Abstract
Compared to men, women with alcohol use disorders experience more severe consequences related to drinking. Intensive Motivational Interviewing (IMI) is a new 9-session version of Motivational Interviewing (MI) designed for women with alcohol use disorders. The current study reports outcomes from a randomized clinical trial of IMI. Data were collected at baseline, 2-month, and 6-month follow-up. In addition to a standard “intent-to-treat” (ITT) analysis, we conducted disaggregated analyses of women who were heavy drinkers and a “per protocol” (PP) analysis of women in the IMI condition who attended 7–9 sessions (80% of the IMI sample). Women in both study conditions made large reductions in drinking between baseline and 2 months that were maintained at 6 months. Generalized estimating equation (GEE) models using the full sample (N=215) did not show time by condition differences, but heavy drinkers(n=153) receiving IMI showed significantly larger reductions in drinking at 2- and 6-month follow-up than the comparison condition. Assessment of heavy drinkers using the PP sample showed larger between condition differences favoring IMI at both follow-up time points. Results support the efficacy of IMI in terms of reducing drinking, particularly among women who are heavy drinkers.
Keywords: Women, Alcohol, Motivational Interviewing, Intensive Motivational Interviewing, heavy drinking
Research has documented that women suffer more severe consequences from problem drinking than men, including more severe health and social problems (Greenfield 2002). In addition, women advance more quickly from initial use, to onset of alcohol related problems, to first treatment episode (Greenfield et al. 2007). Despite more serious consequences related to drinking, treatment for women with alcohol use disorders has been understudied relative to that for men (Erol and Karpyak 2015). Findings from studies focused on women’s treatment are mixed. Some studies provide limited support for gender-specific programs (Greenfield et al. 2007; Walitzer and Dearing 2006), while others show better outcomes for programs that adapt services to be responsive to the needs of women, such as addressing psychiatric symptoms, trauma, parenting, and relationship issues (Greenfield et al. 2007). Like most programs for alcohol and drug problems, effect sizes are also typically small to medium and decline over time (Vasilaki, Hosier and Cox 2006). There is therefore an urgent need for gender specific interventions that have a larger, more sustained impact.
Intensive Motivational Interviewing
Intensive Motivational Interviewing (IMI) began as an intensive intervention for the treatment of methamphetamine (MA) dependence (Galloway, Polcin, Kielstein, Brown and Mendelson 2007). The rationale for developing a more intensive, 9-session dose of MI that went beyond the standard single MI session included the view that a higher number of sessions delivered over a longer period of time might be more effective for persons with more severe drug and other co-occurring problems (Polcin, Galloway, Palmer and Mains 2004). Nine sessions were chosen as being significantly more substantive than the standard single session of MI yet brief enough to keep a focus on MI interventions and avoid becoming more generic outpatient therapy.
IMI expands the process of change planning, a key MI ingredient, to address problems and strategies over time. In standard MI manuals, the change plan is typically developed during the final session. Thus, it is a static process with no opportunity to monitor how the change plan proceeds or adjust it when necessary. In contrast, in IMI, the change plan is continually evolving, with new goals being developed as stated goals are met.
Structure of the IMI Manual
IMI retains all the standard supportive and directive interventions of MI-based approaches (Polcin, Brown and Galloway 2005). The overall focus for the first three sessions is taken from the MI manual intervention developed by Obert and Farentinos (2000) for NIDA Clinical Trials Network (CTN) studies. The focus for first session is “problem identification.” The second session focuses on ambivalence, which includes the pros and cons of making a change in substance use. The primary goal is to meet the client where they are at in terms of their drinking and establish a therapeutic alliance. During subsequent sessions, the therapist guides the interaction to expand on reasons to make changes. This represents an effort to increase “change talk,” which has been found to be associated with improved outcomes (Miller and Rollnick, 2012). In the third session, the client and therapist collaborate on developing the change plan, which specifies changes the client wants to make and strategies for achieving them. Sessions four to eight focus on implementation of the change plan, which might include discussion of achievements, setbacks, revision of goals, revision of strategies for achieving goals and development of new goals. During these discussions the therapist guides the client into discussion of the pros and cons of the goals developed and strategies for achieving them. During session 9, the therapist and client focus on termination by reviewing what has transpired over the course of therapy, gains the client has been made, and ongoing plans for change.
After initial pilot testing of the manual (Galloway et al. 2007), a randomized clinical trial of 217 MA dependent persons was conducted. At 6 months, those who received IMI reduced psychiatric symptoms more than a comparison group consisting of a single session of MI that was enhanced with a nutrition education groups to achieve time equivalence between the two study conditions (Polcin et al. 2014). However, MA outcomes did not differ between the treatment and comparison group. An unexpected finding was that among women who had co-occurring alcohol problems (N= 87 ) those who received IMI (N=40) made more significant reductions in their drinking over the 6-month follow-up than women in the comparison condition. Men did not show similar improvements on drinking measures (Korcha, Polcin, Evans, Bond and Galloway 2014). The largest improvement in drinking outcomes for women were at the most distal follow-up time point, 6 months.
Modification of IMI for Women with Alcohol Disorders
Based on the favorable findings for alcohol reduction among women, funding was obtained to conduct a larger randomized study of IMI focused on alcohol problems and tailor the intervention to maximize the ways it responded to the needs of women. The main changes included directing therapists to assess whether a variety of issues identified by Erol and Karpyak (2015) and Greenfield et al (2007) impacted drinking: 1) relationships, 2) parenting, 3) sexual and physical abuse, 4) self-esteem, 5) obstacles to treatment entry, and 6) co-occurring mental health problems. Consistent with psychotherapy approaches for women in the general psychotherapy literature (DeYoung 2015), therapists elicited discussion about reciprocal associations between drinking and changes in drinking on social relationships. Reducing drinking and related issues, such as building self-efficacy and self-esteem, were primarily approached from an interpersonal perspective. For more details of the development, content, and implementation of the IMI intervention, see Polcin, Korcha and Nayak (2018). A copy of the manual can be obtained from the corresponding author.
Short-term (Two-Month) Outcomes for Women Receiving IMI
The first assessment of IMI for women with alcohol problems involved a randomized trial of 215 women who were interviewed at baseline and 2-month follow-up (Polcin, Korcha, Pugh, et al. 2018). Generalized estimating equation (GEE) models showed that relative to baseline, at 2-month follow-up women in both the IMI and comparison conditions made significant reductions in percent days drinking (PDD) (p<.001), percent heavy drinking days (PHDD) (p<.001), and alcohol severity (p<.001). However, among heavy drinking women, defined as those drinking 14 or more days to the point of intoxication over the past 30 days at baseline (n=153), those assigned to IMI (n=67) showed larger reductions in PDD (p<.01) and PHDD (p<.05) at 2-months than women in the comparison condition. Higher psychiatric severity at baseline and 2 months was associated with worse outcome for both groups.
Purpose
The purpose of the current study was to examine longer-term outcomes at 6-month follow-up. It was hypothesized that, similar to findings at 2 months, while both study conditions would improve on PDD, PHDD and alcohol severity outcomes, those receiving IMI would show greater reductions than the comparison condition at 6 months. As in the 2-month study, analyses assessed the impact of IMI for the full sample using an intent-to treat design and also the subgroup of women who were heavy drinkers at baseline.
An additional component in the examination of 6-month outcomes was the assessment of the effects of IMI among women who received a substantive dose of the intervention. To accomplish this goal, a per protocol analysis (PP) (Gupta 2011; Porta, Bonet and Cove 2007) was used that included women in the IMI condition who had attended 7 or more of the 9 sessions and hence received “intensive” MI. This level of attendance ensured exposure to all of the main elements of IMI, including implementation of the change plan over time. Over 80% of the women in the IMI condition attended 7–9 sessions, indicating an overall high level of acceptance of IMI and evidence that it could be feasibility delivered in an outpatient community-based setting.
Method
Sample
Data collection took place at an outpatient treatment program in Northern California. Women were primarily recruited through radio and newspaper advertising. Others contacted the clinic seeking services for alcohol problems. All participants were age 18 or older, able to speak English, capable of giving informed consent, and met DSM-V criteria for current alcohol use disorder. After an initial phone screen assessing these criteria, participants were screened in-person at the program where the study was conducted. Participants were assessed for detoxification symptoms and mental health disorders and were referred to outside services when it was clinically indicated, but they were not necessarily excluded from the study. However, women with serious, persistent medical or mental health problems were excluded and referred to more intensive services. Women with low to moderate severity of co-occurring drug problems (<6 DSM criteria) were included but those with high severity were excluded from study participation.
Procedures
Figure 1 indicates recruitment and retention data. Of the 384 women screened for the study, 69 were determined to be ineligible, 78 refused participation or did not show up for the baseline interview, and 22 were deemed ineligible at the baseline interview. After signing the informed consent and providing contact information for follow-up interviews, 215 participants completed the baseline assessment and were randomly assigned to receive IMI (n=108) or SMI (n=107) as developed by Martino et al (2006). Sessions occurred weekly for approximately 50 minutes. Randomization included a block design to ensure equivalence across the study conditions of low and medium/high severity of alcohol problems as determined by DSM-V criteria. Assignment to study condition was not blind. All participants were re-interviewed at 2- and 6-month follow-up. Participants were paid $30 for their time participating in the study at baseline and $50 at 2 and 6 months.
Figure 1.
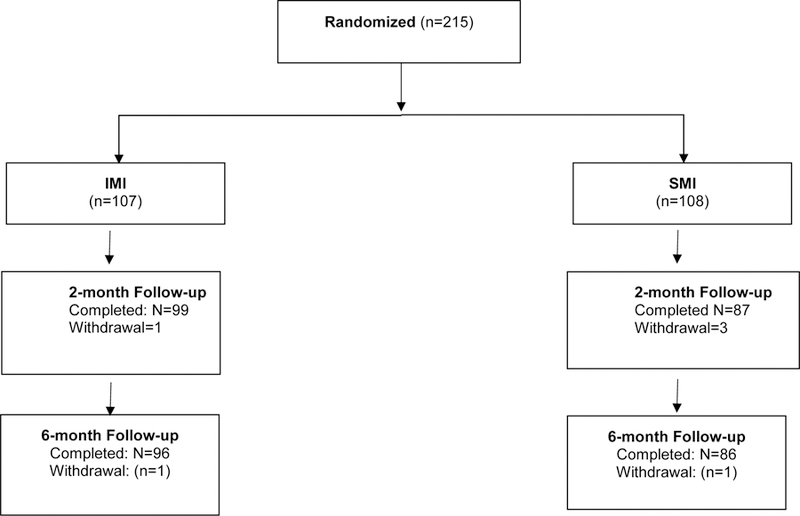
Randomization and follow-up
The IMI and the SMI comparison interventions were delivered by three female master’s degree therapists. Therapists provided sessions to women in both study conditions. Two of the three therapists had previous experience with IMI manuals. All received training on the specific aspects of IMI for women. To ensure competence and adherence to the IMI and SMI interventions, therapists audiotaped all sessions.
The Yale Adherence and Competence Scale II for Motivational Interviewing (YACS) (Nuro et al. 2005) was used as a measure of competency and fidelity for both treatments IMI and SMI. A sample of 146 tapes (16% of all sessions) for IMI and SMI were randomly assigned to raters to be assessed using the YACS. Both raters were Ph.D. psychologists and had previous experience coding MI sessions. One functioned as the primary rater during our 5-year study of IMI for MA dependence (Polcin et al, 2014). In addition to assessing standard items, trained raters examined compliance with modifications made to ensure that issues related to women were addressed. Theses were coded dichotomously as yes (issue was brought up by the client or therapist) or no (issue was not brought up by client or therapists. All session ratings were well above the minimum level for competence defined by the YACS for frequency and skillfulness of MI-based interventions. Inter-rater agreement on 9 tapes rated by two coders was 100% for meeting the minimum standard for competence. During the two months of active treatment, all women in both conditions also attended weekly outpatient group treatment using a Craving Intervention Management (CIM) (Galloway et al. 2000) model that was largely based on cognitive behavioral therapy principles. Study procedures were approved by the Institutional Review Board at the Public Health Institute.
Measures
Baseline Only
DSM V Checklist for Drug and Alcohol Disorders was used to determine inclusion criteria of current alcohol use disorder and exclusion of high severity of drug problems. Items were based on the previous version of the instrument, (American Psychiatric Association 2000; Forman, Svikis, Montoya and Blaine 2004) the DSM IV, but items were updated to reflect new criteria in the DSM V.
Demographics include ethnicity, age, education, and marital status.
Outcomes
Timeline Follow-Back (Sobell et al. 1996) (TLFB, drinking days and heavy drinking days) was used to record the participant’s self-report of percent drinking days (PDD) and percent heavy drinking days (PHDD) (4+drinks) during the past 60 days. The EtG metabolite urine testing was used at each time point to establish concordance with self-reported alcohol use.
Addiction Severity Index Alcohol Scale (McLellan, Luborsky, Woody and O’Brien 1980) is a standardized, structured interview that was used to assess alcohol problem severity. Psychometric properties include test-retest reliability of 0.84 and internal consistency alphas averaging 0.86 (Mäkelä 2004). In addition to using it as an outcome, one item was used to identify heavy drinking at baseline, which asked days drank to intoxication over the past 30 days. Heavy drinking was defined as 14 or more days of drinking to intoxication in the past month.
Analysis
Descriptive analyses examined mean scores on outcome measures by study condition over time. Generalized estimating equation (GEE) models were the primary analyses used to test study hypotheses regarding treatment outcomes. Given that our primary aim was to test within and between condition changes over time controlling for selected variables, GEE was an appropriate method for the analyses required. GEE models have the advantage of being able to accommodate categorical and continuous data as well as data that may be correlated over time. In addition, GEE uses all available data in model estimation.
Models (one for each outcome) testing within effects included terms for condition and time (categorical with baseline as referent) and controlled for age, ethnicity, marital status, and education, and exposure to IMI as defined as greater than 1 session (hence 2 or more sessions). Models testing between effects were identical to the within effects models but included an interaction term for condition by time. Treatment effects were assessed for a) the full sample, and b) the subsample of heavy drinking women using ITT analyses and protocol as planned (PP) analyses.
Results
Demographic Characteristics
The mean age of study participants at baseline was 50.9 (sd=11.3). Participants were mostly white (83.3%), married (53.5%) and college educated (61.4%). Nearly all the women (94.4%) reported residence in a stable living situation, such as renting an apartment or owning a house. Over half (50.2%) reported an annual income over $65,000; 25% reported an income over $150,000. There were no significant demographic differences between the two study conditions for the full sample, the PP sample, or for the subsample of heavy drinkers versus non-heavy drinkers. The overall follow-up rate was 87% at 2 months and 86% at 6 months. There were no significant baseline differences on measures of drinking between women who were and were not followed up at 2 months and 6 months.
Engagement in Treatment
Engagement in the treatment protocols was excellent. Overall, 79.4% of the 108 women randomized to IMI completed 7 or more sessions. Women in the IMI condition attended an average of 7.4 (sd=2.3) individual sessions and an average of 5.9 (sd=2.5) of the 9 CIM group sessions. Among the 107 women assigned to SMI, all attended the single session of MI and an average of 5.1(sd=2.7) CIM groups sessions. However, their attendance at the nutrition group, added to achieve time equivalence between the study conditions, was low, at an average of 2.8(sd=2.7) of the 8 nutrition sessions offered.
Descriptive Analysis
Tables 1.1 and 1.2 show means and standard deviations for drinking outcomes at baseline, 2 months and 6 months, separately for all and heavy drinking participants for the ITT and PP analyses, respectively. There were no significant baseline differences between the study conditions on any of the drinking outcomes, that is PDD, PHDD, or the ASI.
Tables 1.1 and 1.2.
Descriptive statistics of outcome measures by condition and time for intent-to-treat a (ITT) and per-protocol b(PP) analysis samples.
| Table 1.1 | ITT Full Sample (N=215) | ITT Heavy Drinkers (N=153) | ||||||
|---|---|---|---|---|---|---|---|---|
| Baseline | 2-month | 6-month | Baseline | 2-month | 6-month | |||
| Condition | Outcome Measures | Mean(sd) | Mean(sd) | Mean(sd) | Condition | Mean(sd) | Mean(sd) | Mean(sd) |
| SMI (n) | (108) | (87) | (86) | SMI | (86 ) | (70) | (70) | |
| TLFB PDD | 0.764 (0.263) | 0.575 (0.327) | 0.560 (0.352) | 0.825 (0.197) | 0.605 (0.314) | 0.604 (0.330) | ||
| TLFB PHDD | 0.517 (0.323) | 0.284 (0.319) | 0.303 (0.342) | 0.581 (0.316) | 0.316 (0.329) | 0.354 (0.354) | ||
| ASI Alcohol^ | 1.739 (0.153) | 1.468 (0.240) | 1.450 (0.250) | 1.794 (0.107) | 1.500 (0.232) | 1.496 (0.233) | ||
| IMI (n) | (107) | (99) | (96) | IMI | (67) | (62) | (61) | |
| TLFB PDD | 0.693 (0.295) | 0.406 (0.315) | 0.466 (0.361) | 0.854 (0.197) | 0.474 (0.324) | 0.536 (0.364) | ||
| TLFB PHDD | 0.491 (0.334) | 0.196 (0.251) | 0.241 (0.324) | 0.619 (0.321) | 0.230 (0.275) | 0.277 (0.351) | ||
| ASI Alcohol^ | 1.704 (0.155) | 1.403 (0.234) | 1.436 (0.239) | 1.788 (0.113) | 1.433 (0.235) | 1.468 (0.241) | ||
| Table 1.2 | PP Sample (N=193) | PP Heavy Drinkers (N=141) | ||||||
| Baseline | 2-month | 6-month | Baseline | 2-month | 6-month | |||
| Condition | Outcome Measures | Mean(sd) | Mean(sd) | Mean(sd) | Condition | Mean(sd) | Mean(sd) | Mean(sd) |
| SMI (n) | (108) | (87) | (86) | SMI | (86) | (70) | (70) | |
| TLFB PDD | 0.764 (0.263) | 0.575 (0.327) | 0.560 (0.352) | 0.825 (0.197) | 0.605 (0.314) | 0.604 (0.330) | ||
| TLFB PHDD | 0.517 (0.323) | 0.284 (0.319) | 0.303 (0.342) | 0.581 (0.316) | 0.316 (0.329) | 0.354 (0.354) | ||
| ASI Alcohol^ | 1.739 (0.153) | 1.468 (0.240) | 1.450 (0.250) | 1.794 (0.107) | 1.500 (0.232) | 1.496 (0.233) | ||
| IMI (n) | (85) | (84) | (81) | IMI | (55) | (55) | (54) | |
| TLFB PDD | 0.713 (0.296) | 0.395 (0.318) | 0.463 (0.364) | 0.867 (0.192) | 0.462 (0.335) | 0.531 (0.368) | ||
| TLFB PHDD | 0.505 (0.346) | 0.180 (0.250) | 0.233 (0.328) | 0.628 (0.332) | 0.211 (0.277) | 0.271 (0.359) | ||
| ASI Alcohol^ | 1.715 (0.152) | 1.398 (0.226) | 1.432 (0.238) | 1.793 (0.115) | 1.417 (0.230) | 1.457 (0.248) | ||
Intent-To-Treat analyses include all participants assigned to the single session of MI (n=108) and all participants assigned to IMI (n=107). Per-Protocol analyses include all SMI participants (n=108) and IMI participants (n=85) who completed 7–9 sessions of the intervention. For the PP analysis, IMI participants who attended less than 7 sessions of the intervention were dropped from the analyses (n=22). SMI and IMI groups did not differ significantly on baseline outcomes in any the full ITT or PP samples. Heavy drinking is defined as 14+ days of heavy drinking at baseline.
ASI Alcohol was log transformed.
Measures of concordance between self-reported alcohol use and EtG metabolite testing were acceptable using a 3-day assessment period. At baseline, 2.4% of the sample had a positive urine test but indicated they did not drink during the past 3 days. At 2-month follow-up non-concordance over 3 days was 8.1% and at 6 months it was 2.7%.
Reductions in means for both study conditions over time (see Tables 1.1 and 1.2) showed a pattern of reduced drinking between baseline and 2 months and the continuation of that improvement at 6 months, both for the full sample and the sample of heavy drinkers.
Generalized Estimating Equation Models
Tables 2.1 and 2.2 show results for GEE models assessing longitudinal changes for the three outcome variables controlling for baseline covariates. For the full sample (Table 2.1, the top half), the significant time effect for all three outcomes indicates that both SMI and IMI participants improved on drinking outcomes from baseline to two months and that the improvements were maintained at 6 months. Non-significant condition by time interactions using the total ITT sample indicate a lack of difference between IMI participants and SMI participants in changes at 2- and 6-month follow-up periods. In contrast, analyses with the heavy drinking participants (Table 2.2, the bottom half) showed that IMI participants had greater improvement than SMI participants did at 2 months on PDD (β = −0.139, p<.05) and PHDD (β= −0.120, p<.05) and on PHDD at 6 months (β = −0.123, p<.05). Changes in ASI scores over time did not differ by study condition at either 2- or 6-months.
Tables 2.1 and 2.2.
Predicting withina and betweenb group effects on outcome measures using generalized estimating equation (GEE) models.
| Table 2.1 | ITT Sample (N=215) | ||||
|---|---|---|---|---|---|
| 2-month (time effect) | 6-month (time effect) | Condition x 2-month | Condition x 6-month | ||
| Outcomes | GEE Models | Coef. [95% CI] | Coef. [95% CI] | Coef. [95% CI] | Coef. [95% CI] |
| TLFB PDD | |||||
| aTime (baseline = referent) | −0.256 [−0.30, −0.21]*** | −0.226 [−0.27, −0.18]*** | |||
| bCondition x Time | −0.215 [−0.28, −0.15]*** | −0.219 [−0.28, −0.16]*** | −0.078 [−0.17, 0.02] | −0.014 [−0.11, 0.08] | |
| cSMI Condition | −0.215 [−0.28, −0.15]*** | −0.219 [−0.28, −0.16]*** | |||
| cIMI Condition | −0.293 [−0.36, −0.22]*** | −0.234 [−0.30, −0.16]*** | |||
| TLFB PHDD | |||||
| aTime (baseline = referent) | −0.269 [−0.31, −0.22]*** | −0.234 [−0.28, −0.19]*** | |||
| bCondition x Time | −0.239 [−0.30, −0.17]*** | −0.213 [−0.28, −0.15]*** | −0.058 [−0.15, 0.03] | −0.041 [−0.13, 0.05] | |
| cSMI Condition | −0.236 [−0.30, −0.17]*** | −0.211 [−0.28, −0.15]*** | |||
| cIMI Condition | −0.296 [−0.36, −0.23]*** | −0.254 [−0.32, −0.19]*** | |||
| ASI Alcohol | |||||
| aTime (baseline = referent) | −0.292 [−0.33, −0.26]*** | −0.281 [−0.32, −0.25]*** | |||
| bCondition x Time | −0.281 [−0.33, −0.23]*** | −0.296 [−0.34, −0.25]*** | −0.021 [−0.09, 0.05] | 0.029 [−0.04, 0.10] | |
| cSMI Condition | −0.280 [−0.33, −0.23]*** | −0.295 [−0.34, −0.25]*** | |||
| cIMI Condition | −0.302 [−0.35, −0.25]*** | −0.267 [−0.32, −0.22]*** | |||
| Table 2.2 | Heavy Drinkers (N=153) | ||||
| 2-month (time effect) | 6-month(time effect) | Condition x 2-month | Condition x 6-month | ||
| Outcomes | GEE Models | Coef. [95% CI] | Coef. [95% CI] | Coef. [95% CI] | Coef. [95% CI] |
| TLFB PDD | |||||
| aTime (baseline = referent) | −0.302 [−0.36, −0.25]*** | −0.267 [−0.32, −0.22]*** | |||
| bCondition x Time | −0.240 [−0.31, −0.18]*** | −0.227 [−0.30, −0.16]*** | −0.139 [−0.25, −0.02] * | −0.090 [−0.20, 0.02] | |
| cSMI Condition | −0.242 [−0.31, −0.18]*** | −0.228 [−0.30, −0.17]*** | |||
| cIMI Condition | −0.377 [−0.47, −0.29]*** | −0.316 [−0.41, −0.23]*** | |||
| TLFB PHDD | |||||
| aTime (baseline = referent) | −0.320 [−0.38, −0.26]*** | −0.273 [−0.33, −0.22]*** | |||
| bCondition x Time | −0.265 [−0.34, −0.19]*** | −0.218 [−0.29, −0.14]*** | −0.120 [−0.23, −0.01] * | −0.123 [−0.24, −0.01] * | |
| cSMI Condition | −0.263 [−0.34, −0.19]*** | −0.216 [−0.30,−0.14]*** | |||
| cIMI Condition | −0.385 [−0.47, −0.30]*** | −0.340 [−0.42, −0.26]*** | |||
| ASI Alcohol | |||||
| aTime (baseline = referent) | −0.324 [−0.36, −0.28]*** | −0.308 [−0.35, −0.27]*** | |||
| bCondition x Time | −0.299 [−0.35, −0.25]*** | −0.299 [−0.36, −0.25]*** | −0.055 [−0.14, 0.03] | −0.022 [−0.11, 0.06] | |
| cSMI Condition | −0.299 [−0.35, −0.25]*** | −0.299 [−0.35, −0.25]*** | |||
| cIMI Condition | −0.353 [−0.42, −0.29]*** | −0.320 [−0.38, −0.26]*** | |||
Note:
Within group models include terms for condition and time.
Between group models include terms for condition, time, and condition*time interaction.
Models are disaggregated on condition and includes a term for time (added here to aid interpretation of interaction models).
All models adjusted for age, ethnicity, education, marital status, and exposure (2+ MI9 sessions; except cSMI Condtion models). Heavy drinking is defined as 14+ days of heavy drinking at baseline.
p<.05
p<.01
p<.001.
Tables 3.1 and 3.2 show findings from the PP GEE models that include IMI participants who received 7 or more sessions. Models with the full PP sample (Table 3.1, top half) indicate a significant reduction in PDD (β= −0.106, p<.05) and a trend (β = −0.091, p=.06) in PHDD for IMI versus SMI participants at 2 months. There were no differences found between study condition at 6 months. GEE models assessing condition by time effects at 2 months using heavy drinkers (Table 3.2, bottom half) showed significantly larger reductions in PDD (β = −0.165, p<.01) and PHDD (β = −0.153, (p<.01) receiving IMI. In addition, there was a trend (β = −0.077, p=.08) for larger reduction of ASI alcohol scores among women receiving IMI. At 6 months, heavy drinkers receiving IMI had significantly greater reductions in PHDD (β= −0.16, p<.05) compared to those receiving SMI and a trend for greater reduction in PDD (β =−0.110, p=.06).
Tables 3.1. and 3.2.
Predicting withina and betweenb group effects on outcome measures using generalized estimating equation (GEE) models^. PP sample.
| Table 3.1 | PP Sample (N=193) | ||||
|---|---|---|---|---|---|
| 2-month | 6-month | Condition x 2-month | Condition x 6-month | ||
| Outcome | GEE Model | Coef [95% CI] | Coef [95% CI] | Coef [95% CI] | Coef [95% CI] |
| TLFB PDD | |||||
| aTime (baseline= referent) | −0.266 [−0.32, −0.21]*** | −0.236 [−0.28, −0.19]*** | |||
| bCondition x Time | −0.215 [−0.28, −0.15]*** | −0.220 [−0.28, −0.16]*** | −0.106 [−0.21, −0.004]* | −0.036 [−0.14, 0.06] | |
| cSMI Condition | −0.215 [−0.28, −0.15]*** | −0.219 [−0.28, −0.16]*** | |||
| cIMI Condition | −0.321 [−0.40, −0.24]*** | −0.256 [−0.33, −0.18]*** | |||
| TLFB PHDD | |||||
| aTime (baseline= referent) | −0.280 [−0.33, −0.23]*** | −0.245 [−0.29, −0.20]*** | |||
| bCondition x Time | −0.238 [−0.30, −0.17]*** | −0.212 [−0.28, −0.15]*** | −0.091 [−0.18, 0.003]^ | −0.069 [−0.16, 0.03] | |
| cSMI Condition | −0.236 [−0.30, −0.17]*** | −0.211 [−0.28, −0.15]*** | |||
| cIMI Condition | −0.328 [−0.40, −0.26]*** | −0.281 [−0.35, −0.21]*** | |||
| ASI Alcohol | |||||
| aTime (baseline= referent) | −0.298 [−0.33, −0.26]*** | −0.290 [−0.33, −0.25]*** | |||
| bCondition x Time | −0.280 [−0.33, −0.23]*** | −0.296 [−0.34, −0.25]*** | −0.035 [−0.11, 0.04] | 0.012 [−0.06, 0.08] | |
| cSMI Condition | −0.280 [−0.33, −0.23]*** | −0.295 [−0.34, −0.25]*** | |||
| cIMI Condition | −0.316 [−0.37, −0.26]*** | −0.284 [−0.34, −0.23]*** | |||
| Table 3.2 | Heavy Drinkers (N=141) | ||||
| 2-month | 6-month | Condition x 2-month | Condition x 6-month | ||
| Outcomes | GEE Models | Coef [95% CI] | Coef [95% CI] | Coef [95% CI] | Coef [95% CI] |
| TLFB PDD | |||||
| aTime (baseline= referent) | −0.309 [−0.37, −0.25]*** | −0.271 [−0.33, −0.22]*** | |||
| bCondition x Time | −0.240 [−0.31, −0.17]*** | −0.227 [−0.29, −0.16]*** | −0.165 [−0.29, −0.04]** | −0.110 [−0.23, 0.01]^ | |
| cSMI Condition | −0.242 [−0.31, −0.17]*** | −0.228 [−0.30, −0.16]*** | |||
| cIMI Condition | −0.405 [−0.51, −0.30]*** | −0.336 [−0.43, −0.24]*** | |||
| TLFB PHDD | |||||
| aTime (baseline= referent) | −0.328 [−0.39, −0.27]*** | −0.277 [−0.34, −0.22]*** | |||
| bCondition x Time | −0.264 [−0.34, −0.19]*** | −0.216 [−0.29, −0.14]*** | −0.153 [−0.27, −0.04]** | −0.146 [−0.26, −0.03]* | |
| cCondition | −0.263 [−0.34, −0.19]*** | −0.216 [−0.29, −0.14]*** | |||
| cIMI Condition | −0.417 [−0.51, −0.33]*** | −0.362 [−0.45, −0.27]*** | |||
| ASI Alcohol | |||||
| aTime (baseline=referent) | −0.332 [−0.37, −0.29]*** | −0.315 [−0.36, −0.27]*** | |||
| bCondition x Time | −0.299 [−0.35, −0.25]*** | −0.299 [−0.35, −0.24]*** | −0.077 [−0.16, 0.01]^ | −0.040 [−0.13, 0.05] | |
| cSMI Condition | −0.299 [−0.35, −0.25]*** | −0.299 [−0.35, −0.25]*** | |||
| cIMI Condition | −0.376 [−0.45, −0.31]*** | −0.338 [−0.41, −0.27]*** | |||
Note: Note:
Within group models include terms for condition and time.
Between group models include terms for condition, time, and condition*time interaction.
Models are disaggregated on condition and includes a term for time (added here to aid interpretation of interaction models).
Models adjusted for age, ethnicity, education, marital status, and exposure (2+ MI9 sessions). Per-Protocol: The SMI Condition includes all participants assigned to the single session of MI; The IMI Condition includes all participants assigned to intensive MI who completed 7–9 session of the intervention. IMI participants who attended less than 7 sessions were dropped from the analyses (n=22). Heavy drinking = 14+ Days of Heavy Drinking at Baseline. ^ ASI Alcohol scale scores are logged.
p<.05
p<.01
p<.001
p<.10.
In a previous analysis of the 2-month data we found higher psychiatric severity predicted worse drinking outcomes (Polcin et al 2018). In the current study we attempted to build on this finding by testing whether psychiatric severity interacted with IMI at 6 months. Interaction models (not shown in the tables) showed that among women who were heavy drinkers there was a significant moderating effect of psychiatric severity on 6-month outcomes for PDD (β=−0.20, p<.05) and for PHDD (β=−0.18, p<.05). Lower severity was associated with better outcome.
Discussion
Study findings confirmed previous analyses showing the benefits of IMI over standard MI at 2-month follow-up (Polcin, et al 2018). Using the full PP sample, we found women receiving IMI had significantly fewer PDD and a trend toward fewer PHDD. Results from the current study also confirmed previous PP analyses at 2 months showing the benefits of IMI were strongest among women who were heavy drinkers. Relative to the comparison condition, heavy drinkers receiving IMI had significantly lower PDD and PHDD as well as a trend toward lower ASI alcohol severity.
The most important finding from the current study is that some of the differences found at 2 months favoring IMI persisted at 6-months. Larger improvements among heavy drinkers in the IMI condition included lower PHDD, which was the case for both the ITT and PP analyses. In the PP analysis, there was also as well as a trend toward lower PDD. These findings are particularly important in light of the challenges the field has faced when attempting to deliver interventions with effects that persist after treatment ends. One approach among researchers (e.g., McLellan et al 2005) has been to emphasize the need for long-term case management and recovery monitoring after treatment ends. However, IMI is proving to be an example of an intervention that results in sustained improvement on its own.
It is noteworthy that all of the within condition analyses showed large reductions in drinking at 2 months with very little attrition of improvements at 6 months. Part of the reason for the improvement may simply be regression to the mean. However, an additional influence might be coming from the effects of the CIM group intervention to which women in both conditions were assigned. Retention in the CIM group for women in both conditions was high. For women in the IMI condition, the mean number of groups attended was 5.9 and for the SMI comparison condition it was 5.1. It is unclear to what extent IMI may have facilitated slightly higher attendance at the CIM groups. However, anecdotal reports from study therapists suggested attendance to group sessions was discussed with some women during IMI sessions along with ways to manage difficult issues that clients faced during group sessions. Therapists who conducted the CIM groups anecdotally reported a high level of engagement and bonding and that women often continued interactions after the groups had ended. Positive responses to the CIM group intervention across both study conditions may have minimized differences between women receiving IMI versus SMI.
Within and between condition improvements for the ITT and PP samples were consistently largest when we used the heavy drinking sample. One implication is that IMI might be best targeted to the subgroup of heavy drinking women who present more serious drinking problems. For women with less serious problems, the combination of a single session of MI plus the CIM group may be sufficient to reduce and then maintain lower levels of drinking at 6 months. When non-heavy drinkers were included in GEE analyses assessing outcomes at the 6-month timepoint, there did not appear to be an advantage to using IMI rather than SMI.
It was notable that 80% of the women in the IMI condition attended 7–9 sessions. This finding provides support for the feasibility of conducting IMI in community settings and IMI’s high level of acceptability among women. The high retention level is important in light of studies showing the dropout rate in the first month of outpatient treatment is commonly 50% or higher and associated with poor outcome (Ball, Carroll, Canning-Ball, and Rounsaville 2006 ). Retention in treatment is one of the strongest predictors of alcohol and drug treatment outcome and may be a particularly strong indicator for women (Ashley, Sverdlov, and Brady 2004),
Study results add to the MI literature in several ways. First, it supports reviews of the literature on MI that suggest a larger number of sessions are associated with better outcomes (e.g., Burke, Arkowitz and Menchola 2003). However, the findings also suggest the benefits of a larger number of MI sessions may not be uniform for all clients or problems. For example, the study of IMI for methamphetamine dependence (Polcin et al. 2014) found benefit in terms of reducing psychiatric severity, but not methamphetamine use. The current study of IMI showed a significant reduction in PDD and PHDD relative to the SMI condition mostly among heavy drinkers. Our moderator analyses showed that women in the IMI condition with higher levels of psychiatric severity did not fare as well as women with lower severity. For these women, there may be a need for a more intensive focus on psychiatric symptoms.
Need for Additional Research
Despite the significant, sustained reductions in drinking noted over 6 months as well as significant between condition differences favoring IMI, there is a need for new studies to examine how to improve IMI. For example, despite the improvements noted, the level of drinking at 6 months was still of some concern. In the total ITT sample, women on average were drinking heavily 24% of the days over the past 60. We need to know more about their level of functioning while drinking at that frequency and what types of interventions might facilitate further improvement. These might include additional sessions beyond the nine sessions now offered or they might include booster sessions that are more dispersed in time after the initial nine sessions.
The option of a larger number of sessions beyond the nine offered in IMI was supported by qualitative investigations of client and therapist views about IMI for MA dependence (Polcin et al. 2015). Clients reported positive experiences participating in IMI and when asked about ways the IMI intervention could be improved, they frequently stated they would like additional sessions over a longer time period. Therapists who provided IMI thought additional sessions would be helpful as well. However, it was unclear to what extent the desire for more sessions reflected a desire to achieve abstinence or a desire to limit the severity of consequences related to substance use. Research is also needed to identify the characteristics of women drinkers who can sustain the benefits of using IMI as a harm reduction approach that involves reduced drinking with fewer consequences and women for whom an abstinence-based approach is indicated.
There continues to be limited information about why MI is effective and that is certainly the case for IMI because it is a more recent adaptation. Although studies have shown that client “change talk” has been found to be related to better outcome (Miller and Rollnick 2012), we are unclear about the relative effects of different interventions leading to change talk and how interventions fuel subsequent changes in substance use. We need more research on standard MI as well as IMI that addresses the effects of specific interventions, when and for whom they are effective, and when some interventions may be contraindicated.
Limitations
The geographic location of the study was in a suburban area in Northern California. The racial and economic characteristics of the women recruited largely reflected the characteristics of the surrounding community. Demographic characteristics of the sample were limited in terms of diversity and additional studies are needed on younger, lower income, and more racially diverse samples. However, the study does respond to the need for more research on alcohol problems among older women (Greenfield et al. 2007) who present different clinical profiles relative to younger women (Al-Otaiba, Epstein, McCrady and Cook 2012).
Acknowledgements:
Supported by NIAAA grant AA022857. Clinical Trials Number NTC02272023.
We acknowledge the support of the New Leaf Treatment Center in Lafayette, CA and the women who participated in the study.
References
- Al-Otaiba Z; Epstein EE; McCrady B and Cook S 2012. Age-based differences in treatment outcome among alcohol-dependent women. Psychology of Addictive Behaviors 26(3): 423–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association; 2000. Diagnostic and Statistical Manual of Mental Disorders DSM-IV-TR (4th ed.). Washington, DC: American Psychiatric Publishing, Inc. [Google Scholar]
- Ashley OS; Sverdlov L; Brady TM 2004. Length of stay among female clients in substance abuse treatment [Accessed: 2014–01-21. Archived by WebCite® at http://www.webcitation.org/6MnbJKSqI] In: Council CL, ed. Health Services Utilization by Individuals with Substance Abuse and Mental Disorders (DHHS Publication No SMA 04–3949, Analytic Series A-25) Rockville, MD: Substance Abuse and Mental Health Services Administration. Office of Applied Studies: 107–32. [Google Scholar]
- Ball SA; Caroll KM; Canning-Ball M,. and Rounsaville BJ 2006. Reasons for dropout from drug abuse treatment: symptoms, personality, and motivation. Addictive Behaviors 31: 320–30. [DOI] [PubMed] [Google Scholar]
- Burke BL; Arkowitz H and Menchola M 2003. The efficacy of motivational interviewing: a meta-analysis of controlled clinical trials. Journal of Consulting and Clinical Psychology 71(5): 843–861. [DOI] [PubMed] [Google Scholar]
- Carroll KM; Farentinos C; Ball SA, Crits-Christoph P, Libby B; Morgenstern J; … Woody GE 2002. MET meets the real world: design issues and clinical strategies in the Clinical Trials Network. Journal of Substance Abuse Treatment 23(2): 73–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeYoung PA 2015. Relational Psychotherapy: A primer (2nd ed.). New York: Routledge. [Google Scholar]
- Erol A and Karpyak VM 2015. Sex and gender-related differences in alcohol use and its consequences: contemporary knowledge and future research considerations. Drug and Alcohol Dependence 156: 1–13. [DOI] [PubMed] [Google Scholar]
- Forman RF; Svikis D; Montoya ID and Blaine J 2004. Selection of a substance use disorder diagnostic instrument by the National Drug Abuse Treatment Clinical Trials Network. Journal of Substance Abuse Treatment 27(1): 1–8. doi: 10.1016/j.jsat.2004.03.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galloway GP; Marinelli-Casey P; Stalcup J; Lord RH; Christian D; Cohen J;, … Vandersloot D 2000. Treatment-as-usual in the methamphetamine treatment project. Journal of Psychoactive Drugs 32(2): 165–175. [DOI] [PubMed] [Google Scholar]
- Galloway GP; Polcin D; Kielstein A; Brown M and Mendelson J 2007. A nine session manual of motivational enhancement therapy for methamphetamine dependence: adherence and efficacy. Journal of Psychoactive Drugs (SARC Suppl. 4): 393–400. doi: 10.1080/02791072.2007.10399900 [DOI] [PubMed]
- Greenfield SF 2002. Women and alcohol use disorders. Harvard Review of Psychiatry 10(2): 76–85. [DOI] [PubMed] [Google Scholar]
- Greenfield SF; Brooks AJ; Gordon SM; Green CA; Kropp F; McHugh RK; … Miele GM 2007. Substance abuse treatment entry, retention, and outcome in women: a review of the literature. Drug and Alcohol Dependence 86(1): 1–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gupta S 2011. Intent to treat concept: A review. Perspectives in Clinical Research 2(3): 9–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Korcha RA; Polcin DL; Evans K; Bond JC and Galloway GP 2014. Intensive motivational interviewing for women with concurrent alcohol problems and methamphetamine dependence. Journal of Substance Abuse Treatment 46(2): 113–119. doi: 10.1016/j.jsat.2013.08.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mäkelä K 2004. Studies of the reliability and validity of the Addiction Severity Index. Addiction, 99(4): 398–410. [DOI] [PubMed] [Google Scholar]
- Martino S; Ball SA; Gallon SL; Hall D; Garcia M; Ceperich S; … Hausotter W 2006. Motivational Interviewing Assessment: Supervisory tools for enhancing proficiency Retrieved from Salem, OR: http://www.motivationalinterview.org/Documents/MIA-STEP.pdf [Google Scholar]
- McLellan AT; Luborsky L; Woody GE and O’Brien CP 1980. An improved diagnostic evaluation instrument for substance abuse patients: the Addiction Severity Index. The Journal of Nervous and Mental Disease 168(1): 26–33. [DOI] [PubMed] [Google Scholar]
- McLellan AT, McKay JR, Forman R, Cacciola JS, Kemp J. 2005. Reconsidering the evaluation of addiction treatment: from retrospective follow-up to concurrent recovery monitoring. Addiction 100: 447–58. [DOI] [PubMed] [Google Scholar]
- Miller WR, & Rollnick S 2012. Motivational Interviewing: Helping people change (3rd ed.). New York: The Guilford Press. [Google Scholar]
- Nuro K; Maccarelli L; Martino S; Ball S; Baker S; Rounsaville B and Carroll K 2006. Yale adherence and competence scale (YACS II) guidelines (Second Edition). Yale University Psychotherapy Development Center Training; Series No. 7: West Haven, CT. [Google Scholar]
- Obert JL and Farentinos C 2000. Motivational Enhancement Therapy (MET) to improve treatment engagement and outcome in subject seeking treatment for substance abuse Washington, DC: Clinical Trials Network: NIDA. [Google Scholar]
- Polcin DL; Bond J; Korcha R; Nayak MB; Galloway GP and Evans K 2014. Randomized trial of Intensive Motivational Interviewing for methamphetamine dependence. Journal of Addictive Diseases 33(3): 253–265. doi: 10.1080/10550887.2014.950029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL; Brown M and Galloway GP 2005. Intensive Motivational Enhancement Therapy Manual Berkeley, CA: Alcohol Research Group. [Google Scholar]
- Polcin DL; Galloway GP; Palmer J and Mains W 2004. The case for high-dose motivational enhancement therapy. Substance Use and Misuse 39(2): 331–343. [DOI] [PubMed] [Google Scholar]
- Polcin DL; Korcha R and Nayak M 2018. Development of Intensive Motivational Interviewing (IMI) and modifications for treating women with alcohol use disorders. Journal of Contemporary Psychotherapy 48(2): 51–59. doi: 10.1007/s10879-017-9370-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Polcin DL; Korcha R; Pugh S; Witbrodt J; Salinardi M; Galloway G … Nelson E 2018. Intensive motivational interviewing for heavy drinking among women. Addictive Disorders and Their Treatment doi: 10.1097/ADT.0000000000000152. [DOI] [PMC free article] [PubMed]
- Polcin DL; Sterling J; Brown T; Brown M; Buscemi R and Korcha R 2015. Client and therapist views about intensive and standard motivational interviewing. Journal of Contemporary Psychotherapy 45(3): 167–176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porta N; Bonet C; and Cove E 2007. Discordance between reported intention-to-treat and per protocol analyses. Journal of Clinical Epidemiology 60(7): 663–669. [DOI] [PubMed] [Google Scholar]
- Sobell LC; Sobell MB; Buchan G; Cleland PA; Fedoroff IC and Leo GI 1996. The reliability of the Timeline Followback method applied to drug, cigarette, and cannabis use. In Association for the Advancement of Behavior Therapy New York, NY: November 21–24. [Google Scholar]
- Vasilaki EI; Hosier SG and Cox WM 2006. The efficacy of motivational interviewing as a brief intervention for excessive drinking: a meta-analytic review. Alcohol and Alcoholism 41(3): 328–335. [DOI] [PubMed] [Google Scholar]
- Walitzer KS and Dearing RL 2006. Gender differences in alcohol and substance use relapse. Clinical Psychology Review 26(2): 128–148. [DOI] [PubMed] [Google Scholar]


