Abstract
Objectives:
In this study, we assessed whether commercials for electronic cigarettes (e-cigarettes) influence the use of e-cigarettes, cigarettes, and cigars among high-risk youth in southern California.
Methods:
We recruited students (N = 1060) from 29 alternative high schools into a prospective cohort study. We used multilevel Poisson regression models to examine whether exposure to e-cigarette commercials and perceptions of their appeal predicted increased use of e-cigarettes, cigarettes, and cigars one year later. We also tested the potential moderating effect of gender and ethnicity.
Results:
Models with and without covariates suggest that exposure to e-cigarette commercials is a statistically significant predictor of increased use of e-cigarettes. When gender was added to the models as a moderator, the relationships between commercial exposure and future use of e-cigarettes and cigars were found to be stronger among females. Unadjusted and adjusted models also indicated that students with favorable perceptions of e-cigarette commercials reported greater use of e-cigarettes, cigarettes, and cigars one year later.
Conclusions:
E-cigarette commercials may play an important role in persuading high-risk youth to use nicotine and tobacco products. Extending the Broadcast Advertising Ban of 1971 to include a broader range of products may be critical to preventing future generations from becoming addicted to nicotine.
Keywords: electronic cigarettes, cigarettes, cigars, tobacco advertising, tobacco control
In the 1960s, television commercials were the preeminent form of tobacco advertising.1 Following the release of a report by the Surgeon General in 1964 that detailed the dangers of smoking,2 the Federal Communications Commission (FCC) took steps in 1967 to protect the public by mandating that the persuasive power of cigarette commercials be counterbalanced by anti-smoking ads. Within a year, the 3 major networks had broadcast over 1300 anti-smoking commercials.3 By 1971, the Broadcast Advertising Ban ended cigarette advertising on television. Tobacco companies embraced this change as a preferable alternative to the relentless stream of counteradvertising.4
In the midst of the 2013 Super Bowl, a 30-second regional ad for NJOY e-cigarettes signaled the reemergence of television commercials promoting nicotine products. The ad instantly reached over 10 million viewers.5 It concluded with a statement that e-cigarettes contained nicotine and were ‘not for sale to minors.’6 No mention was made of the health risks. Research at the time reported adverse health effects in individuals who used e-cigarettes.7–9 Subsequent research revealed the presence of potential carcinogens including formaldehyde, acetaldehyde, and acrolein.10 Researchers conducting a systematic review of 76 studies concluded that e-cigarettes could not be considered a safe product.11 Emerging evidence also suggested that while no sidestream vapor was generated from e-cigarettes, vapor exhaled by users involuntarily exposed non-users to harmful compounds.12–14
The Broadcast Advertising Ban had been implemented to protect the public from a dangerous product. E-cigarettes also posed risks,11,15,16 but the same restrictions were not applied.17 Some argued that e-cigarettes deserved special consideration as a potentially safer alternative to traditional cigarettes.18–21 Others argued that this was a strawman comparison because most products are a safer alternative to traditional cigarettes.11,22 Moreover, the harm reduction argument presumed that individuals would only use e-cigarettes. In a meta-analysis involving 17,389 adolescents and young adults, youth who tried e-cigarettes were significantly more likely to try cigarettes.23
Examining the Effect of E-cigarette Commercials on High-risk Youth
Research indicates that e-cigarettes have the potential to save lives.24 However, the advertising strategy implemented by the nicotine and tobacco industry suggests a different priority. Commercials for e-cigarettes have been aired alongside television programs with substantial youth audiences.25 An estimated 24 million youth have been exposed to imagery that glamorizes the use of nicotine products.26 Given the high awareness of e-cigarettes among youth,27 as well as evidence from experimental studies showing that youth exposed to e-cigarette advertising are more likely to use e-cigarettes,28–30 it is not surprising that by 2019 an estimated 3 million high school students reported the use of e-cigarettes in the past 30 days.31
Although prior studies32 have examined the impact of tobacco advertising on adolescent smoking, to our knowledge, no study has examined the effects of e-cigarette commercials on high-risk youth in the United States (US). One such population that warrants investigation is students who are referred to alternative high schools due to poor academic performance, conduct problems, or extenuating life circumstances. Reports of past month use of traditional cigarettes among these students have ranged from 38.7% to 56.3%33–37 compared to the national rate of 8.1%.31 Based on prior research,38–43 it was hypothesized that the frequency with which these high-risk youth viewed e-cigarette commercials and their reaction to those commercials would predict future use of e-cigarettes, cigarettes, and cigars even after adjusting for multiple covariates commonly cited by the tobacco industry.44
METHODS
Sampling
Using data obtained from the California Department of Education, we identified 183 eligible alternative high schools. We classified schools as eligible if they had at least 100 students and were within 100 miles of the program offices in Claremont, California. After receiving approval from the Claremont Graduate University Institutional Review Board, all schools were contacted in a randomly selected order and invited to participate in the study. Schools were accepted on a first-come, first-served basis until 29 sites were enrolled. Research staff visited the schools between October 14, 2014 and May 18, 2015. Interest forms were distributed to 6870 students who were in attendance at the schools. Completed forms were returned by 2726 students. Each student that returned a form was assigned to a specific staff member. The staff member obtained written consent and provided a link to a Web-based survey. Parental consent and youth assent were obtained for students under the age of 18. All students were given until September 1, 2015 to complete a 90-minute survey programmed with Inquisit 4 software (http://www.millisecond.com/). Data were gathered on the variables presented as well as a number of additional variables beyond the scope of this article.45,46 A total of 1060 students took part in the initial assessment. Each of these students was given a $45 gift card to compensate them for their time.
We tracked students using procedures modeled on longitudinal studies conducted with high-risk populations.47–50 Contact points included: (1) a reminder flyer mailed to each student 6 months prior to the one-year follow-up assessment; (2) a personalized text message delivered on the student’s birthday; (3) a scripted email exchange performed 3 months prior to the follow-up assessment; and (4) a scripted text message exchange initiated one month before the follow-up assessment. One-year follow-up assessments were conducted between September 21, 2015 and September 1, 2016. The average follow-up assessment took place 330 days (SD = 26.6) after the initial assessment. Most assessments (96.6%) were administered on a Web-enabled device utilizing Inquisit or Qualtrics (http://www.qualtrics.com). Students without access to a Web-enabled device (3.4%) were given the option to take a computer-assisted telephone interview. Each student that completed an assessment received a $50 gift card. The completion rate was 87.1%. Overall, 137 students did not complete a follow-up assessment due to withdrawal from the study (5.8%), incarceration (0.7%), or failure to respond to repeated contact attempts (93.5%).
Measures
Demographics.
We asked students to report their gender and ethnicity. Students also provided their birthdate which was used to calculate their age at the time of the initial assessment.
Exposure to e-cigarette commercials.
A single item utilized in prior research51,52 was administered to quantify exposure to e-cigarette commercials. We asked students: About how often did you see an electronic cigarette commercial in the last 6 months? Response options included ‘Never’, ‘Less than once a month’, ‘Once a month’, ‘2–3 times a month’, ‘Once a week’, ‘2–6 times a week’, and ‘Every day’.
Likeability of e-cigarette commercials (α = .77).
We used a 5-item scale modeled on prior studies53–56 to gauge the extent to which students liked the e-cigarette commercials they had seen. The first 3 questions were: When you see electronic cigarette commercials on TV or online…, ‘Do you think they are funny? ‘, ‘Do you think they are sexy? ‘, ‘Do you wish you were like the people in the commercials?’ Response options for all 3 items were: ‘No, never’, ‘No, usually not’, ‘Yes, usually’, and ‘Yes, always’. The next question was: When you see electronic cigarette commercials, how often do you pay attention to them? Response options included: ‘Never’, ‘Some of the time’, ‘Most of the time’, and ‘Always’. The final question was: Of all the commercials you see, how much do you like electronic cigarette commercials? Students responded on a 4-point scale ranging from ‘I like electronic cigarette commercials the least’ to ‘I like electronic cigarette commercials the most.’
Exposure to other forms of advertising for nicotine and tobacco products (α = .81).
To account for the influence of other advertising channels, a 4-item scale was adapted from the National Youth Tobacco Survey (NYTS).57 The scale assessed the extent to which students had been exposed to: (1) newspaper and magazine ads; (2) posters and signs; (3) radio spots; and (4) Web banners for nicotine and tobacco products. Response options included: ‘None’, ‘1–3 times in the past 30 days’, ‘1–3 times per week’, ‘Daily or almost daily’, and ‘More than once a day’.
Family use of nicotine and tobacco products.
Numerous studies have documented the impact of family tobacco use on youth.58–62 To adjust for this effect, 3 items were adapted from the NYTS to determine whether students had at least one family member who currently used: (1) cigarettes; (2) e-cigarettes, vaporizers, or vape pens; or (3) cigars, cigarillos, or little cigars.
Peer use of nicotine and tobacco products.
The influence of peers on youth tobacco use is another well-documented finding.63–67 To adjust for the effect of peer use of nicotine and tobacco products, 3 items were adapted from the California Student Tobacco Survey68 to measure whether students had at least one friend who currently used cigarettes, e-cigarettes, vaporizers, or vape pens, or cigars, cigarillos, or little cigars.
Use of nicotine and tobacco products in the past 30 days.
To facilitate comparisons across products, a previously validated drug use questionnaire69,70 was modified to inquire about cigarettes, e-cigarettes, vaporizers, or vape pens, and cigars, cigarillos, or little cigars. Students were asked how many times they had used each product in the past 30 days. Response options included: ‘0 times’, ‘1–10 times’, ‘11–20 times’, ‘21–30 times’, ‘31–40 times’, ‘41–50 times’, ‘51–60 times’, ‘61–70 times’, ‘71–80 times’, ‘81–90 times’, and ‘91+ times’. The response provided at the one-year follow-up assessment was used as the dependent variable and the responses for each product at the initial assessment were integrated as covariates.71
Data Analysis
The sample consisted of 1060 students nested within 29 schools. Calculating the intra-class correlation revealed that 5.5% to 11.7% of the variance in the use of e-cigarettes, cigarettes, and cigars could be attributed to clustering effects at the school level. Two approaches were considered to account for similarities between students attending the same school.72 The first approach involved the use of generalized estimating equations to model population-averaged responses. The second approach utilized generalized linear mixed models to estimate subject-specific responses. Based on prior research indicating that marginal models have inflated type 1 error rates when analyzing datasets with a relatively small number of clusters (ie, schools),73–75 the decision was made to use generalized linear mixed models. Because the dependent variables exhibited a count distribution and consisted of only non-negative integers, a multilevel Poisson regression was used in all analyses. Continuous independent variables included in the Poisson regression models were group-mean centered.
A comparison between participants with complete data versus those with missing responses revealed no statistically significant differences by gender (45.8% male vs 55.7% male, p = .916), ethnicity (78.1% Hispanic vs 72.1% Hispanic, p = .956), age (17.5 vs 17.5, p = .550), exposure to e-cigarette commercials (1.73 vs 1.80, p = .610), or the perceived likeability of e-cigarette commercials (0.54 vs 0.57, p = .483). Use of e-cigarettes (0.53 vs 0.56, p = .779), cigarettes (0.43 vs 0.54, p = .412), and cigars (0.27 vs 0.37, p = .362) in the past 30 days at the initial assessment were also not significantly different. Based on this preliminary analysis, missing responses were assumed to be missing at random and a multiple imputation analysis was performed using SAS PROC MI and MIANALYZE.76
Models that assessed whether exposure to e-cigarette commercials predicted product use in the past 30 days at the one-year follow-up assessment were estimated utilizing SAS PROC GLIMMIX. The first set of models analyzed raw data and used LaPlace’s method77 to assess the unadjusted effect of exposure. The second set of models analyzed forty imputed datasets78 and incorporated multiple covariates including gender (female = 0 vs male = 1), ethnicity (Non-Hispanic = 0 vs Hispanic = 1), age, family use of nicotine and tobacco products (nonuse = 0 vs use = 1), peer use of nicotine and tobacco products (nonuse = 0 vs use = 1), use of nicotine and tobacco products in the past 30 days at the initial assessment, and exposure to promotions for nicotine and tobacco products through other advertising channels. A third set of models tested whether ethnicity or gender moderated the relationships between exposure to e-cigarette commercials at the initial assessment and the use of nicotine and tobacco products at the one-year follow-up assessment.
The next set of analyses was restricted to a sub-sample of 720 students who had seen at least one e-cigarette commercial. The first set of models used raw data to estimate the unadjusted effect of e-cigarette commercial exposure and likeability. The second set of models incorporated the same covariates utilized previously. The third set of models examined whether there was a statistically significant interaction between the likeability of e-cigarette commercials and either ethnicity or gender.
RESULTS
Descriptive Statistics
The sample was 50.7% male and 75.2% Hispanic as Table 1 shows. The mean age was 17.5 years (SD = 0.9). Compared to high school students in California,79 students in the current sample reported greater use of e-cigarettes (19.8% vs 8.6%, p < .001), cigarettes (15.9% vs 4.3%, p < .001), and cigars (11.9% vs 4.3%, p < .001) in the past 30 days. Students attending alternative high schools also reported greater use of 2 or more nicotine or tobacco products in the past 30 days (13.1% vs 6.1%, p < .001).
Table 1.
Descriptive Statistics for 1060 Students from 29 Alternative High Schools
| Initial Assessment | |
| Gender, N (%) | |
| Male | 534 (50.7%) |
| Female | 520 (49.3%) |
| Ethnicity, N (%) | |
| Hispanic | 777 (75.2%) |
| Non-Hispanic | 256 (24.8%) |
| Age, Mean (SD) | 17.5 (0.9) |
| Exposure to E-cigarette Commercials, Mean (SD) | 1.8 (1.9) |
| Likeability of E-cigarette Commercials, Mean (SD) | 0.6 (0.5) |
| Exposure to other Forms of NTP Advertising, Mean (SD) | 1.2 (1.0) |
| Family Use of NTPs, N (%) | |
| E-cigarettes | 150 (15.3%) |
| Cigarettes | 283 (29.7%) |
| Cigars | 102 (10.4%) |
| Peer Use of NTPs, N (%) | |
| E-cigarettes | 435 (52.8%) |
| Cigarettes | 435 (51.1%) |
| Cigars | 230 (24.1%) |
| Use of NTPs in the Past 30 Days, N (%) | |
| E-cigarettes | 198 (19.8%) |
| Cigarettes | 160 (15.9%) |
| Cigars | 119 (11.9%) |
| Only One Product | 152 (15.4%) |
| 2 Products | 73 (7.4%) |
| All 3 Products | 56 (5.7%) |
| One Year Follow-uv Assessment | |
| Use of NTPs in the Past 30 Days, N (%) | |
| E-cigarettes | 124 (14.2%) |
| Cigarettes | 134 (15.3%) |
| Cigars | 88 (10.1%) |
| Only One Product | 110 (12.8%) |
| 2 Products | 58 (6.7%) |
| All 3 Products | 35 (4.1%) |
Note.
NTPs = Nicotine and tobacco products
More than two-thirds of the students (67.9%) indicated they had seen at least one e-cigarette commercial. More than one-third (39.2%) had seen 2 or more commercials in the past month. Among the 720 students who had seen a commercial, 68.1% reported watching the commercial on television while 30.3% reported seeing it online.
Exposure to E-cigarette Commercials and Product Use One Year Later
The first set of models estimated the unadjusted effect of exposure to e-cigarette commercials. Table 2 presents the unstandardized coefficients (b), standard errors (SE), and p-values. A one unit change in exposure to e-cigarette commercials was associated with a 21.8% increase in the number of times students used e-cigarettes one year later (b = 0.20, SE = 0.03, p < .001), a 10.0% increase in the number of times students smoked cigarettes (b = 0.10, SE = 0.02, p < .001), and a 10.1% increase in the number of times students smoked cigars (b = 0.10, SE = 0.03, p = .001).
Table 2.
Multilevel Poisson Regression Models Examining the Relationship between E-cigarette Commercial Exposure and Product Use One Year Later Among 1060 Alternative High School Students
| Variables | E-cigarettes | Cigarettes | Cigars | ||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | b | SE | p | |
| Unadjusted Models | |||||||||
| Exposure to E-cigarette Commercials | 0.20 | 0.03 | <.001 | 0.10 | 0.02 | <.001 | 0.10 | 0.03 | .001 |
| Covariate Adjusted Models | |||||||||
| Gender (Male) | 0.76 | 0.13 | <.001 | 0.37 | 0.10 | <.001 | 0.81 | 0.13 | <.001 |
| Ethnicity (Hispanic) | −0.35 | 0.13 | .010 | −0.53 | 0.10 | <.001 | −0.59 | 0.13 | <.001 |
| Age | 0.01 | 0.07 | .856 | 0.01 | 0.06 | .925 | −0.11 | 0.07 | .123 |
| Family Use of E-cigarettes | 0.25 | 0.17 | .144 | 0.24 | 0.13 | .074 | 0.21 | 0.17 | .214 |
| Family Use of Cigarettes | −0.15 | 0.16 | .368 | 0.28 | 0.12 | .022 | −0.05 | 0.17 | .777 |
| Family Use of Cigars | 0.15 | 0.22 | .491 | −0.02 | 0.15 | .893 | 0.31 | 0.19 | .100 |
| Peer Use of E-cigarettes | 0.02 | 0.19 | .915 | −0.21 | 0.14 | .155 | 0.30 | 0.19 | .121 |
| Peer Use of Cigarettes | 0.39 | 0.18 | .032 | 0.55 | 0.19 | .004 | −0.36 | 0.19 | .066 |
| Peer Use of Cigars | −0.16 | 0.14 | .265 | 0.24 | 0.13 | .074 | 0.61 | 0.15 | <.001 |
| Previous Use of E-cigarettes | 0.17 | 0.02 | <.001 | −0.02 | 0.02 | .328 | −0.03 | 0.03 | .318 |
| Previous Use of Cigarettes | 0.03 | 0.03 | .178 | 0.22 | 0.02 | <.001 | 0.16 | 0.03 | <.001 |
| Previous Use of Cigars | −0.23 | 0.06 | <.001 | −0.02 | 0.03 | .567 | 0.06 | 0.03 | .052 |
| Exposure to other Tobacco Advertising | 0.10 | 0.06 | .125 | 0.09 | 0.05 | .089 | 0.23 | 0.06 | <.001 |
| Exposure to E-cigarette Commercials | 0.07 | 0.03 | .024 | 0.02 | 0.03 | .412 | −0.01 | 0.03 | .742 |
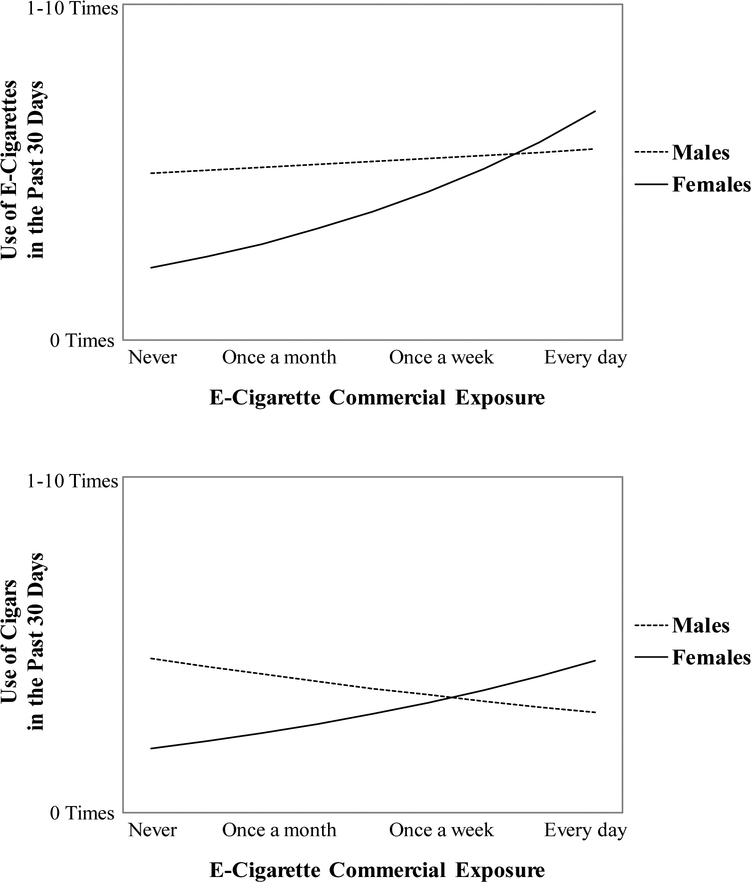
The second set of models integrated multiple covariates. Use of nicotine and tobacco products in the past 30 days at the initial assessment was a statistically significant predictor in most of the models. Other variables, such as gender and ethnicity, were also relevant. After accounting for these covariates, exposure to e-cigarette commercials remained a statistically significant predictor of e-cigarette use (b = 0.07, SE = 0.03, p = .024) but not cigarette use (b = 0.02, SE = 0.03, p = .412) or cigar use (b = −0.01, SE = 0.03, p = .742). A third set of analyses that examined the moderating effect of ethnicity revealed that the interaction between ethnicity and exposure to e-cigarette commercials was not statistically significant in models estimating the use of e-cigarettes (b = 0.11, SE = 0.06, p = .056), cigarettes (b = 0.08, SE = 0.05, p = .143), or cigars (b = 0.07, SE = 0.07, p = .294). However, gender had a moderating effect on the relationship between e-cigarette commercial exposure and the use of e-cigarettes (b = −0.17, SE = 0.07, p = .011) and cigars (b = −0.22, SE = 0.07, p = .003). Table 3 presents parameter estimates and Figure 1 provides a visualization of the interaction. The interaction between exposure to e-cigarette commercials and gender was not statistically significant in models estimating the use of cigarettes (b = −0.04, SE = 0.05, p = .446) at the one-year follow-up assessment.
Table 3.
Multilevel Poisson Regression Models Examining the Moderating Effect of Gender on the Relationship between E-cigarette Commercial Exposure and Product Use One Year Later among 1060 Alternative High School Students
| Variables | E-cigarettes | Cigarettes | Cigars | ||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | b | SE | p | |
| Gender (Male) | 0.84 | 0.14 | <.001 | 0.38 | 0.10 | <.001 | 0.88 | 0.14 | <.001 |
| Ethnicity (Hispanic) | −0.33 | 0.13 | .015 | −0.53 | 0.10 | <.001 | −0.59 | 0.13 | <.001 |
| Age | 0.01 | 0.07 | .860 | 0.01 | 0.06 | .932 | −0.12 | 0.07 | .108 |
| Family Use of E-cigarettes | 0.24 | 0.17 | .162 | 0.24 | 0.13 | .078 | 0.18 | 0.17 | .275 |
| Family Use of Cigarettes | −0.14 | 0.16 | .395 | 0.28 | 0.12 | .022 | −0.05 | 0.17 | .783 |
| Family Use of Cigars | 0.20 | 0.22 | .353 | −0.01 | 0.15 | .960 | 0.38 | 0.19 | .043 |
| Peer Use of E-cigarettes | 0.02 | 0.19 | .904 | −0.21 | 0.14 | .142 | 0.34 | 0.19 | .085 |
| Peer Use of Cigarettes | 0.40 | 0.18 | .026 | 0.55 | 0.19 | .004 | −0.37 | 0.20 | .058 |
| Peer Use of Cigars | −0.20 | 0.14 | .167 | 0.24 | 0.13 | .079 | 0.58 | 0.15 | <.001 |
| Previous Use of E-cigarettes | 0.18 | 0.02 | <.001 | −0.02 | 0.02 | .352 | −0.03 | 0.03 | .327 |
| Previous Use of Cigarettes | 0.03 | 0.03 | .209 | 0.22 | 0.02 | <.001 | 0.16 | 0.03 | <.001 |
| Previous Use of Cigars | −0.23 | 0.06 | <.001 | −0.02 | 0.03 | .570 | 0.06 | 0.03 | .046 |
| Exposure to other Tobacco Advertising | 0.08 | 0.06 | .204 | 0.09 | 0.05 | .107 | 0.22 | 0.06 | <.001 |
| Exposure to E-cigarette Commercials | 0.19 | 0.06 | .001 | 0.05 | 0.04 | .255 | 0.14 | 0.06 | .012 |
| Gender X Commercial Exposure | −0.17 | 0.07 | .011 | −0.04 | 0.05 | .446 | −0.22 | 0.07 | .003 |
Figure 1.
Visual Depiction of How Gender Moderates the Effect of E-cigarette Commercial Exposure on Product Use One Year Later among 1060 Alternative High School Students
Note.
Poisson regression models estimate a multiplicative effect characterized by a logarithmic curve.
Likeability of E-cigarette Commercials and Product Use One Year Later
Within the subsample of students who had seen at least one e-cigarette commercial, exposure to e-cigarette commercials was a statistically significant predictor of future use of e-cigarettes (b = 0.16, SE = 0.04, p <.001), cigarettes (b = 0.13, SE = 0.03, p <.001), and cigars (b = 0.09, SE = 0.04, p = .002) as Table 4 shows. Likeability also was a statistically significant predictor of increased use of e-cigarettes (b = 0.91, SE = 0.10, p < .001), cigarettes (b = 0.71, SE = 0.10, p < .001), and cigars (b = 0.80, SE = 0.10, p < .001). After adding multiple covariates to the models, exposure remained a significant predictor of increased use of e-cigarettes (b = 0.11, SE = 0.04, p = .004) and cigarettes (b = 0.10, SE = 0.04, p = .008), whereas likeability remained a statistically significant predictor of increased use of e-cigarettes (b = 0.44, SE = 0.12, p < .001), cigarettes (b = 0.23, SE = 0.10, p = .031), and cigars (b = 0.47, SE = 0.13, p < .001).
Table 4.
Multilevel Poisson Regression Models Examining the Relationship between E-cigarette Commercial Likeability and Product Use One Year Later among A Subsample of 720 Alternative High School Students Who Had Seen at Least One E-cigarette Commercial
| Variables | E-cigarettes | Cigarettes | Cigars | ||||||
|---|---|---|---|---|---|---|---|---|---|
| b | SE | p | b | SE | p | b | SE | p | |
| Unadjusted Models | |||||||||
| Exposure to E-cigarette Commercials | 0.16 | 0.04 | <.001 | 0.13 | 0.03 | <.001 | 0.09 | 0.04 | .019 |
| Likeability of E-Cigarette Commercials | 0.91 | 0.10 | <.001 | 0.71 | 0.10 | <.001 | 0.80 | 0.10 | <.001 |
| Covariate Adjusted Models | |||||||||
| Gender (Male) | 0.66 | 0.16 | <.001 | 0.26 | 0.12 | .023 | 0.48 | 0.15 | .002 |
| Ethnicity (Hispanic) | −0.40 | 0.16 | .013 | −0.40 | 0.13 | .002 | −0.48 | 0.16 | .003 |
| Age | 0.02 | 0.08 | .831 | 0.01 | 0.07 | .889 | −0.12 | 0.09 | .188 |
| Family Use of E-cigarettes | 0.13 | 0.17 | .447 | 0.22 | 0.14 | .113 | 0.13 | 0.18 | .473 |
| Family Use of Cigarettes | −0.20 | 0.17 | .262 | 0.31 | 0.13 | .015 | −0.03 | 0.18 | .871 |
| Family Use of Cigars | 0.27 | 0.22 | .210 | 0.02 | 0.17 | .920 | 0.35 | 0.21 | .100 |
| Peer Use of E-cigarettes | 0.09 | 0.26 | .722 | −0.05 | 0.18 | .793 | 0.19 | 0.22 | .379 |
| Peer Use of Cigarettes | 0.25 | 0.23 | .278 | 0.64 | 0.24 | .008 | −0.32 | 0.24 | .175 |
| Peer Use of Cigars | −0.21 | 0.17 | .203 | 0.14 | 0.15 | .339 | 0.44 | 0.17 | .011 |
| Previous Use of E-cigarettes | 0.15 | 0.02 | <.001 | 0.03 | 0.02 | .211 | −0.03 | 0.03 | .374 |
| Previous Use of Cigarettes | 0.08 | 0.03 | .010 | 0.21 | 0.02 | <.001 | 0.16 | 0.03 | <.001 |
| Previous Use of Cigars | −0.16 | 0.05 | .003 | −0.01 | 0.04 | .759 | 0.10 | 0.04 | .003 |
| Exposure to other Tobacco Advertising | 0.17 | 0.07 | .013 | 0.13 | 0.06 | .029 | 0.22 | 0.07 | .002 |
| Exposure to E-cigarette Commercials | 0.11 | 0.04 | .004 | 0.10 | 0.04 | .008 | 0.00 | 0.04 | .910 |
| Likeability of E-cigarette Commercials | 0.44 | 0.12 | <.001 | 0.23 | 0.10 | .031 | 0.47 | 0.13 | <.001 |
A one unit change in exposure to e-cigarette commercials was associated with an 11.6% increase in the number of times students used e-cigarettes and a 10.0% increase in the number of times students smoked cigarettes in the past 30 days. A one unit change in likeability was associated with a 56.0% increase in the number of times students used e-cigarettes, a 25.2% increase in the use of cigarettes, and a 60.7% increase in the use of cigars in the past 30 days. The interaction between ethnicity and the likeability of e-cigarette commercials was not statistically significant in models predicting the use of e-cigarettes (b = −0.08, SE = 0.23, p = .734), cigarettes (b = 0.08, SE = 0.21, p = .714), or cigars (b = 0.13, SE = 0.25, p = .594). Similarly, gender did not moderate the relationship between e-cigarette commercial likeability and the use of e-cigarettes (b = −0.25, SE = 0.27, p = .352), cigarettes (b = 0.13, SE = 0.21, p = .531), or cigars (b = −0.15, SE = 0.28, p = .592).
DISCUSSION
E-cigarette Commercials and the Use of Multiple Nicotine and Tobacco Products
We explored the relationship between e-cigarette commercials and the use of nicotine and tobacco products in high-risk youth in southern California. In the unadjusted models, exposure to e-cigarette commercials was associated with increased use of e-cigarettes, cigarettes, and cigars one year later. After adding covariates to the model, only the relationship between commercial exposure and the use of e-cigarettes remained statistically significant. However, a moderating effect also was detected, which indicated that the relationship between commercial exposure and the use of e-cigarettes and cigars was stronger among females. Within the subsample of students who had viewed at least one e-cigarette commercial, repeated exposure was associated with increased use of e-cigarettes and cigarettes in both the unadjusted and adjusted models. Moreover, the degree to which students liked the commercials predicted an increase in the use of e-cigarettes, cigarettes, and cigars one year later in models with and without covariates. Taken together, these findings suggest that e-cigarette commercials may play an important role in persuading high-risk youth to use nicotine and tobacco products. This interpretation aligns with prior research indicating that e-cigarette advertising increases susceptibility to smoking in youth41,42 and that likeable commercials influence youth behavior.52,53 The moderating effect of gender that we found and supported by other studies80–82 is particularly troubling given that females metabolize nicotine faster than males,83 which may make subsequent attempts at cessation more challenging.84–85
Although the use of traditional cigarettes among youth has declined, dual-use and poly-use have been rising since 2011.86 The timing is noteworthy given that whereas e-cigarettes were introduced to US consumers in 2006,87 advertising expenditures remained relatively low until 201188 after which they increased 10-fold.89 It was only after this increase that e-cigarette use among students who had not previously used tobacco products rose from approximately 79,000 in 2011 to more than 263,000 in 2013.90 Past research shows a dose-response relationship between exposure to pro-tobacco advertising channels and youth experimentation with alternative nicotine and tobacco products.91–93 The addition of a new product (e-cigarettes) promoted through a new medium (commercials) may be a key factor contributing to recent estimates indicating that over 1.6 million youth have used 2 or more nicotine and tobacco products in the past 30 days.31
Limitations
Conclusions derived from the current investigation must be weighed against threats to validity94 such as mono-method bias and maturation. Among smokers, self-report measures have been known to produce imprecise estimates of cigarette use.95–97 Recall bias may have similarly resulted in inaccurate reports of the use of cigarettes, e-cigarettes, and cigars in the past 30 days. Prior longitudinal investigations also have revealed that youth tobacco use progression is associated with increased receptivity to tobacco advertising98 as well as greater amounts of time spent watching television.99,100 Although randomized experiments29,30,101–103 suggest a causal mechanism in which e-cigarette advertising encourages youth to use nicotine and tobacco products, it also may be the case that reported increases in the use of e-cigarettes, cigarettes, and cigars are being driven by a natural progression in the use of addictive products and that the higher levels of e-cigarette commercial exposure and receptivity observed in the current investigation are incidental.
Another noteworthy limitation is that the sample was predominantly Hispanic and restricted to students attending alternative high schools in southern California, which limits the generalizability of the findings. Future research should test whether the reported effects can be replicated in national and international longitudinal datasets such as those provided through the Population Assessment of Tobacco and Health Study and the International Tobacco Control Policy Evaluation Project. It is also worth emphasizing that whereas the current investigation highlighted the importance of commercial likeability it did not delineate the types of content that youth find appealing. Focus groups have revealed the attractive qualities of novel tobacco products.104,105 Similar qualitative research should be conducted to determine the types of commercials youth classify as engaging.
Policy Implications
Despite the limitations, findings from the study suggest that policies should be developed to protect high-risk youth from the influence of e-cigarette commercials utilizing evidence-based106 frameworks such as the World Health Organization Framework Convention on Tobacco Control107–109 (WHO FCTC). A sensible approach described in Article 13 of the WHO FCTC would be to extend the Broadcast Advertising Ban to include a broader range of nicotine and tobacco products.110,111 Such policies have been shown to be effective at reducing smoking112,113 and have been implemented in multiple countries across the globe,114 including all nations within the European Union.115 Unfortunately, this form of government intervention is likely to be challenged on the grounds of free speech in the US.116,117 Consequently, policymakers may wish to support counteradvertising campaigns in accordance with Article 12 of the WHO FCTC. Numerous studies118–126 have demonstrated the efficacy of mass media interventions including those that specifically target adolescent females.127 In light of the moderating effect of gender that we detected, both prevention and cessation programs tailored toward young women may help reduce the use of nicotine and tobacco products among high-risk youth. It may also be prudent to require the Federal Trade Commission to track advertising expenditures for e-cigarettes given the known correlation between the launch of tobacco marketing campaigns and gender-specific increases in youth smoking.128,129
Article 6 of the WHO FCTC suggests that raising the price of nicotine and tobacco products through taxation may be an effective deterrent to youth smoking. This approach is strongly supported in California,130 has been implemented in multiple locations throughout the US,131 and is buttressed by prior research132–134 including a study indicating that Hispanics, females, and low-SES populations are especially responsive to increases in the price of tobacco products.135 Increasing the cost of cigars may be especially powerful given evidence indicating these are some of the cheapest tobacco products sold near alternative high schools,45 and that the sale of cigars may be escalating following the passage of the Family Smoking Prevention and Tobacco Control Act.136 An additional course of action recommended by Article 16 of the WHO FCTC and supported by extensive research137–140 is to increase the minimum age at which youth can purchase nicotine and tobacco products. Public support for these laws is broad141 and nearly half of the states and over 400 cities within the country have already raised the minimum age for tobacco purchases to 21.142 Applying the same restriction to e-cigarettes may be a politically feasible way to combat the current vaping epidemic.143
As policymakers consider these approaches, they also may find it necessary to reframe the conversation surrounding commercials for e-cigarettes. Although the debate about whether e-cigarettes represent a safer alternative to traditional cigarettes is warranted, it should not overshadow the discussion about whether advertising that could persuade youth to use hazardous products should be disseminated without limitations. Although society may benefit by encouraging existing smokers to switch to a less harmful alternative, such benefits must be balanced against the cost of permitting a new generation of youth to become addicted to nicotine and tobacco products.
Acknowledgements
The authors thank Sandy Asad, Sara J Asad, Melissa Garrido, Sarah Z Gonzalez, and Brenda Lisa Lucero for their tireless efforts recruiting and tracking alternative high school students. Additional thanks to Jerry Grenard for critical help refining the central concepts.
Conflict of Interest Disclosure Statement
Research reported in this publication was supported by the NICHD and FDA Center for Tobacco Products (R01HD077560). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the FDA. All authors declare no other conflicts of interest.
Footnotes
Human Subjects Statement
This study was approved by the Claremont Graduate University Institutional Review Board (IRB#: 2214).
Contributor Information
James Russell Pike, School of Community and Global Health, Claremont Graduate University, Claremont, CA..
Nasya Tan, School of Community and Global Health, Claremont Graduate University, Claremont, CA..
Stephen Miller, School of Community and Global Health, Claremont Graduate University, Claremont, CA..
Christopher Cappelli, Department of Preventive Medicine, Keck School of Medicine, University of Southern California, Los Angeles, CA..
Bin Xie, School of Community and Global Health, Claremont Graduate University, Claremont, CA..
Alan W Stacy, School of Community and Global Health, Claremont Graduate University, Claremont, CA..
References
- 1.Pollay R. Targeting tactics in selling smoke: youthful aspects of 20th century cigarette advertising. Journal of Marketing Theory and Practice. 1995;3:1–22. [Google Scholar]
- 2.US Department of Health, Education, and Welfare. Smoking and Health: Report of the Advisory Committee to the Surgeon General of the Public Health Service. Washington, DC: US Department of Health, Education, and Welfare; 1964. [Google Scholar]
- 3.Lewit EM, Coate D, Grossman M. The effect of government regulation on teenage smoking. J Law Econ. 1981;24:545–569. [Google Scholar]
- 4.Holak SL, Reddy SK. Effects of a television and radio advertising ban: a study of the cigarette industry. J Mark. 1986;50(4):219–227. [Google Scholar]
- 5.Hodge JG, Collmer V, Orenstein DG, et al. Reconsidering the legality of cigarette smoking advertisements on television public health and the law. J Law Med Ethics. 2013;41(1):369–373. [DOI] [PubMed] [Google Scholar]
- 6.Gray E. The Super Bowl ad you won’t see this year. Time Magazine. 2014. Available at: http://business.time.com/2014/01/23/the-superbowl-ad-you-wont-see-this-year/. Accessed July 6,2017. [Google Scholar]
- 7.Bullen C, McRobbie H, Thornley S, et al. Effect of an electronic nicotine delivery device (e cigarette) on desire to smoke and withdrawal, user preferences and nicotine delivery: randomised cross-over trial. Tob Control. 2010;19(2):98–103. [DOI] [PubMed] [Google Scholar]
- 8.McCauley L, Markin C, Hosmer D. An unexpected consequence of electronic cigarette use. Chest. 2012;141(4):1110–1113. [DOI] [PubMed] [Google Scholar]
- 9.Monroy AE, Hommel E, Smith ST, Raji M. Paroxysmal atrial fibrillation following electronic cigarette use in an elderly woman. Clin Geriatr Med. 2012;20(3):28–32. [Google Scholar]
- 10.Goniewicz ML, Knysak J, Gawron M, et al. Levels of selected carcinogens and toxicants in vapour from electronic cigarettes. Tob Control. 2014;23(2):133–139. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pisinger C, Dossing M. A systematic review of health effects of electronic cigarettes. Prev Med. 2014;69:248–260. [DOI] [PubMed] [Google Scholar]
- 12.Schripp T, Markewitz D, Uhde E, Salthammer T. Does e-cigarette consumption cause passive vaping? Indoor Air. 2013;23(1):25–31. [DOI] [PubMed] [Google Scholar]
- 13.Schober W, Szendrei K, Matzen W, et al. Use of electronic cigarettes (e-cigarettes) impairs indoor air quality and increases FeNO levels of e-cigarette consumers. Int J Hyg Environ Health. 2014;217(6):628–637. [DOI] [PubMed] [Google Scholar]
- 14.McAuley TR, Hopke PK, Zhao J, Babaian S. Comparison of the effects of e-cigarette vapor and cigarette smoke on indoor air quality. Inhal Toxicol. 2012;24(12):850–857. [DOI] [PubMed] [Google Scholar]
- 15.Glantz SA, Bareham DW. E-Cigarettes: use, effects on smoking, risks, and policy implications. Annu Rev Public Health. 2018;39:215–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Livingston CJ, Freeman RJ, Costales VC, et al. Electronic nicotine delivery systems or e-cigarettes: American College of Preventive Medicine’s practice statement. Am J Prev Med. 2019;56(1):167–178. [DOI] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services (USDHHS). E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: USDHHS, US Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 2016. [Google Scholar]
- 18.Abrams DB. Promise and peril of e-cigarettes: can disruptive technology make cigarettes obsolete? JAMA. 2014;311(2):135–136. [DOI] [PubMed] [Google Scholar]
- 19.Green SH, Bayer R, Fairchild AL. Evidence, policy, and e-cigarettes – will England reframe the debate? N Engl J Med. 2016;374(14):1301–1303. [DOI] [PubMed] [Google Scholar]
- 20.Hajek P, Etter JF, Benowitz N, et al. Electronic cigarettes: review of use, content, safety, effects on smokers and potential for harm and benefit. Addict. 2014;109(11):1801–1810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Niaura RS, Glynn TJ, Abrams DB. Youth experimentation with e-cigarettes: another interpretation of the data. JAMA. 2014;312(6):641–642. [DOI] [PubMed] [Google Scholar]
- 22.Schraufnagel DE. Electronic cigarettes: vulnerability of youth. Pediatr Allergy Immunol Pulmonol. 2015;28(1):2–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Soneji S, Barrington-Trimis JL, Wills TA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Levy D, Borland R, Lindblom EN, et al. Potential deaths averted in USA by replacing cigarettes with e-cigarettes. Tob Control. 2018;27(1):18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.McCarthy M. E-cigarette companies target youth, US congressional study finds. BMJ. 2014;348:g2871. [DOI] [PubMed] [Google Scholar]
- 26.Duke JC, Lee YO, Kim AE, et al. Exposure to electronic cigarette television advertisements among youth and young adults. Pediatrics. 2014;134(1):e29–36. [DOI] [PubMed] [Google Scholar]
- 27.Greenhill R, Dawkins L, Notley C, et al. Adolescent awareness and use of electronic cigarettes: a review of emerging trends and findings. J Adolesc Health. 2016;59(6):612–619. [DOI] [PubMed] [Google Scholar]
- 28.Duke JC, Allen JA, Eggers ME, et al. Exploring differences in youth perceptions of the effectiveness of electronic cigarette television advertisements. Nicotine Tob Res. 2016;18(5):1382–1386. [DOI] [PubMed] [Google Scholar]
- 29.Farrelly MC, Duke JC, Crankshaw EC, et al. A randomized trial of the effect of e-cigarette TV advertisements on intentions to use e-cigarettes. Am J Prev Med. 2015;49(5):686–693. [DOI] [PubMed] [Google Scholar]
- 30.Villanti AC, Rath JM, Williams VF, et al. Impact of exposure to electronic cigarette advertising on susceptibility and trial of electronic cigarettes and cigarettes in US young adults: a randomized controlled trial. Nicotine Tob Res. 2016;18(5):1331–1339. [DOI] [PubMed] [Google Scholar]
- 31.Gentzke A, Creamer M, Cullen K, et al. Vital signs: tobacco product use among middle and high school students - United States, 2011–2018. MMWR Morb Mortal Wkly Rep. 2019;68(6):157–164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lovato C, Watts A, Stead LF. Impact of tobacco advertising and promotion on increasing adolescent smoking behaviours. Cochrane Database Syst Rev. 2011;5(10):CD003439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Barnett E, Spruijt-Metz D, Unger JB, et al. Bidirectional associations between future time perspective and substance use among continuation high-school students. Subst Use Misuse. 2013;48(8):574–580. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Black DS, Sussman S, Unger J, et al. Gender differences in body consciousness and substance use among high-risk adolescents. Subst Use Misuse. 2010;45(10):1623–1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Johnson KE, McMorris BJ, Kubik MY. Comparison of health-risk behaviors among students attending alternative and traditional high schools in Minnesota. J Sch Nurs. 2013;29(5):343–352. [DOI] [PubMed] [Google Scholar]
- 36.Pokhrel P, Sussman S, Stacy AW. Relative effects of social self-control, sensation seeking, and impulsivity on future cigarette use in a sample of high-risk adolescents. Subst Use Misuse. 2014;49(4):343–351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sussman S, Rohrbach LA, Spruijt-Metz D, et al. One-year prediction of pain killer use among at-risk older teens and emerging adults. J Drug Educ. 2012;42(2):195–210. [DOI] [PubMed] [Google Scholar]
- 38.Zheng Y, Zhen C, Dench D, Nonnemaker JM. U.S. demand for tobacco products in a system framework. Health Econ. 2017;26(8):1067–1086. [DOI] [PubMed] [Google Scholar]
- 39.Zheng Y, Zhen C, Nonnemaker JM, Dench D. Advertising, habit formation, and U.S. tobacco product demand. Am J Agric Econ. 2016;98(4):1038–1054. [Google Scholar]
- 40.Camenga D, Gutierrez KM, Kong G, et al. E-cigarette advertising exposure in e-cigarette naïve adolescents and subsequent e-cigarette use: a longitudinal cohort study. Addict Behav. 2018;81:78–83. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pierce JP, Sargent JD, Portnoy DB, et al. Association between receptivity to tobacco advertising and progression to tobacco use in youth and young adults in the PATH study. JAMA Pediatr. 2018;172(5):444–451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pierce JP, Sargent JD, White MM, et al. Receptivity to tobacco advertising and susceptibility to tobacco products. Pediatrics. 2017;139(6):e20163353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Singh T, Agaku IT, Arrazola RA, et al. Exposure to advertisements and electronic cigarette use among US middle and high school students. Pediatrics. 2016;137(5):e20154155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.US Department of Health and Human Services. Preventing Tobacco Use Among Young People: A Report of the Surgeon General. Atlanta, GA: USDHHS, US Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; 1994. [Google Scholar]
- 45.Beleva Y, Pike JR, Miller S, et al. Share of advertising voice at the point-of-sale and its influence on at-risk students’ use of alternative tobacco products. Nicotine Tob Res. 2019;21(7):903–910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Miller S, Pike JR, Stacy AW, et al. Negative affect in at-risk youth: outcome expectancies mediate relations with both regular and electronic cigarette use. Psychol Addict Behav. 2017;31(4):457–464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Booker CL, Harding S, Benzeval M. A systematic review of the effect of retention methods in population-based cohort studies. BMC Public Health. 2011;11:249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hall EA, Zuniga R, Cartier J, et al. Staying in Touch: A Fieldwork Manual of Tracking Procedures for Locating Substance Abusers in Follow up Studies. Los Angeles, CA: UCLA Integrated; 2003. [Google Scholar]
- 49.McCuller WJ, Sussman S, Holiday K, et al. Tracking procedures for locating high-risk youth. Eval Health Prof. 2002;25(3):345–362. [DOI] [PubMed] [Google Scholar]
- 50.Scott CK. A replicable model for achieving over 90% follow-up rates in longitudinal studies of substance abusers. Drug Alcohol Depend. 2004;74(1):21–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Schooler C, Feighery E, Flora JA. Seventh graders’ self-reported exposure to cigarette marketing and its relationship to their smoking behavior. Am J Public Health. 1996;86(9):1216–1221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Stacy AW, Zogg JB, Unger JB, Dent CW. Exposure to televised alcohol ads and subsequent adolescent alcohol use. Am J Health Behav. 2004;28(6):498–509. [DOI] [PubMed] [Google Scholar]
- 53.Grenard JL, Dent CW, Stacy AW. Exposure to alcohol advertisements and teenage alcohol-related problems. Pediatrics. 2013;131(2):e369–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pokhrel P, Fagan P, Kehl L, Herzog TA. Receptivity to e-cigarette marketing, harm perceptions, and e-cigarette use. Am J Health Behav. 2015;39(1):121–131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Unger JB, Schuster D, Zogg J, et al. Alcohol advertising exposure and adolescent alcohol use: a comparison of exposure measures. Addict Res Theory. 2003;11(3):177–193. [Google Scholar]
- 56.Pokhrel P, Fagan P, Herzog TA, et al. Comparison of measures of e-cigarette advertising exposure and receptivity. Tob Regul Sci. 2017;3(4):424–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.US Centers for Disease Control and Prevention (CDC). 2011 Youth tobacco survey Smoking & Tobacco Use. Atlanta, GA; CDC; 2014. Available at: http://www.cdc.gov/tobacco/data_statistics/surveys/yts/index.htm. Accessed September 25, 2019. [Google Scholar]
- 58.Bricker JB, Peterson AV, Robyn Andersen M, et al. Close friends’, parents’, and older siblings’ smoking: reevaluating their influence on children’s smoking. Nicotine Tob Res. 2006;8(2):217–226. [DOI] [PubMed] [Google Scholar]
- 59.Chassin L, Presson C, Seo DC, et al. Multiple trajectories of cigarette smoking and the intergenerational transmission of smoking: a multigenerational, longitudinal study of a midwestern community sample. Health Psychol. 2008;27(6):819–828. [DOI] [PubMed] [Google Scholar]
- 60.Gilman SE, Rende R, Boergers J, et al. Parental smoking and adolescent smoking initiation: an intergenerational perspective on tobacco control. Pediatrics. 2009;123(2):e274–281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Leonardi-Bee J, Jere ML, Britton J. Exposure to parental and sibling smoking and the risk of smoking uptake in childhood and adolescence: a systematic review and meta-analysis. Thorax. 2011;66(10):847–855. [DOI] [PubMed] [Google Scholar]
- 62.Peterson AV, Leroux BG, Bricker J, et al. Nine-year prediction of adolescent smoking by number of smoking parents. Addict Behav. 2006;31(5):788–801. [DOI] [PubMed] [Google Scholar]
- 63.Ali MM, Dwyer DS. Estimating peer effects in adolescent smoking behavior: a longitudinal analysis. J Adolesc Health. 2009;45(4):402–408. [DOI] [PubMed] [Google Scholar]
- 64.Jackson C, Henriksen L, Dickinson D, et al. A longitudinal study predicting patterns of cigarette smoking in late childhood. Health Educ Behav. 1998;25(4):436–447. [DOI] [PubMed] [Google Scholar]
- 65.Scal P, Ireland M, Borowsky IW. Smoking among American adolescents: a risk and protective factor analysis. J Community Health. 2003;28(2):79–97. [DOI] [PubMed] [Google Scholar]
- 66.Tyas SL, Pederson LL. Psychosocial factors related to adolescent smoking: a critical review of the literature. Tob Control. 1998;7(4):409–420. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wang MQ. Social environmental influences on adolescents’ smoking progression. Am J Health Behav. 2001;25(4):418–425. [DOI] [PubMed] [Google Scholar]
- 68.California Department of Public Health. 2011–2012 California Student Tobacco Survey California Tobacco Control Program. Sacramento, CA: California Department of Public Health; 2014. Available at: http://www.cdph.ca.gov/programs/tobacco/Pages/default.aspx. Accessed January 21, 2014. [Google Scholar]
- 69.Graham J, Flay BR, Johnson CA, et al. Reliability of self-report measures of drug use in prevention research: evaluation of the Project SMART questionnaire via the test-re-test reliability matrix. J Drug Educ. 1984;14(2):175–193. [DOI] [PubMed] [Google Scholar]
- 70.Stacy AW, Flay BR, Sussman S, et al. Validity of alternative self-report indices of smoking among adolescents. Psychol Assess. 1990;2:442–446. [Google Scholar]
- 71.Ouellette JA, Wood W. Habit and intention in everyday life: the multiple processes by which past behavior predicts future behavior. Psychol Bull. 1998;124(1):54–74. [Google Scholar]
- 72.Fitzmaurice G, Laird N, Ware J. Applied Longitudinal Analysis. Hoboken, NJ: John Wiley & Sons Inc; 2004. [Google Scholar]
- 73.Gunsolley JC, Getchell C, Chinchilli VM. Small sample characteristics of generalized estimating equations. Commun Stat Simul Comput. 1995;24(4):869–878. [Google Scholar]
- 74.McNeish DM, Harring JR. Clustered data with small sample sizes: comparing the performance of model-based and design-based approaches. Commun Stat Simul Comput. 2017;46(2):855–869. [Google Scholar]
- 75.Pan W, Wall MM. Small-sample adjustments in using the sandwich variance estimator in generalized estimating equations. Stat Med. 2002;21(10):1429–1441. [DOI] [PubMed] [Google Scholar]
- 76.Berglund P, Heeringa S. Multiple Imputation of Missing Data Using SAS. Cary, NC: SAS Institute Inc; 2014. [Google Scholar]
- 77.Schabenberger O. Growing Up Fast: SAS 9.2 Enhancements to the GLIMMIX Procedure. Cary, NC: SAS Institute Inc; 2007. [Google Scholar]
- 78.Graham JW, Olchowski AE, Gilreath TD. How many imputations are really needed? Some practical clarifications of multiple imputation theory. Prev Sci. 2007;8(3):206–213. [DOI] [PubMed] [Google Scholar]
- 79.Zhu S-H, Cummins SE, Zhuang YL, et al. California Student Tobacco Survey 2015–16: Results of the Statewide Student Survey, Grades 8, 10, and 12. San Diego, CA: Center for Research and Intervention in Tobacco Control (CRITC), University of California, San Diego; 2017. [Google Scholar]
- 80.Brown Q, Milam AJ, Bowie JV, et al. The moderating role of gender in the relationship between tobacco outlet exposure and tobacco use among African American young adults. Prev Sci. 2016;17(3):338–346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Dirocco DN, Shadel WG. Gender differences in adolescents’ responses to themes of relaxation in cigarette advertising: relationship to intentions to smoke. Addict Behav. 2007;32(2):205–213. [DOI] [PubMed] [Google Scholar]
- 82.Mays D, Gilman SE, Rende R, et al. Influences of tobacco advertising exposure and conduct problems on smoking behaviors among adolescent males and females. Nicotine Tob Res. 2014;16(6):855–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Benowitz NL, Lessov-Schlaggar CN, Swan GE, Jacob P III. Female sex and oral contraceptive use accelerate nicotine metabolism. Clin Pharmacol Ther. 2006;79(5):480–488. [DOI] [PubMed] [Google Scholar]
- 84.Cepeda-Benito A, Reynoso JT, Erath S. Meta-analysis of the efficacy of nicotine replacement therapy for smoking cessation: differences between men and women. J Consult Clin Psychol. 2004;72(4):712–722. [DOI] [PubMed] [Google Scholar]
- 85.Piper ME, Cook JW, Schlam TR, et al. Gender, race, and education differences in abstinence rates among participants in two randomized smoking cessation trials. Nicotine Tob Res. 2010;12(6):647–657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.El-Toukhy S, Sabado M, Choi K. Trends in tobacco product use patterns among U.S. youth, 1999–2014. Nicotine Tob Res. 2019;20(6):690–697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Flahault A, Etter JF. Electronic cigarettes: it is urgent to promote them to save lives. Int J Public Health Res. 2014;59(5):681–682. [DOI] [PubMed] [Google Scholar]
- 88.Kim AE, Arnold KY, Makarenko O. E-cigarette advertising expenditures in the U.S., 2011–2012. Am J Prev Med. 2014;46(4):409–412. [DOI] [PubMed] [Google Scholar]
- 89.Kornfield R, Huang J, Vera L, Emery SL. Rapidly increasing promotional expenditures for e-cigarettes. Tob Control. 2015;24(2):110–111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Bunnell RE, Agaku IT, Arrazola R, et al. Intentions to smoke cigarettes among never-smoking US middle and high school electronic cigarette users: National Youth Tobacco Survey, 2011–2013. Nicotine Tob Res. 2015;17(2):228–235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Agaku IT, Ayo-Yusuf OA. The effect of exposure to pro-tobacco advertising on experimentation with emerging tobacco products among U.S. adolescents. Health Educ Behav. 2014;41(3):275–280. [DOI] [PubMed] [Google Scholar]
- 92.Amrock S, Zakhar J, Zhou S, Weitzman M. Perception of e-cigarette harm and its correlation with use among U.S. adolescents. Nicotine Tob Res. 2015;17(3):330–336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mantey DS, Cooper MR, Clendennen SL, et al. E-cigarette marketing exposure is associated with e-cigarette use among U.S. youth. J Adolesc Health. 2016;58(6):686–690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Shadish WR, Cook TD, Campbell DT. Experimental and Quasi-Experimental Designs for Generalized Causal Inference. Belmont, CA: Wadsworth Cengage Learning; 2002. [Google Scholar]
- 95.Shiffman S. How many cigarettes did you smoke? Assessing cigarette consumption by global report, Time-Line Follow-Back, and ecological momentary assessment. Health Psychol. 2009;28(5):519–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Stanton WR, McClelland M, Elwood C, et al. Prevalence, reliability and bias of adolescents’ reports of smoking and quitting. Addiction. 1996;91(11):1705–1714. [PubMed] [Google Scholar]
- 97.Wang H, Shiffman S, Griffith SD, Heitjan DF. Truth and memory: linking instantaneous and retrospective self-reported cigarette consumption. Ann Appl Stat. 2012;6(4):1689–1706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Audrain-McGovern J, Rodriguez D, Tercyak K, et al. Identifying and characterizing adolescent smoking trajectories. Cancer Epidemiol Biomarkers Prev. 2004;13(12):2023–2034. [PubMed] [Google Scholar]
- 99.Gidwani PP, Sobol A, DeJong W, et al. Television viewing and initiation of smoking among youth. Pediatrics. 2002;110(3):505–508. [DOI] [PubMed] [Google Scholar]
- 100.Soldz S, Cui X. Pathways through adolescent smoking: a 7-year longitudinal grouping analysis. Health Psychol. 2002;21(5):495–504. [PubMed] [Google Scholar]
- 101.Padon AA, Lochbuehler K, Maloney EK, Cappella JN. A randomized trial of the effect of youth appealing e-cigarette advertising on susceptibility to use e-cigarettes among youth. Nicotine Tob Res. 2018;20(8):954–961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Petrescu DC, Vasiljevic M, Pepper JK, et al. What is the impact of e-cigarette adverts on children’s perceptions of tobacco smoking? An experimental study. Tob Control. 2017;26:421–427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rath JM, Teplitskaya L, Williams VF, et al. Correlates of e-cigarette ad awareness and likeability in U.S. young adults. Tob Induc Dis. 2017;15:22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Byron MJ, Baig SA, Moracco KE, Brewer NT. Adolescents’ and adults’ perceptions of ‘natural’, ‘organic’ and ‘additive-free’ cigarettes, and the required disclaimers. Tob Control. 2016;25(5):517–520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Caraballo RS, Pederson L, Gupta N. New tobacco products: do smokers like them? Tob Control. 2006;15(1):39–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Hoffman SJ, Tan C. Overview of systematic reviews on the health-related effects of government tobacco control policies. BMC Public Health. 2015;15:744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.World Health Organization (WHO). WHO Framework Convention on Tobacco Control. Geneva, Switzerland: WHO; 2003. [Google Scholar]
- 108.World Health Organization (WHO). The WHO Framework Convention on Tobacco Control: An Overview. Geneva, Switzerland: WHO; 2018. Available at: https://www.who.int/fctc/WHO_FCTC_summary.pdf?ua=1. Accessed April 8, 2019. [Google Scholar]
- 109.World Health Organization (WHO). Global Accelerated Action for the Health of Adolescents (AA-HA!): Guidance to Support Country Implementation. Geneva, Switzerland: WHO; 2017. [Google Scholar]
- 110.Grana R, Benowitz N, Glantz SA. Background paper on e-cigarettes (electronic nicotine delivery systems) World Health Organization Report. Geneva, Switzerland: World Health Organization; 2013. [Google Scholar]
- 111.Grana R, Benowitz N, Glantz SA. E-cigarettes: a scientific review. Circulation. 2014;129(19):1972–1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Harris F, MacKintosh AM, Anderson S, et al. Effects of the 2003 advertising/promotion ban in the United Kingdom on awareness of tobacco marketing: findings from the International Tobacco Control (ITC) Four Country Survey. Tob Control. 2006;15(Suppl 3):iii26–iii33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Kasza KA, Hyland AJ, Brown A, et al. The effectiveness of tobacco marketing regulations on reducing smokers’ exposure to advertising and promotion: findings from the International Tobacco Control (ITC) Four Country Survey. Int J Environ Res Public Health. 2011;8(2):321–340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Kennedy RD, Awopegba A, De León E, Cohen JE. Global approaches to regulating electronic cigarettes. Tob Control. 2016;26(4):440–445. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Islami F, Stoklosa M, Drope J, Jemal A. Global and regional patterns of tobacco smoking and tobacco control policies. Eur Urol Focus. 2015;1(1):3–16. [DOI] [PubMed] [Google Scholar]
- 116.Gostin LO. Corporate speech and the Constitution: the deregulation of tobacco advertising. Am J Public Health. 2002;92(3):352–355. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Stoll E. The Family Smoking Prevention and Tobacco Control Act and the First Amendment: why a substantial interest in protecting public health won’t save some new restrictions on tobacco advertising. Food Drug Law J. 2010;65(4):873–900. [PubMed] [Google Scholar]
- 118.Carson KV, Ameer F, Sayehmiri K, et al. Mass media interventions for preventing smoking in young people. Cochrane Database Syst Rev. 2017;6:CD001006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Bauer UE, Johnson TM, Hopkins RS, et al. Changes in youth cigarette use and intentions following implementation of a tobacco control program: findings from the Florida Youth Tobacco Survey, 1998–2000. JAMA. 2000;284(6):723–728. [DOI] [PubMed] [Google Scholar]
- 120.Emery S, Wakefield MA, Terry-McElrath Y, et al. Televised state-sponsored antitobacco advertising and youth smoking beliefs and behavior in the United States, 1999–2000. Arch Pediatr Adolesc Med. 2005;159(7):639–645. [DOI] [PubMed] [Google Scholar]
- 121.Farrelly MC, Healton CG, Davis KC, et al. Getting to the truth: evaluating national tobacco countermarketing campaigns. Am J Public Health. 2002;92(6):901–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Farrelly MC, Davis KC, Haviland ML, et al. Evidence of a dose-response relationship between “truth” antismoking ads and youth smoking prevalence. Am J Public Health. 2005;95(3):425–431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Niederdeppe J, Farrelly MC, Haviland ML. Confirming “truth”: more evidence of a successful tobacco counter marketing campaign in Florida. Am J Public Health. 2004;94(2):255–257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Siegel M, Biener L. The impact of an antismoking media campaign on progression to established smoking: results of a longitudinal youth study. Am J Public Health. 2000;90(3):380–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Sly DF, Hopkins RS, Trapido E, Ray S. Influence of a counteradvertising media campaign on initiation of smoking: the Florida “truth” campaign. Am J Public Health. 2001;91(2):233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Terry-McElrath YM, Wakefield MA, Emery S, et al. State anti-tobacco advertising and smoking outcomes by gender and race/ethnicity. Ethn Health. 2007;12(4):339–362. [DOI] [PubMed] [Google Scholar]
- 127.Worden JK, Flynn BS, Solomon LJ, et al. Using mass media to prevent cigarette smoking among adolescent girls. Health Educ Q. 1996;23(4):453–468. [DOI] [PubMed] [Google Scholar]
- 128.Pierce JP, Lee L, Gilpin EA. Smoking initiation by adolescent girls, 1944 through 1988. An association with targeted advertising. JAMA. 1994;271(8):608–611. [PubMed] [Google Scholar]
- 129.Pierce JP, Gilpin EA. A historical analysis of tobacco marketing and the uptake of smoking by youth in the United States: 1890–1977. Health Psychol. 1995;14(6):500–508. [DOI] [PubMed] [Google Scholar]
- 130.Unger JB, Barker D, Baezconde-Garbanati L, et al. Support for electronic cigarette regulations among California voters. Tob Control. 2017;26(3):334–337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Tremblay MC, Pluye P, Gore G, et al. Regulation profiles of e-cigarettes in the United States: a critical review with qualitative synthesis. BMC Med. 2015;13:130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Chaloupka FJ, Straif K, Leon ME. Working Group, International Agency for Research on Cancer. Effectiveness of tax and price policies in tobacco control. Tob Control. 2011;20(3):235–238. [DOI] [PubMed] [Google Scholar]
- 133.Chaloupka FJ, Yurekli A, Fong GT. Tobacco taxes as a tobacco control strategy. Tob Control. 2012;21(2):172–180. [DOI] [PubMed] [Google Scholar]
- 134.Golden SD, Ribisl KM, Perreira KM. Economic and political influence on tobacco tax rates: a nationwide analysis of 31 years of state data. Am J Public Health. 2013;104(2):350–357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Tauras JA, Huang J, Chaloupka FJ. Differential impact of tobacco control policies on youth sub-populations. Int J Environ Res Public Health. 2013;10(9):4306–4322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Delnevo C, Giovenco D, Miller Lo E. Changes in the mass-merchandise cigar market since the Tobacco Control Act. Tob Regul Sci. 2017;3(2 Suppl 1):S8–S16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.DiFranza JR, Carlson RP, Caisse RE. Reducing youth access to tobacco. Tob Control. 1992;1(1):58. [Google Scholar]
- 138.Levinson AH, Mickiewicz T. Reducing underage cigarette sales in an isolated community: the effect on adolescent cigarette supplies. Prev Med. 2007;45(6):447–453. [DOI] [PubMed] [Google Scholar]
- 139.Tutt D, Bauer L, Difranza J. Restricting the retail supply of tobacco to minors. J Public Health Policy. 2009;30(1):68–82. [DOI] [PubMed] [Google Scholar]
- 140.Verdonk-Kleinjan WM, Knibbe RA, Bieleman B, et al. The tobacco sales ban and tobacco purchases by adolescents: a general population study in The Netherlands. Eur J Public Health. 2008;18(5):498–503. [DOI] [PubMed] [Google Scholar]
- 141.Lee JG, Boynton MH, Richardson A, et al. Raising the legal age of tobacco sales: policy support and trust in government, 2014–2015, U.S. Am J Prev Med. 2016;51(6):910–915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Jenssen BP, Boykan R. Electronic cigarettes and youth in the United States: a call to action (at the local, national and global levels). Children (Basel). 2019;6(2):30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Chadi N, Hadland SE, Harris SK. Understanding the implications of the “vaping epidemic” among adolescents and young adults: a call for action. Subst Abus. 2019;40(1):7–10. [DOI] [PMC free article] [PubMed] [Google Scholar]