Abstract
Background
Massage and touch have been suggested as a non‐pharmacological alternative or supplement to other treatments offered in order to reduce or manage a range of conditions associated with dementia such as anxiety, agitated behaviour and depression. It has also been suggested that massage and touch may counteract cognitive decline.
Objectives
To assess the effects of a range of massage and touch therapies on conditions associated with dementia, such as anxiety, agitated behaviour and depression, identify any adverse effects, and provide recommendations about future trials.
Search methods
We identified trials from a search of the Specialized Register of the Cochrane Dementia and Cognitive Improvement Group on 12 July 2005 using the terms massage, reflexology, touch and shiatsu. This Register contains records from all major healthcare databases and many ongoing trials databases and is updated regularly. In addition, general and specific literature databases were searched and patient and therapist organizations contacted.
Selection criteria
Randomized controlled trials (RCTs) in which a massage or touch intervention was given to persons suffering from dementia of any type, compared with other treatments or no treatment, and in which effect parameters included measures of behavioural problems, caregiver burden, emotional distress or cognitive abilities, were eligible for inclusion. Furthermore, we employed a set of minimal methodological quality criteria as a selection filter.
Data collection and analysis
We identified 34 references in the initial searches. Of these, seven were actual or possible RCTs, but only two were found to meet the requirements of the set of minimal methodological criteria.
Main results
The very limited amount of reliable evidence available is in favour of massage and touch interventions for problems associated with dementia. However, this evidence addresses only two specific applications: hand massage for the immediate or short‐term reduction of agitated behaviour, and the addition of touch to verbal encouragement to eat for the normalization of nutritional intake. The existing evidence does not support general conclusions about the effect or possible side effects of such interventions. No severe side effects were identified.
Authors' conclusions
Massage and touch may serve as alternatives or complements to other therapies for the management of behavioural, emotional and perhaps other conditions associated with dementia. More research is needed, however, to provide definitive evidence about the benefits of these interventions.
Keywords: Humans, Massage, Touch, Anxiety, Anxiety/therapy, Cognition Disorders, Cognition Disorders/therapy, Dementia, Dementia/psychology, Dementia/therapy, Depression, Depression/therapy, Psychomotor Agitation, Psychomotor Agitation/therapy, Randomized Controlled Trials as Topic
Insufficient evidence to draw conclusions about the possibility that massage and touch interventions are effective for dementia or associated problems
Massage and touch interventions have been proposed as an alternative or supplement to pharmacological and other treatments to counteract anxiety, agitated behaviour, depression, and if possible to slow down cognitive decline in people with dementia. This review provides an overview of existing research on the use of massage for people with dementia. Eighteen studies of the effects of massage interventions were located, but only two small studies were of a sufficient methodological rigour to count as evidence to answer the question of effect.
The small amount of evidence currently available is in favour of massage and touch interventions, but is too limited in scope to allow for general conclusions. Further, high‐quality randomized controlled trials are required.
Background
Massage and touch are among the range of pharmacological and psychosocial interventions used in dementia care with the aim of counteracting cognitive decline, reducing the frequent accompanying problems of depression, anxiety, aggression and related psychological and behavioural manifestations, improving quality of life, or improving general health and ultimately survival (Cohen‐Mansfield 2001). Anxiety, agitated behaviour and depression associated with dementia require substantial resources of professional care either in the home or in residential units (Williams‐Burgess1996).
Massage and touch are sometimes perceived, in the context of traditional or commonsense interactions with patients, as belonging to a 'tacit knowledge' of care that would be a matter of course in a setting that was not institutionalized or professional. However, even if touch therapy aims only to reintroduce something which has been 'lost' in the professionalization and institutionalization of care, it may still turn out to be a relatively effective, inexpensive and low‐risk (Ernst 2003) intervention in the given setting (Anon 2003). Furthermore, the professional training of massage/touch therapists may add something beyond an implicit culture of caring touch, in terms of scope or intensity (Bush 2001; Kostrzewa 2000; Moraga 2000; Vanderbilt 2000).
Various theoretical models have been proposed to explain the possible positive effects of massage and touch for persons with dementia. One physiological model is based on the observation that the sensation of touch or proximity has an immediate calming, reassuring influence, mediated, for example, by the production of oxytocin, and hence modifies the symptoms of discomfort, agitation and mood disorders (Lund 2002; Uvnäs‐Moberg 1998). Neurological models of action have also been proposed (Scherder 1995a). Another more psychological kind of model sees touch and massage as a way to 'stay in touch' and retain a sense of meaningful, reassuring communication even when words begin to fail (Bush 2001; Vanderbilt 2000). The sensory stimulation involved may also help to activate non‐verbalized patterns of memories and meanings (Opie 1999). Under such assumptions it would be conceivable that massage and touch modalities could also help to counteract the progressive decline of cognitive abilities if this decline is at least partly due to lack of use and meaningful stimulation. In any case there seems to be a broad consensus that the potential short‐term effects lie primarily in behaviour, mood and well‐being, while the longer‐term effects may include a limited degree of modification of cognitive decline.
A wide range of massage and touch modalities are described in the recent literature. One study reports, without further specification, the use of a 'massage' component of a combined intervention (Smallwood 2001); another reports only that a professional massage therapist was in charge of such a component (Brooker 1997). Most studies describe the parts of the patients' bodies which were massaged or touched: in many cases these are large areas of the body, particularly back, shoulders, and back of the neck (Rowe 1999; Sansone 2000). In other cases the hands, arms and shoulders (Kim 1999), only the hands (Snyder 1995; Snyder 1995a) or only the lower legs and feet (Malaquin‐Pavan 1997) were massaged or touched. Many studies report types of stroking and styles of touching in general or technical terms: tender touch with large strokes (Sansone 2000), slow strokes (Rowe 1999), expressive touch (Kim 1999), rubbing, kneading (Scherder 1995), and effleurage (Bowles 2002). In some cases the massage/touch is described as part of a general communicative situation including encouragement and friendly words (Kim 1999). In other cases a caregiver's calm state of mind is an important element of the intervention, even to the extent that the caregivers prepare themselves through a suggestive or meditative exercise (Malaquin‐Pavan 1997; Rowe 1999). This is also the case in the more or less standardized therapy form 'therapeutic touch' (TT) in which the therapist's hands are held near the patient's body but not in physical contact. In four of the studies, the intervention used was TT alone or in combination (Giasson 1999; Snyder 1995; Snyder 1995a; Woods 2002). Several other more or less established therapeutic systems enter as elements in the interventions reported: reflexology (Malaquin‐Pavan 1997), acupressure (Kilstoff 1998) and aromatherapy (Kilstoff 1998). The number of treatments given per patient in a study varies: in most studies it is between 10 and 50. The frequency of treatments is fixed at once or twice per day in most cases, but in a few cases it is variable according to need. The duration of each treatment varies from 1 to 30 minutes, but in a few cases this was not reported. Most studies give some information on the provider of the massage or touch intervention: nursing staff (Malaquin‐Pavan 1997), nursing staff working to a specified protocol (Snyder 1995; Snyder 1995a), nursing staff trained by a therapist (Brooker 1997; Sansone 2000), therapist (Bowles 2002; Scherder 1995), investigator (Woods 2002), research assistants trained by investigator (Kim 1999), family members trained by nursing staff (Kilstoff 1998; Rowe 1999). In at least two cases it can be argued that the intervention tested was not really massage or touch per se, but training with follow up given to a caregiver at home or at an institution, so that the receiver of the intervention was not the patient but the patient‐caregiver dyad (Kilstoff 1998; Rowe 1999; Sansone 2000). There is considerable heterogeneity in the style, the categories and the degree of precision with which the studies specify the interventions involved.
Studies address questions of the effect of massage and touch interventions on one or several outcome variables in the general class of agitated behaviour, mood, discomfort and pain, while some also address the impact of massage/touch on cognitive/practical ability (Kilstoff 1998). A few studies combine the measurement of concrete clinical outcomes with physiological correlates which either belong to a hypothesized mechanism of action or are taken to express an outcome of anxiety, stress, relaxation, etc (Fraser 1993; Kim 1999; Snyder 1995).
Study designs include non‐randomized controlled trials (Snyder 1995), cross‐over studies (Snyder 1995a), time‐series without a control group (Kilstoff 1998; Kim 1999; Malaquin‐Pavan 1997; Rowe 1999; Woods 2002), single case studies (Brooker 1997), 'action research' ‐ a method of repeatedly and systematically involving the feedback of several types of actors in the development of an intervention, involving elements of qualitative research methodology (Kilstoff 1998), and 'demonstration project' in which qualitative study of the practical experience with implementation at an institution, and the meaningful experience of family members involved, are given at least as much weight as quantitative findings (Sansone 2000).
A large number of different rating scales, psychological tests and physiological measurements were used in the studies as measures of the outcomes described. A list of outcome measures is given in Additional Table 2. It is interesting to note that, although agitated behaviour and anxiety/relaxation are outcomes in most of the studies, no two studies measure them with the same instruments (except for those by Scherder et al., who repeated most of the elements of their own design; see 'Excluded studies'). Ratings of behaviour, mood etc. are typically performed by nursing staff or researchers, but in several cases this is not specified even though tests for reliability and validity are quoted. This review will adopt a sufficiently broad definition of massage and touch‐related therapies to ensure that all the interventions of this family which are actually in use in dementia care can be included.
Table 1.
Outcome measures
| Study | Outcome measures |
| Smallwood 2001 | behavioral disturbances (rating of sampled video recordings, applying a behaviour category scheme, Bowie 1993) |
| Sansone 2000 | pain (author's own scale, rated by patient and/or staff), anxiety/agitation (adapted standard scale "CARE" in which nursing staff record their observations) |
| Rowe 1999 | episodes of agitation (Agitated Behavior Rating Scale Scoring Guide (ABRSSG) adapted from Woods 1993, rated by caregivers) dementia related behaviour leading to caregiver/family distress (Behaviour Symptom Rating Scale (BSRS), Rabins 1994, rated by caregivers) |
| Kim 1999 | anxiety (measured as pulse rate) dysfunctional behaviour (Behavioral Pathology in Alzheimer's Disease Scale (E‐BEHAVE‐AD), Auer 1996) |
| Kilstoff 1998 | levels of dementia and dependency (Revised Elderly Persons' Disability Scale (REPDS), Fleming R 1993), satisfaction, caregiver burden and other qualitative evaluations (interviews, focus groups etc.) |
| Malaquin‐Pavan 1997 | behaviour rating scale, rated by physician, psychologist, nurse (reference to Peoples, 1985, unidentifiable). several scales of level of dementia video recordings, sleep registration |
| Brooker 1997 | disturbed behaviour ‐ authors' own (individualised) rating scales |
| Snyder 1995 | relaxation ‐ rating scale (Luiselli 1982), count of instances of anxious behaviour ‐ authors' own individualised checklist physical relaxation ‐ pulse rate |
| Snyder 1995a | count of agitated behaviours during care activities ‐ authors' own individualised checklist |
| Remington 2002 | agitation ‐ CMAI Agitation Inventory (Cohen‐Mansfield 1995) modified from retrospective data collection to observer format according to Chrisman 1991. |
| Scherder 1995 | (I) memory ‐ selected subscales from the Wechsler Memory Scale‐Revised (Wechsler 1984), from the Eight Word Test (Lindenboom 1989), from the Rivermead Beh Memory Test (Wilson 1987), and from the Groninger Intelligence Test (Snijders 1983) (II) affective behaviour ‐‐ Beoorderlingsschal voor Oudere Patiënten (Van der Kam 1971), combined with a behaviour inventory constructed by the authors |
| Scherder 1995a | as Scherder 1995, part (II) |
| Scherder 1998 | as Scherder 1995, part (I) |
| Giasson 1999 | discomfort ‐ EI‐DTA (Alzheimer‐specific scale) Hurley 1992 |
| Woods 2002 | frequency & intensity of agitated behavior, rating scale (Agitated Behaviour Rating Scale ‐ ABRS) modified from Bliwise 1993, Woods 1993. |
| Bowles 2002 | severity of dementia, MMSE "mini‐mental state examination" (Folsten 1975), dementia‐related behaviors, author's own scale with a specific subscale for resistance to nursing care. |
| Fraser 1993 | anxiety, STAI Spielberger Self‐Evaluation Questionnaire, Spielberger 1970 systolic and diastolic blood pressure, heart rate. |
| Eaton 1986 | nutrition intake, calculated on the basis of evaluation of returned plates, an ad‐hoc method developed by the authors. |
Objectives
Primary To assess the effectiveness of a range of massage and touch therapies offered to patients suffering from dementia.
Secondary To give an overview of forms of massage which have been applied and studied in the context of dementia care. To systematically present information on experienced harmful effects and practical difficulties encountered. To provide recommendations for research in this area.
Methods
Criteria for considering studies for this review
Types of studies
We included randomised controlled trials (RCTs) in the review. We used studies with other research designs to provide background information only and have discussed these above.
As the sensation and awareness of touch is likely to be essential to these interventions, study design elements such as placebo control, and blinding of patient and therapist, are probably not relevant and we did not give them positive weight in the review. However, we considered blinding in the assessment of response to be one important element of study quality. Useful information may be obtained from trials comparing a full massage session with a session containing some of its elements only (e.g. aromatic oil alone) or merely talking to a sympathetic therapist; thus we included these also.
We set no limits on the length of trials or the number of measurements made. Outcome measures should, however, be appropriate in the context of the length of the trial and the number of treatments. Although it makes sense to look for changes in 'soft' measures of well‐being and behaviour in the short term as a result of single sessions or a few treatments, effects on 'harder' measures of cognitive ability and general health could be expected to emerge only after longer‐term evaluation.
Types of participants
Patients with a diagnosis of dementia of any type, and receiving standard professional care for this condition, in their homes, in hospitals, or in residential institutions.
Types of interventions
Any type of massage and touch compared with other treatments, no treatment or placebo. This includes regular massage forms ('Swedish', 'Esalen' etc.) in which a touch with some pressure is applied in a moving way on parts of the body (typically the neck, shoulders or hands), therapies focused on finger pressure on specific points (reflexology, shiatsu), and 'therapeutic touch' (i.e. interventions where the therapist's hands may be held at a short distance from the patient's body rather than in direct physical contact). In this context, a 'short distance' means close enough to be perceived by patients as warm, intimate and bodily present (excluding, for example, prayer and distant healing.)
Types of outcome measures
1. We sought reported changes in the frequency and severity of various types of agitated behaviour as observed by staff or investigators (using any rating method, and short term as well as long term), and in the emotional well‐being and quality of life of the patients (rated by any method by staff, investigators and/or patients themselves). 2. Additionally, we considered outcomes in terms of cognitive abilities, survival, medication use, and caregiver burden. 3. We calculated overall response within a given type of outcome where appropriate. 4. We also considered global response, given that considerable individual differences in response are to be expected.
Search methods for identification of studies
We identified trials from a search of the Cochrane Dementia and Cognitive Improvement Group Specialized Register on 12 July 2005, using the terms massage, reflexology, touch and shiatsu.
This Specialized Register at that time contained records from the following databases:
CENTRAL (Cochrane Central Register of Controlled Trials): January 2005 (issue 1)
MEDLINE: 1966 to 2005/02
EMBASE: 1980 to 2005/01
PsycINFO: 1887 to 2005/01
CINAHL: 1982 to 2004/12
SIGLE (Grey Literature in Europe): 1980 to 2004/06
ISTP (Index to Scientific and Technical Proceedings): to May 2000
INSIDE (BL database of Conference Proceedings and Journals): to June 2000
Aslib Index to Theses (UK and Ireland theses): 1970 to March 2003
Dissertation Abstracts (USA): 1861 to March 2003
http://clinicalstudies.info.nih.gov/
National Research Register: issue 2/2005
ClinicalTrials.gov (last searched June 2005)
LILACS (Latin American and Caribbean Health Science Literature): last searched April 2003
http://www.forestclinicaltrials.com/CTR/CTRController/CTRHome (last searched 2 July 2005)
ClinicalStudyResults.org (last searched 1 July 2005)
http://www.lillytrials.com/index.shtml (last searched 30 June 2005)
ISRCTN Register: last searched 2 July 2005
The search strategies we used to identify relevant records in MEDLINE, EMBASE, PsycINFO and CINAHL can be found in the Group's module on the Cochrane Library. We made additional direct searches on MEDLINE, EMBASE, MANTIS, PsycINFO and CINAHL, for combinations of terms for the relevant conditions (Alzheimer's or dementia), interventions (massage, touch, therapeutic touch, shiatsu or acupressure) and study types (randomized controlled trials or controlled trials). Finally, a number of patients' and therapists' organizations were asked if they knew of unpublished data from relevant trials, and reference lists from retrieved publications were checked for further relevant reports.
Almost all published trials on complementary/alternative medicine are less than 20 years old, so we considered the search strategy likely to be comprehensive without the need for handsearching.
Data collection and analysis
The searches described yielded a total of 34 references. We obtained hard copies whenever possible. In the case of two articles, it was not possible to obtain abstracts or hard copies, but in both cases correspondence with the authors established that the article contained no original data that were otherwise unobtainable.
Two reviewers performed independently an initial screening for relevance. This first screening resulted in a list of 18 potentially relevant studies, eight of these being definite or possible randomized controlled trials.
In a second and final round of screening, two reviewers (NVH, TJ) independently evaluated the 8 articles that were potentially relevant RCTs for eligibility for inclusion in the review. We developed an electronic form through consultation and testing with all reviewers, with a quality (validity and bias) checklist constructed and agreed beforehand. Following the example of the Cochrane review on music therapy for dementia (Vink 2005), we used an adapted form of the 'Delphi' checklist developed in Verhagen 1998. We consulted chapter 8 of the Cochrane Reviewers' Handbook (Alderson 2004) to ensure that all relevant aspects were covered in the checklist. On testing the checklist we found it was not helpful to define a score with or without a threshold score to determine exclusion or inclusion. We also observed that two of the checklist's standard criteria ‐ blinding of patient, and blinding of provider ‐ were not possible or relevant in any of the protocols studied in the eight reports, and probably will not be so in any reasonable trial of a massage or touch intervention. Hence, as anticipated in our protocol, we did not consider failure to meet these two criteria to be a relevant criterion of study quality (while of course criteria such as blinded assessment would still be relevant). Finally, the test run of the 'Delphi' checklist made us aware of the desirability of an eighth criterion, which was added to the seven remaining in our adapted version of Verhagen's 'Delphi' list. This added criterion is the requirement that there be one well‐defined primary outcome which clearly corresponds to a primary hypothesis that the study is designed to test.
For five of the eight articles considered at this stage, additional information about study quality or the availability of raw data was sought from the authors. Several authors kindly made additional information and data available to us (see 'Acknowledgements').
Results
Description of studies
Only two small trials (Eaton 1986; Remington 2002) with a total of 110 participants met the quality criteria for inclusion in the review. In this section we give brief descriptions of the two included and six excluded trials.
Included Studies Eaton 1986: RCT assessing the effect on nutritional intake of "verbal encouragement with touch" during meals, compared with verbal encouragement alone. Forty‐two institutionalized patients with a diagnosis of chronic organic brain syndrome (the article does not specify any procedure or criterion for this diagnosis) were randomly assigned to the two intervention groups. The experimental intervention was given at two meals per day for one week, with a pretreatment and post‐treatment period of one week each, in which all patients received "verbal encouragement" only. Nutritional intake was estimated in each case by blinded evaluators on the basis of food remaining on the patients' plates. This study met most of the quality requirements but the randomization procedure is not described and it is not possible to determine whether allocation was concealed. It is questionable whether the outcome variables of nutritional intake fall within the field defined in our protocol (mood problems, affective behaviour and cognitive decay), but both reviewers found that they do belong to the intended overall problem of care for the health and quality of life for persons suffering from dementia. However, data are not reported in sufficient detail to enter into further analysis. Both reviewers were in doubt as to whether the outcome ‐ nutritional intake ‐ should be considered as belonging to the cluster of outcomes defined in the protocol. It was finally decided that it does, for material reasons. Nutritional intake can be seen as a surrogate measure of the behavioural and mood problems associated with dementia, and the authors explicitly characterize it as such in their introduction: "Persons with chronic organic brain syndrome who are confused and disoriented often wander from the table and leave the food untouched..."
Remington 2002: RCT assessing a short‐term effect of calming music and hand massage by comparing four treatment arms (calming music, hand massage, simultaneous calming music and hand massage, no intervention). Sixty‐eight nursing home residents with dementia (medical records contained a diagnosis of Alzheimer's disease, multi‐infarct dementia or senile dementia) were randomly allocated using a sealed envelope procedure to four groups with 17 persons in each group. The intervention lasted for 10 minutes, and was given to each patient once. Treatment effect on 'agitation level' was evaluated by using a modified version of the Cohen‐Mansfield Agitation Inventory (CMAI) administered by trained research assistants who were blinded to treatment allocation when possible (obviously this is not possible for measurements during the intervention). This study met all of the quality requirements except that the description of the procedure indicates that patients could have been excluded after allocation (if they had a CMAI score of 0 at baseline). However, the authors have indicated that in fact no such exclusions happened. Furthermore, they kindly supplied additional data which allowed us to enter the study into RevMan for meta‐analysis. However, in the absence of any other comparable data, this adds little to the data analysis already given in the published paper.
Excluded studies Giasson 1999: RCT assessing the short‐term effect of a 'therapeutic touch' intervention on patient 'discomfort' measured by a validated behaviour observation scale. Twenty‐seven nursing home residents diagnosed as suffering from dementia of the Alzheimer type, stage 5 to 7, were randomized to an intervention group (n = 16) and a control group (n = 11) which received 'simple presence' as a control intervention. Interventions lasted 10 minutes and were given once per day for five consecutive days. Observers and evaluators were blinded to group allocation, and observation took place three times: immediately before the first intervention, and immediately after interventions 3 and 5. The authors report a decrease in discomfort levels which was significantly greater in the treatment than in the control group. However, the report lacks a clear summary of means and standard deviations (or other measures of variation) for effect data. Furthermore, the allocation procedure is not specified further than the indication that it involved randomization ('facon aleatoire'). In particular, there is no indication of concealed allocation. No explanation is given for the large difference in group sizes, and there is no information on compliance and dropouts. Hence it seems likely that there were either irregularities in the allocation procedure or very large dropout rates.
Scherder 1995; Scherder 1995a; Scherder 1998: Three reports of a series of very similar controlled trials ‐ according to correspondence with the authors, the latter two are in fact reports from the same trial, but using different outcome measures. The trials assess the long‐term effects of a combined intervention of transcutaneous electrical nerve stimulation (TENS) and back massage (Scherder 1995) or back massage alone (Scherder 1995a; Scherder 1998) on cognitive function as measured by a battery of standard tests (Scherder 1995a), affective behaviour as measured by another battery of tests (Scherder 1998) or a combination (Scherder 1995). In all cases, the control intervention was sham TENS. In all of the group's studies, 16 nursing home residents with a diagnosis of dementia of probable Alzheimer's type were allocated to treatment and control groups, and interventions were given for 30 minutes per day for six weeks. Evaluators were blinded to group allocation, and pre‐, post‐ and delayed scores (measured after a 'washout' period of six weeks) were recorded. The authors report statistically significant improvements between pre‐ and post‐values in some of the several scales and subscales used, but only small and insignificant differences between pre‐ and delayed values. Only one of the reports (Scherder 1998) specifies that allocation was random, but according to correspondence with the authors, the trials were not really randomized because a pairing procedure was performed by the investigators concurrently with their decision about inclusion: in particular, allocation was clearly not concealed. Furthermore, the fact that many outcome measures are reported without a priori establishment of a primary outcome measure (e.g. in the form of a calculated combined score) makes the possibility of selective reporting a serious drawback in study quality. Data are not reported in a sufficient degree of detail to allow us to construct combined scores and perform calculations on these, nor were the authors able to supply the additional data this would require. Scherder et al. (Scherder 1995b) have also published reports on a third very similar trial in which the intervention was TENS alone.
Smallwood 2001: Randomized controlled trial assessing the long‐term effect on behaviour disturbance of a combination of aromatherapy massage compared with two control interventions: aromatherapy with conversation, and massage alone. Twenty‐one district general hospital inpatients with a diagnosis of dementia were randomly allocated to the three arms, seven patients in each. Interventions were given twice a week for four weeks. Behaviour disturbance was assessed by sampled video recording by evaluators blinded to treatment allocation. The investigators report a trend towards a greater reduction in behavioural disturbance in the aromatherapy plus massage arm than in the aromatherapy plus conversation arm, but this reached statistical significance only when analysis was restricted to a particular subset of data, namely measurements made during one particular time period during the day. This study was excluded from the Cochrane review of 'Aromatherapy for dementia' (Thorgrimsen 2003) because of the unmotivated use of the interaction with time of day in data analysis (which again raises issues of selective reporting). Furthermore, one dropout is reported but it is not stated how this was treated in the data analysis, and no details are given of the type of massage offered, or the duration of each treatment. The investigators did not respond to requests for additional information.
Bowles 2002: CCT assessing the effect on cognitive function, dementia‐related behaviour and resistance to nursing care of massage with an essential oil blend compared with control massage with plain base cream not containing the essential oil blend. Fifty‐six elderly residents in a care facility who had been diagnosed with moderate to severe dementia (using the MMSE) were divided into groups matched for mobility, sex, and type and severity of dementia. Interventions were given in a crossover fashion, with group A receiving the treatment intervention for four weeks while group B received the control; the two groups then received the alternate intervention for another four weeks. Cognitive function was assessed the day before the residents commenced essential oil treatment and the day after they finished receiving the treatment (i.e. a 28‐day separation) using the MMSE (Folstein 1975). Dementia‐related behaviour was assessed using some measures described in the Cohen‐Mansfield Agitation Inventory (Cohen‐Mansfield 1986). The frequency and severity of other behaviours such as confusion were measured via a bespoke scale (0 to 3 where 0 = no occurrence of the behaviour and 3 = behaviour occurring more than five times or continuously during the nursing shift). Resistance to nursing care was measured on a scale of 1 to 3 where 1 = person requiring verbal redirection away from the problem behaviour and 3 = person requiring the physical intervention of two nurses (ie extremely difficult to redirect). The trialists observed an increase in behaviours classified as resistance to nursing care in the massage plus essential oil blend group in contrast to the massage alone group. The report suggests this unexpected finding be reinterpreted as an improvement in alertness. However, the trial could not be included in this review, nor the results used because of the lack of randomization of participants.
Risk of bias in included studies
As discussed in the descriptions of excluded and included studies above, the two included studies appeared methodologically sound, except that in Eaton 1986 the randomization procedure is not described and it is not possible to determine whether allocation was concealed. Furthermore, both of these trials were very small (only 17 and 21 patients in the active treatment groups).
Effects of interventions
The included studies provide evidence within two limited subfields of the overall question of effectiveness of massage and touch in dementia.
One author (Remington 2002) found a decrease in agitated behaviour (rated using the modified CMAI scale) which was greater in the group receiving hand massage than in the group receiving no treatment. This treatment effect was consistently found compared with baseline for measurements taken during treatment, immediately after treatment, and one hour after treatment, and it was practically identical between the three groups receiving treatment (hand massage, calming music or both). The magnitude of this treatment effect (about 15 CMAI scale units or 75%) appears to be comparable with the effects of other treatments, pharmacological as well as non‐pharmacological (Opie 1999; Snowden 2003), but it should be noted that evaluation methods and scales vary considerably and also that this study only assesses immediate and very short‐term effects of a single treatment. Eaton 1986 found a significant increase in mean intake of calories (from 570 to 740 cal/day) as well as protein (from 32 to 43 g/day) in the group receiving verbal encouragement with touch, but no change in the control group receiving verbal encouragement only ‐ a difference they report to be statistically significant.
The only adequate data available for entry into RevMan's statistical module was the additional set made available by Dr Remington (see Comparison 01). In the absence of comparable data our analysis merely repeats the study's conclusion of a positive and statistically significant difference between scores in the hand massage group and the no treatment group.
Discussion
Although a wide range of research questions and methodologies have been applied to this family of interventions, questions of clinical effectiveness clearly dominate. However, few RCTs were identified, and only two of these were found to be of sufficient methodological quality to produce reliable evidence regarding effectiveness. This evidence relates only to one small aspect of the overall question of clinical benefits of massage and touch in dementia. Both of the included studies assessed short‐term or immediate effects on behaviour. Longer‐term effects, effects on mood or depression, and effects in terms of degree of cognitive dysfunction have all been addressed only by small studies which lack sufficient methodological rigour to count as reliable evidence. Although the available reliable evidence supports the use of massage and touch, it is so limited in scope that it is not possible to draw general conclusions about benefits in dementia. However, a number of recommendations can be made on the basis of the recent wider literature described in the 'Introduction' above, none of which could be formally included in the meta‐analysis of this review.
First, several studies shift the focus away from the patient as the sole target of the intervention to patient‐caregiver 'dyads', or aim to produce benefits in terms of communication with staff and family members or the need of caregivers and family to feel they can contribute something meaningful to the care of the person with dementia. Further development of such perspectives may help to indicate how basic sensory contact and stimulation could interact with conditions affecting cognitive abilities. Secondly, the review identified a number of intervention trials rich in good ideas and features of high quality, which would often have required a limited additional effort to meet the criteria for inclusion. Given the relatively small resources available for research in complementary and alternative medicine, it is essential to ensure that trials provide high‐quality evidence.
When blinding of patient and provider is impossible or irrelevant, as seems generally the case with massage and touch interventions, it makes no sense to consider its absence as a lack of quality. Similarly it is important that this is not taken to imply that other quality criteria are poor: it should be possible to maintain a well‐described randomization procedure, concealed allocation and a well‐defined primary effect parameter.
Thirdly, the existing literature points to a number of research approaches which could help answer a range of different questions on these interventions. One approach concerns possible mechanisms of action (biochemical, psychological, etc.), another the interaction of culture, language, perception of body and sense of meaningful interactions, and a third the problems, possibilities and costs of involving new procedures and caregiver qualifications in institutional practice. These questions need to be addressed alongside those of clinical efficacy. Some of the studies attempt to answer several types of questions at once ‐ this may have led to difficulties in satisfying several sets of study quality criteria simultaneously.
Finally, some of the studies make an interesting observation which may or may not reflect a general feature of massage and perhaps other sensory/psychosocial therapies: the effect of two different interventions in this family did not seem to be additive, but rather the beneficial effect of combined interventions seemed to have the same magnitude as that of one intervention alone.
Most of these wider literature studies report individual and average improvements with respect to central effect measures. When using single case designs significant pre‐ or post‐improvements are sometimes reported but the clinical significance of these is hard to establish without a control group. In addition, some of the individual case studies show the opposite pattern, with worsening scores on outcome measures such as agitation. No studies report outspoken adverse effects of the interventions, although in a few cases a patient was reported to find the treatment uncomfortable and/or withdraw from the study.
We conclude that the existing published research provides no basis for determining whether any of the many types of touch and massage are more effective than others, or how to best characterize and delimit the possible benefits of these interventions. Future research should include multidisciplinary, hypothesis‐driven work. Some of the many creative ideas expressed in existing work (e.g. action research to refine intervention, or the focus on families and carer‐patient 'dyads' as the target of intervention) should lead to clear, operational definitions and hypotheses which can be tested in future clinical trials.
Finally, in order to make results useful for practice, it is important to give precise descriptions of interventions. The specifications should be in concrete as well as in general terms, as there is not yet a well‐established system of general terms for complementary and alternative therapies (Murphy 2003). A minimal set of information on a massage or touch intervention must include: who gives the massage or touch; the duration, frequency, situation and time of day; physical positions of provider and patient; parts of body touched; the force applied (if any); the style and tempo of movements; the conversation or silence accompanying them; and any required mental or spiritual preparation of the therapist. If the intervention is standardized according to the training or instructions of a particular school of massage etc., this should also be specified.
Authors' conclusions
There is insufficient evidence regarding the efficacy of massage/touch interventions, and insufficient data to conduct a meta‐analysis. Some evidence is available to support the efficacy of two specific applications: the use of hand massage for an immediate and short‐term reduction of agitated behaviour, and the addition of touch to verbal encouragement to eat for the normalization of nutritional intake.
Given the limited evidence available, there is a need for further, more methodologically rigorous research. Well‐designed RCTs are needed to add to the evidence base in this area. In particular, trials should include a well‐described randomization procedure, concealed allocation, and a well‐defined primary effect parameter. It is important to give careful and precise descriptions of the interventions used.
Acknowledgements
We gratefully acknowledge the contributions of:
Consumer editor, Susanne Bjerregaard
Dr Snyder, Dr Scherder, and Dr Remington for giving us access to additional data and other information on their studies
The State Library at the University of Aarhus for retrieving hard copies of all the studies considered in this review
ViFAB for providing technical facilities and enabling NVH to work on this review as part of his function in the institution
Data and analyses
Comparison 1.
Massage vs no massage
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 mean agitation score ‐ during treatment | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 6.24 [2.94, 9.54] |
| 1.1 during treatment | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 6.24 [2.94, 9.54] |
| 2 mean agitation score ‐ immediately after treatment | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 7.83 [4.30, 11.36] |
| 2.1 immediately after treatment | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 7.83 [4.30, 11.36] |
| 3 mean agitation score ‐ 1 hr after treatment | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 12.12 [6.58, 17.66] |
| 3.1 1 hr after treatment | 1 | 34 | Mean Difference (IV, Fixed, 95% CI) | 12.12 [6.58, 17.66] |
Analysis 1.1.
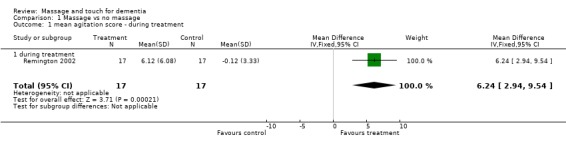
Comparison 1 Massage vs no massage, Outcome 1 mean agitation score ‐ during treatment.
Analysis 1.2.
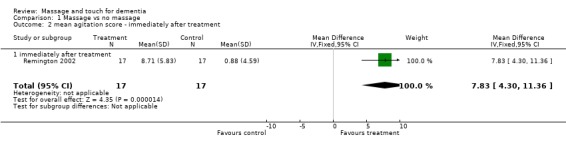
Comparison 1 Massage vs no massage, Outcome 2 mean agitation score ‐ immediately after treatment.
Analysis 1.3.
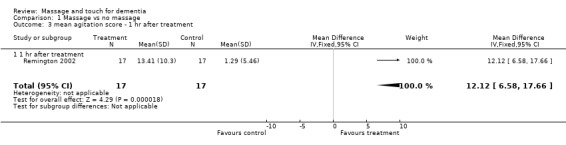
Comparison 1 Massage vs no massage, Outcome 3 mean agitation score ‐ 1 hr after treatment.
What's new
| Date | Event | Description |
|---|---|---|
| 23 May 2008 | Amended | Converted to new review format. |
History
Protocol first published: Issue 4, 2004 Review first published: Issue 4, 2006
| Date | Event | Description |
|---|---|---|
| 3 August 2006 | New citation required and conclusions have changed | Substantive amendment |
Characteristics of studies
Characteristics of included studies [ordered by study ID]
| Methods | RCT | |
| Participants | 42 (21+21) nursing home residents with a diagnosis of "Chronic organic brain syndrome" | |
| Interventions | (1) gentle touch on forearm accompanying encouragement to eat (2) no touch (one week, two meals per day, several times per meal) | |
| Outcomes | nutritional intake | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Unclear risk | B ‐ Unclear |
| Methods | RCT | |
| Participants | 68 (4x17) nursing home residents with a diagnosis of dementia | |
| Interventions | (1) calming music (2) hand massage (3) calming music and hand massage (4) no intervention (One treatment of 10 min. Only groups 2 and 4 are considered in this review) | |
| Outcomes | Agitation (CMAI score) | |
| Notes | ||
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Allocation concealment? | Low risk | A ‐ Adequate |
CMAI: Cohen‐Mansfield Agitation Inventory
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Bowles 2002 | Compares two combined interventions in which the massage component is identical |
| Giasson 1999 | Allocation procedure not specified, except for an indication that it was random, but there is no explanation for a large difference in group sizes (n = 16 therapeutic touch and n = 11 "simple presence" control) and no account for compliance and dropouts. |
| Scherder 1995 | Allocation is quasi‐random and not concealed; many outcome measures are reported without an a priori establishment of a primary outcome measure |
| Scherder 1995a | As Scherder 1995 |
| Scherder 1998 | As Scherder 1995 |
| Smallwood 2001 | An unmotivated splitting of results according to 'time of day' results in an apparent positive treatment effect in part of the material; one dropout is reported but it is not stated how this was treated in the data analysis; no details given of the type of massage or duration of treatment |
Contributions of authors
TJ and NVH: Jointly responsible for all decisions about inclusion and assessment of quality of data, and for interpretation of the results of analyses and summaries.
NVH: Database searches, literature retrieval, programming of data registration forms and data transfer into RevMan, statistical analysis, summaries of other information about studies.
LOE: Arbiter in selection of trials for inclusion, discussions on interpretations and conclusions.
Contact editor: Linda Clare
Consumer editor: Susanne Bjerregaard
This review has been peer reviewed in June 2006
Sources of support
Internal sources
ViFAB ‐ the Knowledge and Research Center for Alternative Medicine (Ministry of Health), Denmark.
External sources
No sources of support supplied
Declarations of interest
None known
Edited (no change to conclusions)
References
References to studies included in this review
- Eaton M, Mitchell Bonair IL, Friedmann E. The effect of touch on nutritional intake of chronic organic brain syndrome patients. Journals of Gerontology 1986;41(5):611‐6. [DOI] [PubMed] [Google Scholar]
- Remington R. Calming music and hand massage with agitated elderly. Nursing Resources 2002;51(5):317‐323. [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
- Bowles EJ, Griffiths DM, Quirk L, Brownrigg A, Croot K. Effects of essential oils and touch on resistance to nursing care procedures and other dementia‐related behaviours in a residential care facility. International Journal of Aromatherapy 2002;12(1):22‐9. [Google Scholar]
- Giasson M, Leroux G, Tardif H, Bouchard L. Therapeutic touch. L'Infirmiere du Quebec 1999;6(6):38‐47. [PubMed] [Google Scholar]
- Scherder E, Bouma A, Steen L. Effects of Simultaneously Applied Short‐Term Transcutaneous Electrical Nerve‐Stimulation and Tactile Stimulation on Memory and Affective Behavior of Patients with Probable Alzheimers‐Disease. Behavioural Neurology 1995;8(1):3‐13. [DOI] [PubMed] [Google Scholar]
- Scherder E, Bouma A, Steen L. The effects of peripheral tactile stimulation on memory in patients with probable Alzheimer's disease. American Journal of Alzheimer's Disease 1995;May/June:15‐21. [Google Scholar]
- Scherder E, Bouma A, Steen L. Effects of peripheral tactile nerve stimulation of affective behavior of patients with probable Alzheimer's disease.. American Journal of Alzheimer's Disease 1998;March/April:15‐21. [Google Scholar]
- Smallwood J, Brown R, Coulter F, Irvine E, Copland C. Aromatherapy and behaviour disturbances in dementia: a randomized controlled trial. International Journal of Geriatric Psychiatry 2001;16(10):1010‐1013. [DOI] [PubMed] [Google Scholar]
Additional references
- Alderson P, Green S, Higgins JPT, editors. Cochrane Reviewers’ Handbook 4.2.2 [updated December 2003]. The Cochrane Library 2004, Issue 1. [Google Scholar]
- Anon. Aromatherapy trial. Journal of Dementia Care 2001i;9(6):38. [Google Scholar]
- Anon. Alert / early warning [Mjuk massage vid demenssjukdom]. National Swedish MTA Institute2003.
- Armstrong L, Wright A. Communication in day care: talking without words. Journal of Dementia Care 2002;10(5):18‐19. [Google Scholar]
- Aveyard B, Sykes M, Doherty D. Therapeutic touch in dementia care. Nurs Older People 2002;14(6):20‐21. [PubMed] [Google Scholar]
- Braverman DL, Schulman RA. Massage techniques in rehabilitation medicine. Phys Med Rehabil Clin N Am 1999;10(3):631‐49, ix. [PubMed] [Google Scholar]
- Brooker DJ, Snape M, Johnson E, Ward D, Payne M. Single case evaluation of the effects of aromatherapy and massage on disturbed behaviour in severe dementia. British Journal of Clinical Psychology 1997;36(2):287‐96. [DOI] [PubMed] [Google Scholar]
- Bush E. The use of human touch to improve the well‐being of older adults: a holistic nursing intervention. Journal of holistic nursing 2001;19(3):256‐70. [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield J. Agitated behaviours in the elderly: II. Preliminary results in the cognitively deteriorated. Journal of the American Geriatrics Society 1986;10:722‐727. [DOI] [PubMed] [Google Scholar]
- Cohen‐Mansfield J. Nonpharmacological Interventions for Inappropriate Behaviors in Dementia. Am J Geriatr Psyciatry 2001;9(4):361‐81. [PubMed] [Google Scholar]
- Ernst E. The safety of massage therapy. Rheumatology (Oxford) 2003;42(9):1101‐1106. [DOI] [PubMed] [Google Scholar]
- Field TM. Massage therapy effects. Am Psychol 1998;53(12):1270‐81. [DOI] [PubMed] [Google Scholar]
- Folstein MF, Folstein SE. Mini‐Mental State – a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research 1975;12:189‐198. [DOI] [PubMed] [Google Scholar]
- Fraser J, Kerr JR. Psychophysiological effects of back massage on elderly institutionalized patients. Journal of Advanced Nursing 1993;18(2):238‐45. [DOI] [PubMed] [Google Scholar]
- Gaylord S, Crotty N. Enhancing function with complementary therapies in geriatric rehabilitation. Topics in Geriatric Rehabilitation 2002;18(2):63‐79. [Google Scholar]
- Kilstoff K, Chenoweth L. New approaches to health and well‐being for dementia day‐care clients, family carers and day‐care staff. Int J Nurs Pract 1998;4(2):70‐83. [DOI] [PubMed] [Google Scholar]
- Kim EJ, Buschmann MT. The effect of expressive physical touch on patients with dementia. Int J Nurs Stud 1999;36(3):235‐243. [DOI] [PubMed] [Google Scholar]
- Kostrzewa S. [Death with dignity in the old age home: consideration for the needs of demented patients]. Pflege Zeitschrift 2000;53(11):757‐62. [PubMed] [Google Scholar]
- Lund I, Long‐Chuan Y, Uvnas‐Moberg K, Wang J, Yu C, Kurosawa M, Agren G, Rosen A, Lekman M, Lundeberg T. Repeated massage‐like stimulation induces long‐term effects on nociception: contribution of oxytocinergic mechanisms. Eur J Neurosci 2002;16(2):330‐8. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Malaquin‐Pavan E. [Therapeutic benefit of touch‐massage in the overall management of demented elderly]. Recherche en Soins Infirmiers 1997;49:11‐66. [PubMed] [Google Scholar]
- Meehan TC. Therapeutic touch as a nursing intervention. Journal of Advanced Nursing 1998;28(1):117‐25. [DOI] [PubMed] [Google Scholar]
- Moraga M. Therapeutic touch as part of the care for the aged. Soins Gerontol 2000;21:30‐33. [PubMed] [Google Scholar]
- Murphy LS, Reinsch S, Najm WI, Dickerson VM, Seffinger MA, Adams A. Searching biomedical databases on complementary medicine: the use of controlled vocabulary among authors, indexers and investigators. BMC ‐ Complementary and Alternative Medicine 2003;3(1):3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nelson D. The power of touch in facility care. Massage and Bodywork 2001;16(1):12‐18. [Google Scholar]
- Opie J, Rosewarne R, O'Connor DW. The efficacy of psychosocial approaches to behaviour disorders in dementia: a systematic literature review. Australian and New Zealand Journal of Psychiatry 1999;33(6):789‐99. [DOI] [PubMed] [Google Scholar]
- Richards KC. Sleep promotion. Critical care nursing clinics of North America 1996;8(1):39‐52. [PubMed] [Google Scholar]
- Roberson L. The importance of touch for the patient with dementia. Home Health Nurse 2003;21(1):16‐19. [DOI] [PubMed] [Google Scholar]
- Rowe M, Alfred D. The effectiveness of slow‐stroke massage in diffusing agitated behaviors in individuals with Alzheimer's disease. Journal of Gerontology Nursing 1999;25(6):22‐34. [DOI] [PubMed] [Google Scholar]
- Sansone P, Schmitt L. Providing tender touch massage to elderly nursing home residents: a demonstration project. Geriatric Nursing 2000;21(6):303‐308. [DOI] [PubMed] [Google Scholar]
- Scherder EJ, Bouma A, Steen AM. Effects of short‐term transcutaneous electrical nerve stimulation on memory and affective behaviour in patients with probable Alzheimer's disease. Behav Brain Res 1995;67(2):211‐9. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Snowden M, Sato K, Roy‐Byrne P. Assessment and treatment of nursing home residents with depression or behavioral symptoms associated with dementia: a review of the literature. Journal of the American Geriatrics Society 2003;51(9):1305‐1317. [DOI] [PubMed] [Google Scholar]
- Snyder M, Egan EC, Burns KR. Interventions for decreasing agitation behaviors in persons with dementia. Journal of Gerontology Nursing 1995;21(7):34‐40. [DOI] [PubMed] [Google Scholar]
- Snyder M, Egan EC, Burns KR. Efficacy of hand massage in decreasing agitation behaviors associated with care activities in persons with dementia. Geriatric Nursing 1995;16(2):60‐63. [DOI] [PubMed] [Google Scholar]
- Thorgrimsen L, Spector A, Wiles A, Orrell M. Aroma therapy for dementia. Cochrane Database of Systematic Reviews 2003, Issue 3. [DOI: 10.1002/14651858.CD003150] [DOI] [PubMed] [Google Scholar]
- Uvnäs‐Moberg K. Oxytocin may mediate the benefits of positive social interaction and emotions. Psychoimmunoendocrinology 1998;23(8):819‐35. [DOI] [PubMed] [Google Scholar]
- Vanderbilt S. It's never too late to touch: massage emerges as a lifeline to dementia patients. Massage and Bodywork 2000;15(3):140‐44. [Google Scholar]
- Verhagen AP, Vet HC, Bie RA, Kessels AG, Boers M, Bouter LM, Knipschild PG. The Delphi list: a criteria list for quality assessment of randomized clinical trials for conducting. J Clin Epidemiol 1998;51(12):1235‐1241. [MEDLINE: ] [DOI] [PubMed] [Google Scholar]
- Vink AC, Birks JS, Buinsma MS, Scholten RJS. Music therapy for people with dementia. Cochrane Database of Systematic Reviews 2005, Issue 1. [DOI] [PubMed] [Google Scholar]
- Wiles A, Brooker DJ. Complementary therapies in dementia care. Journal of Dementia Care 2003;11(3):31‐36. [Google Scholar]
- Williams‐Burgess RN, Ugarriza D, Gabbai M. Agitation in Older Persons with Dementia: A Research Synthesis. The Online Journal of Knowledge Synthesis for Nursing 1996;3(13):U4‐U22. [Google Scholar]
- Woods DL, Dimond M. The effect of therapeutic touch on agitated behavior and cortisol in persons with Alzheimer's disease. Biological Research for Nursing 2002;4(2):104‐114. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
- Viggo Hansen N, Jørgensen T, Ørtenblad L. Massage and touch for dementia. Cochrane Database of Systematic Reviews 2006, Issue 4. [DOI: 10.1002/14651858.CD004989.pub2] [DOI] [PMC free article] [PubMed] [Google Scholar]


