management of family members, as they became eligible for cascade genetic testing. B, Index patient was diagnosed with colorectal tubular adenoma and was found to carry the variant MSH6 c.3802-7_3802-4delTCTT on a 67-gene panel test. The patient’s sister, who had been previously diagnosed with endometrial adenocarcinoma showing loss of MSH6 (OMIM 600678) protein expression on immunohistochemistry (IHC), also carried this variant. Both sisters opted to participate in this study, and reclassification of the variant from a variant of uncertain significance to a likely pathogenic variant confirmed a diagnosis of Lynch syndrome. Both sisters elected risk-reducing total abdominal hysterectomy with bilateral salpingo-oophorectomy and were recommended to continue additional screening per National Comprehensive Cancer Network guidelines. Genetic testing for their adult children and other at-risk relatives was also recommended. C, A 24-gene panel identified the variant BRCA1 c.5152 + 5G>T in a woman diagnosed with papillary serous carcinoma of the right fallopian tube and both ovaries. The patient and her family opted to participate in this study, which resulted in the variant being reclassified from a variant of uncertain significance to a likely pathogenic variant. Subsequently, the patient was offered high-risk breast screening as defined by the National Comprehensive Cancer Network. The patient’s father was identified to carry the likely pathogenic variant and was recommended increased screening for prostate and breast cancers. D, A 34-gene panel identified the variant MSH6 c.3801 + 5G>A in an index patient with a family history of cancer. Colorectal cancer (CRC) screening recommendations for the patient included colonoscopy every 5 years based on family history. No abnormal transcripts were identified by RGT, resulting in reclassification from a variant of uncertain significance to a likely benign variant and no recommendation of increased medical management. No further familial testing was recommended for this variant. Diagonal lines indicate that the individual is deceased; arrows indicate index patients. BCC indicates basal cell carcinoma.