Abstract
Aims
To describe aetiologies and temporal trends in young patients with atrioventricular block (AVB).
Methods and results
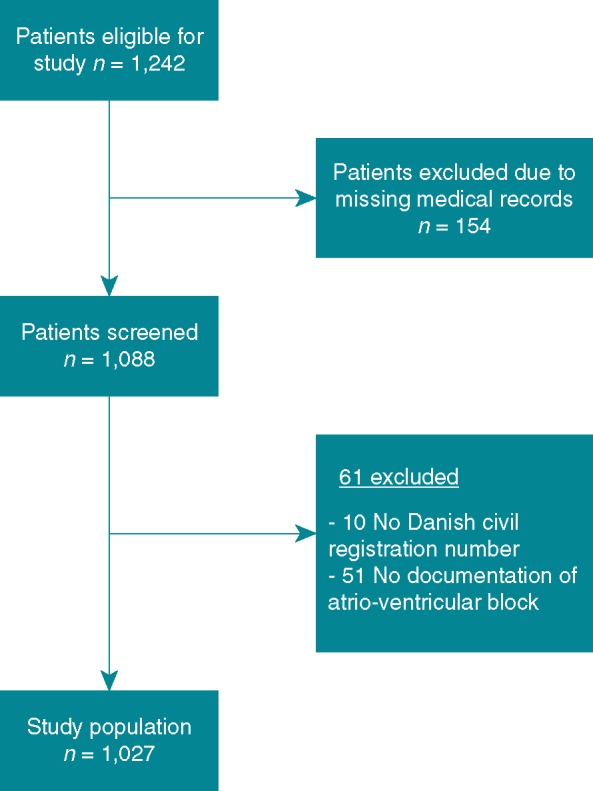
We identified all patients in Denmark, receiving their first pacemaker because of AVB before the age of 50 years between 1996 and 2015. Medical records were reviewed and clinical information and diagnostic work-up results were obtained to evaluate the aetiology. We used Poisson regression testing for temporal trends. One thousand and twenty-seven patients were identified, median age at time of implantation was 38 (interquartile range 25–45) years, 584 (56.9%) were male. The aetiologies were complications to cardiac surgery [n = 157 (15.3%)], congenital AVB [n = 93 (9.0%)], cardioinhibitory reflex [n = 52 (5.0%)], congenital heart disease [n = 43 (4.2%)], complication to radiofrequency ablation [n = 35 (3.4%)], cardiomyopathy [n = 31 (3.0%)], endocarditis [n = 18 (1.7%)], muscular dystrophy [n = 14 (1.4%)], ischaemic heart disease [n = 14 (1.4%)], sarcoidosis [n = 11 (1.1%)], borreliosis [n = 9 (0.9%)], hereditary [n = 6 (0.6%)], side-effect to antiarrhythmics [n = 6 (0.6%)], planned His-ablation [n = 5 (0.5%)], complication to alcohol septal ablation [n = 5 (0.5%)], and other known aetiologies [n = 11 (1.1%)]. The aetiology remained unknown in 517 (50.3%) cases. While the number of patients with unknown aetiology increased during the study period (P < 0.001), we observed no significant change in the number of patients with identified aetiology (P = 0.35).
Conclusion
In a nationwide cohort, the aetiology of AVB was identified in only half the patients younger than 50 years referred for first-time pacemaker implantation. The number of patients with unknown aetiology increased during the study period. These findings indicate need for better insight into aetiologies of AVB and improved diagnostic work-up guidelines.
Keywords: Atrioventricular block, Pacemaker, Aetiology, Temporal trends, Surgical complication, Congenital heart block
What’s new?
Aetiology of atrioventricular block (AVB) was identified in only half the patients younger than 50 years referred for first-time pacemaker implantation.
There has been a temporal increase in the number of patients younger than 50 years receiving their first pacemaker because of AVB.
While the number of patients with AVB of unknown aetiology increased during the study period, we observed no significant change in number of patients with identified aetiology.
Introduction
Atrioventricular block (AVB) is the most common indication for pacemaker implantation, constituting around half of all first-time pacemaker implantations in Denmark.1
The incidence of AVB increases with age, with idiopathic and age-related fibrosis of the cardiac conduction system (Lenegres disease) considered to be the most common aetiology.2,3 In general, patients with AVB has a good prognosis after pacemaker implantation,4 but in some cases, underlying disease determines a more malignant prognosis.5–9 In younger patients, underlying cardiac disease other than idiopathic fibrosis may cause AVB, but the knowledge about their prevalence is scarce. Previous studies have shown, that underlying cardiac diseases is underdiagnosed, potentially leaving some of these patients with a higher risk of heart failure, tachyarrhythmia, or sudden cardiac death.10–12
In this study, we aimed to describe the aetiologies of AVB identified by former and current diagnostic work-up in patients receiving their first pacemaker before the age of 50 years in a two-decade Danish nationwide population-based cohort. We hypothesized that in a large proportion of patients, the aetiology of AVB was not identified prior to implantation despite their young age.
Methods
Study population
To study aetiologies of AVB in a younger patient population, an age cut-off of 50 years was chosen. Between 1 January 1996 and 31 December 2015 all patients receiving their first pacemaker because of AVB before the age of 50 years in Denmark were included. Patients were identified from the Danish Pacemaker and ICD Registry.1 The register was founded in 1982, and all pacemaker implantations in Denmark have been reported to the registry since then. Upon birth or immigration, all Danish citizens are given a unique and permanent civil registration number. This allowed us to use the civil registration numbers from the Danish Pacemaker and ICD Registry to identify individual patient medical records.13
The study complies with the Declaration of Helsinki and was approved by the Danish Patient Safety Authority (record number: 3-3013-1970/1/) and the Danish Data Protection Agency (record number: 1-16-02-440-16).
Reviewing process
An in-depth review of the medical records and results from diagnostic work-up was performed retrospectively to evaluate the symptoms and the aetiologies of AVB as well as comorbidities. Patients were excluded if it was not possible to find the medical records.
In Denmark, the indication for pacemaker implantation follows the ESC guidelines on cardiac pacing.14 The indication for implantation was registered as either: (i) symptomatic 1st-degree AVB or symptomatic Mobitz Type I AVB. (ii) Mobitz Type II AVB or advanced 2nd-degree AVB. (iii) Third-degree AVB. For all patients included, documentation for the AVB was identified by electrocardiogram (ECG), telemetric recording, Holter-monitoring, loop-recording, or a description of the AVB, based on one of those modalities, written in the medical record. To ensure a consistent review, all medical records were reviewed by the same physician (J.R.R., overseen by H.K.J.) and categorization of aetiologies was defined before reviewing patient data. Congenital heart disease was considered the aetiology of AVB in cases with congenital corrected transposition, ventricular septal defect, Steno-Fallot tetralogy, or univentricular heart anatomy.15,16 The aetiology was registered as congenital AVB, borreliosis, or side-effect to needed medical treatment if this was reported as the aetiology in the medical records. In cases where the patient was known to have cardiomyopathy,17 cardiac sarcoidosis,11 or muscular dystrophy,18 this was considered the aetiology of AVB. The aetiology was registered as hereditary if a known pathogenic genetic mutation associated with AVB was identified. Ischaemic heart disease was considered the aetiology in cases where the patient developed AVB in relation to acute myocardial infarction. A tilt-table test with documented AVB was recorded as cardioinhibitory reflex aetiology. If planned His-ablation was performed, this was registered as the aetiology. AVB was considered a complication to cardiac surgery, alcohol septal ablation, or radiofrequency ablation if the patient had sinus rhythm prior to the procedure and AVB within 2 weeks after regardless of the indication for the procedure. Endocarditis was registered as the aetiology only if the atrioventricular conduction was affected in any way prior to surgery.
Statistical analysis
Continuous variables are expressed as median (interquartile range) and dichotomous variables as numbers (proportions). Comparisons were done using the χ2 test or the Mann–Whitney U test. Poisson regression was used to test for temporal trends. For the analyses of temporal trends, we adjusted for the number of inhabitants <50 years in Denmark each year. We did not test for temporal trends if there were <30 events throughout the study period. A P-value <0.05 was considered statistically significant. Statistical analyses were performed using STATA version 15.1.
Results
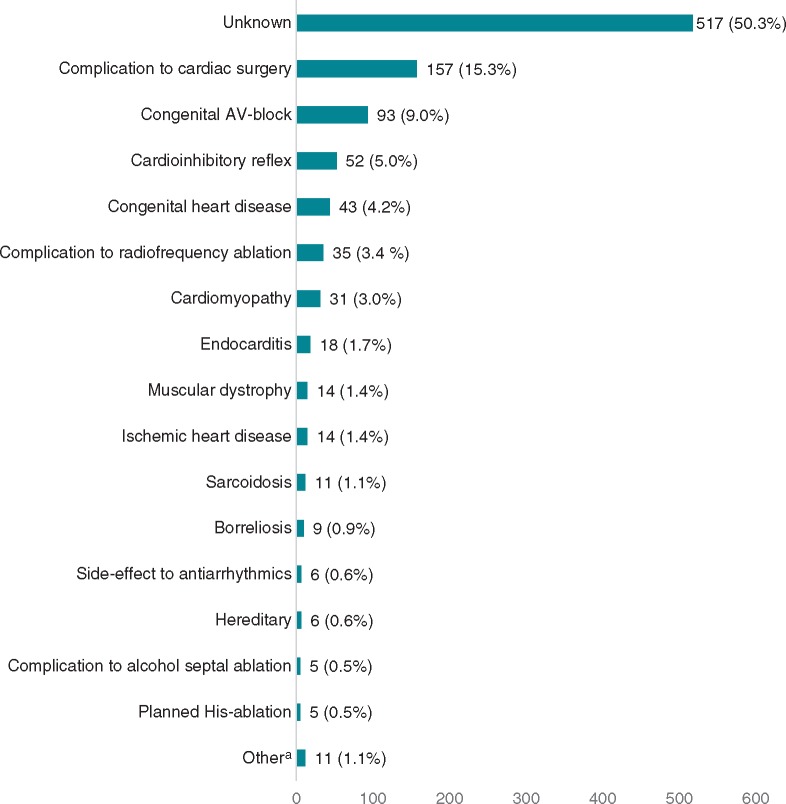
We identified 1242 patients from the Danish Pacemaker and ICD Registry receiving their first pacemaker due to AVB before 50 years of age. This equals an average incidence of 17.7 per year per one million inhabitants <50 years throughout the study period. After exclusion of 215 patients, we included 1027 patients in the study (Figure 1). The age- and sex distributions of the patients excluded due to missing medical records were similar to those of the included patients. Median age at first pacemaker implantation was 38 years (interquartile range 25–45) and 584 (56.9%) were males (Table 1). The aetiology of AVB was identified in 510 (49.7%) patients. Patients with AVB of known aetiology were significantly younger than patients with unknown aetiology at the time of pacemaker implantation (P < 0.001) and more often they were asymptomatic (P < 0.001). A high number of asymptomatic patients were seen among patients with complications to cardiac surgery [130 of 157 (82.8%)], congenital AVB [44 of 93 (47.3%)] and complications to radiofrequency ablation [20 of 35 (57.1%)]. Moreover, atrial fibrillation or flutter (P = 0.002) and heart failure (P < 0.001) were more common among patients with known aetiology.
Figure 1.
Flowchart for inclusion of patients with atrioventricular block treated with pacemaker implantation before the age of 50 years.
Table 1.
Characteristics of younger patients with AVB at time of first-pacemaker implantation
| Total (n = 1027) | Known (n = 510) | Unknown (n = 517) | P-value | |
|---|---|---|---|---|
| Age at implant | 38 (25–45) | 33 (14–44) | 41 (32–46) | <0.001 |
| Male sex | 584 (56.9%) | 285 (55.9%) | 299 (57.8%) | 0.528 |
| Mobitz I or 1st-degree AVB | 29 (2.8%) | 10 (2.0%) | 19 (3.7) | 0.097 |
| Mobitz II or advanced AVB | 193 (18.8%) | 50 (9.8%) | 143 (27.7%) | <0.001 |
| Third-degree AVB | 805 (78.4%) | 450 (88.2%) | 355 (68.7%) | <0.001 |
| Persistent AVB | 370 (36.0%) | 291 (57.1%) | 79 (15.3%) | <0.001 |
| Symptoms | ||||
| Dizziness | 352 (34.3%) | 95 (18.6%) | 257 (49.7%) | <0.001 |
| Syncope | 337 (32.8%) | 93 (18.2%) | 244 (47.2%) | <0.001 |
| Dyspnoea | 199 (19.4%) | 91 (17.8%) | 108 (20.9%) | 0.217 |
| Malaise | 157 (15.3%) | 60 (11.8%) | 97 (18.8%) | 0.002 |
| Chest pain | 109 (10.6%) | 40 (3.9%) | 69 (13.3%) | 0.004 |
| Fatigue | 106 (10.3%) | 49 (4.8%) | 57 (11.0%) | 0.455 |
| Cardiac arrest | 14 (1.4%) | 9 (0.9%) | 5 (1.0%) | 0.270 |
| Asymptomatic | 284 (27.7%) | 239 (46.9%) | 45 (8.7%) | <0.001 |
| Comorbidity | ||||
| Atrial fibrillation/flutter | 64 (6.2%) | 44 (8.6%) | 20 (3.9%) | 0.002 |
| Hypertension | 59 (5.7%) | 22 (4.3%) | 37 (7.2%) | 0.050 |
| Heart failure | 32 (3.1%) | 28 (5.5%) | 4 (0.8%) | <0.001 |
| Hypercholesterolaemia | 39 (3.8%) | 18 (3.5%) | 21 (4.1%) | 0.655 |
| Diabetes | 25 (2.4%) | 14 (2.7%) | 11 (2.1%) | 0.521 |
| Ischaemic heart disease | 24 (2.3%) | 13 (2.5%) | 11 (2.1%) | 0.655 |
| Sarcoidosis | 11 (1.1%) | 11 (2.2%) | 0 (0%) | 0.001 |
| Connective tissue disease | 16 (1.6%) | 5 (1.0%) | 11 (2.1%) | 0.138 |
AVB, atrioventricular block.
Aetiology of atrioventricular block
The aetiologies of AVB are shown in Figure 2. The most common were complications to cardiac surgery [n = 157 (15.3%)], congenital AVB [n = 93 (9.1%)] and cardioinhibitory reflex [n = 52 (5.1%)]. In 517 (50.3%) cases, no aetiology of AVB was identified. Results for men and women separately are reported in Supplementary material online, Tables S1A and B.
Figure 2.
Identified aetiologies of AV block in patients <50 years (n = 1027). aAmyloidosis (n = 2), myocarditis (n = 2), severe right ventricular dilation (n = 2), cardiac tumour (n = 1), Kearn–Sayre syndrome (n = 1), rheumatic fever (n = 1), side-effect to radiation therapy (n = 1), and graft vs. host reaction (n = 1). AV, atrioventricular.
Age distribution
The age distribution of the study population is shown in Figure 3. We observed a relatively high number of implants in children up to 4 years of age. The number of implants was lower among children aged 5–14 years, while from the age of 15 years, we observed an increasing number of implants with increasing age. In small children (0–5 years), an aetiology was identified in the vast majority of patients (94%), mainly complications to cardiac surgery or congenital AVB. Conversely, in middle-aged patients (44–49 years) aetiology was identified in less than half the patients (40.8%).
Figure 3.
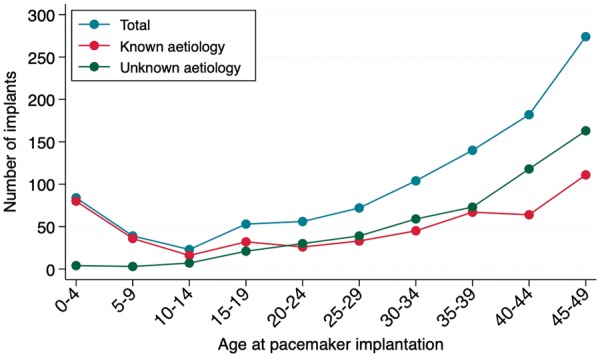
Total number of first-time pacemaker implantations in the period from 1 January 1996 and 31 December 2015 in patients <50 years with atrioventricular block divided into age groups of 5-year intervals.
Temporal development
During the study period, an overall temporal increase in the number of patients receiving a pacemaker was observed (P < 0.001). We tested for temporal trends also including the patients excluded due to missing medical records and still the temporal increase in the number of implants during the study period remained (P < 0.001). A temporal increase among patients without an identified aetiology of AVB was observed (P < 0.001), while there was no significant change in number of patients with an identified aetiology (P = 0.35) (Figure 4).
Figure 4.
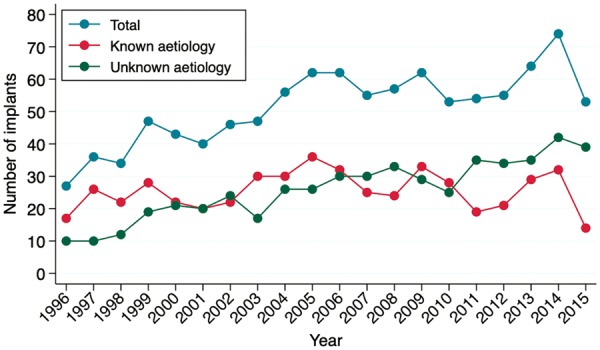
Number of first-time pacemaker implantations in younger patients with atrioventricular block per year from 1 January 1996 and 31 December 2015.
We observed no significant temporal changes in the type of AVB leading to pacemaker implantation among patients with AVB of known or unknown aetiology when corrected for the development in the number of implants in the respective groups (Figure 5).
Figure 5.
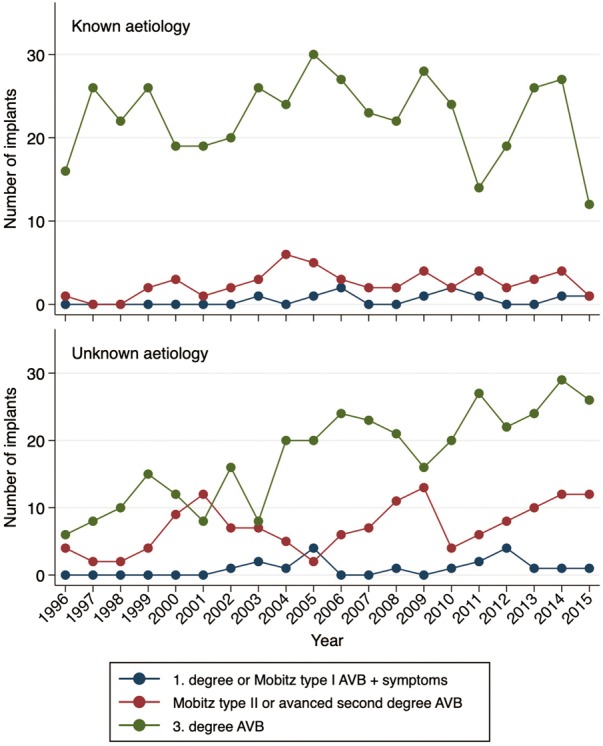
Indications of first-time pacemaker implantation in younger patients with atrioventricular block (AVB) of known and unknown aetiology in the period from 1 January 1996 and 31 December 2015.
When the aetiologies of AVB were tested for temporal trends one by one, we found a significant drop in the number of patients with congenital AVB (P = 0.049), and a significant increase in the number patients in whom cardioinhibitory reflex was the aetiology (P < 0.001). No significant temporal changes in the remaining aetiologies were observed (Supplementary material online, Table S2).
Discussion
In the present two-decade study, we investigated the aetiologies of AVB in a complete consecutive nationwide cohort of young patients with AVB. The main finding was that the aetiology of AVB was only identified in approximately half the patients, in whom complications to cardiac surgery or congenital AVB were the dominating aetiologies. In the remaining half, the aetiology of AVB remained unknown. Though access to advanced cardiac imaging techniques and molecular-genetic testing has evolved during the study period, the number of patients receiving a pacemaker on the basis of a known aetiology remained stable, while the number of patients with unknown aetiology rose throughout the study period. This finding could be triggered by increased use of Holter-monitoring and loop-recorders, and perhaps more persistency in the search of arrhythmias in recent years. Although an increasing number of patients receive a pacemaker, higher awareness of long-term complications in device treatment has appeared. Therefore, it cannot be ruled out that some patients treated with pacemaker in 1996 would not receive a permanently implanted device in 2015.
A large majority of patients with unknown aetiology had intermittent AVB. It cannot be ruled out that a considerable proportion hereof may suffer from idiopathic paroxysmal AVB, characterized by absence of structural heart disease, paroxysmal 3rd-degree AVB and normal resting ECG in-between AVB episodes.19
The use of advanced cardiac imaging methods in the diagnostic work-up of younger patients with AVB has previously been studied. In a study of North American patients aged 18–60 years, patients with AVB of unknown aetiology underwent fluorodeoxyglucose–positron emission tomography, resulting in a diagnosis of sarcoidosis in 34% of patients.11 In our study, only one percent of patients were found to have AVB due to sarcoidosis. Given the fact that northern Europe has one of the highest incidences of sarcoidosis in the world, cardiac sarcoidosis may be underdiagnosed in young patients with AVB.20 However, this needs to be tested in prospective studies.
We found that patients with known aetiology more often were asymptomatic compared to patients with unknown aetiology. The reason for this may be that more patients with known aetiology suffer from conditions requiring healthcare system attention. In these patients, there is a higher probability of discovering AVB before symptoms appear. Furthermore, when AVB is complicating an ablation procedure or surgery, a temporary pacemaker is placed upfront, shielding the patient from symptomatic bradyarrhythmia. In addition, many patients with congenital AVB are asymptomatic. In contrast, a healthy person younger than 50 years does not seek the healthcare system before symptoms appear. This may add to explain our findings. Still, the main cause of implantation in both patients with known and unknown aetiology was Mobitz II, advanced AVB or 3rd-degree AVB.
Cardiovascular comorbidities were more common among patients with AVB of known aetiology. Though, a smaller percentage of patients with AVB of unknown aetiology were also affected. These were still classified as having AVB of unknown aetiology because a causal link between atrial fibrillation/flutter, hypertension or heart failure, and AVB has not been shown. Regarding ischaemic heart disease, we defined this as aetiology only if AVB occurred in relation to acute myocardial infarction, not if the patient had atherosclerosis without myocardial infarction. Therefore, it cannot be ruled out that these comorbidities contributed to some degree to AVB in some patients with AVB of unknown aetiology.
The proportion of patients with congenital AVB in our study was similar to findings by others.8 It should be noted that we reported the number of patients receiving a pacemaker and that there was a shift in the late 90s from an expecting approach, where implantation was done only in symptomatic patients, to a more progressive approach with early, pre-symptomatic pacemaker implantation.21 Therefore, there might have been a catch-up in our study period which may be the reason for an upper range frequency of 1/13 700 in our study compared to 1/15 000–22 000 in earlier studies.8 Also, it cannot be ruled out that the temporal drop observed in patients with congenital AVB might be a product of a catch-up early in the follow-up period.
In our cohort, myocarditis was identified as the aetiology in only two patients. In the Global Burden of Disease Study 2013, the estimated annual incidence of myocarditis was 22/100 000 persons.22 In Denmark, this might represent 1250 annual cases. A previous study showed that 1.1% of patients with myocarditis develop high degree AVB, and hereof, one-fifth ended up receiving a permanent pacemaker.23 Applying these data to our cohort, this could represent around 50 patients during the 20-year study period. Thus, we cannot exclude under-diagnosis of myocarditis during this study period. Myocarditis might be one of the explanations underlying ABV of unknown aetiology in some patients.
Atrioventricular block based on cardioinhibitory reflex accounted for 5.1% of cases in our study.24 This is accordant with the current guidelines, that pacemaker implantation should be avoided in young patients on the indication of cardioinhibitory reflex syncope.25 It cannot be ruled out that the increased implantation activity on this indication over the study period was caused by higher attention to this disease entity.
Mutations in the LMNA and SCN5A genes are among the known hereditary causes of AVB. In our study, a hereditary aetiology was diagnosed in 0.6% of cases. It should be noted, that molecular-genetic testing was not nationwide implemented in Denmark before 2006. Furthermore, awareness of genetic mutations leading to AVB was not implemented in national guidelines before 2013. Therefore, the true prevalence of hereditary aetiologies is probably not reflected in this study. With increased use of molecular-genetic testing, the number of patients diagnosed with a hereditary aetiology is likely to increase in the future.
The identified aetiologies of AVB are diverse. Ranging from infectious disease to primary myocardial diseases, iatrogenic causes and autoimmune diseases, the diagnostic work-up has to be thorough to identify the aetiology. Particularly, since the aetiology may have decisive impact on treatment, e.g. antibiotics for borreliosis to avoid permanent pacemaker implantation and primary implantable cardioverter-defibrillator implantation rather than pacemaker in patients with sarcoidosis or pathogenic mutations implying increased risk of ventricular tachyarrhythmia and sudden cardiac death. Although knowledge about the aetiology may influence the choice of device in some patients, current guidelines have little focus on determining the aetiology of AVB in the diagnostic work-up. Given the large proportion of young patients with AVB without identified aetiology, it could be considered that such patients undergo standard screening upon time of implantation. We propose that such programme may comprise a thorough medical history with family history, laboratory screening including borreliosis serology and markers of sarcoidosis as well as echocardiography and cardiac MRI. Tilt-table-test should be performed if cardioinhibitory reflex is suspected and molecular-genetic testing may be reasonable in selected individuals as those with a family history of inherited heart disease or sudden cardiac death (Table 2). However, the diagnostic yield of such a programme is unknown and must be followed prospectively.
Table 2.
Suggested diagnostic work-up for younger patients with atrioventricular block at time of first-pacemaker implantation
| Routine work-up: recommended for all patients | |
|---|---|
| Diagnostics | Aetiology potentially covered |
| Medical history | Iatrogenica |
| Congenital AV block | |
| Congenital heart disease | |
| Cardiomyopathy | |
| Muscular dystrophy | |
| Ischaemic heart disease | |
| Sarcoidosis | |
| Borreliosis | |
| Myocarditis | |
| Amyloidosis | |
| Kearn–Sayre syndrome | |
| Echocardiography | Congenital heart disease |
| Cardiomyopathy | |
| Endocarditis | |
| Amyloidosis | |
| Cardiac tumour | |
| Laboratory testing | Congenital AV block |
| Borreliosis | |
| Myocarditis | |
| Cardiac magnetic resonance imaging | Congenital heart disease |
| Cardiomyopathy | |
| Sarcoidosis | |
| Myocarditis | |
| Amyloidosis | |
| Cardiac tumour | |
| Additional work-up: recommended on suspicion | |
|
| |
| Diagnostics | Aetiology potentially covered |
|
| |
| Tilt-table test | Cardioinhibitory reflex |
| Molecular genetic testing | Muscular dystrophy |
| Hereditary causes | |
AV, atrioventricular.
Complications to cardiac surgery, radiofrequency ablation or alcohol septal ablation, planned His-ablation, side-effect to antiarrhythmics or radiation therapy.
Strengths and limitations
A major strength of the study was access to all consecutive young patients receiving a pacemaker in Denmark. Hereby, were able to provide a complete overview of the aetiologies of AVB over a period of 20 years. Furthermore, all medical records were reviewed by the same physician, which ensured a uniform evaluation. To our knowledge, this is the first study to present a complete overview of AVB aetiologies on a nationwide scale. However, the study has limitations.
The study was performed retrospectively, with all the limitations inherited in this study design. Most importantly, diagnostic work-up was not protocolled to encompass any collection of specific diagnostics, and therefore, differed between patients. It is unknown whether an aetiology could have been identified in a larger proportion of patients, had all patients undergone the same well-defined series of diagnostic tests. Another limitation, also resulting from the study design, was the exclusion of 12% of patients due to medical records not available. However, the age- and sex distribution of the patients excluded were similar to that of the patients included.
Conclusion
In a nationwide cohort, the aetiology of AVB was identified in only half the patients younger than 50 years referred for first-time pacemaker implantation, and the number of patients with unknown aetiology increased during the study period. These findings indicate need for better insight into the aetiologies of AVB and improved diagnostic work-up guidelines.
Supplementary Material
Acknowledgements
We thank our colleagues Michael Skov Hansen, Aabenraa Regional Hospital; Sam Riahi Aalborg University Hospital; Søren Højberg, Bispebjerg Regional Hospital; Kristian Korsgaard Thomsen, Esbjerg Regional Hospital; Jim Hansen, Gentofte University Hospital; Troels Niemann, Herning Regional Hospital; Michael Dilou Jacobsen, Hillerød Regional Hospital; Gunnar Vagn Hagemann Jensen, Roskilde University Hospital; Anne Sejr Knudsen, Vejle Regional Hospital; and Jens Refsgaard, Viborg Regional Hospital for providing access to medical records.
Funding
This work was supported by unrestricted research grants from Skibsreder Per Henriksen, R. og hustrus Foundation, Danish Heart Foundation [16-R107-A6707-22988], the A. P. Møller Foundation for the Advancement of Medical Science, and the Novo Nordisk Foundation [NNF18OC0031258 to H.K.J].
Conflict of interest: J.C.N. is supported by an unrestricted grant from the Novo Nordisk Foundation, Denmark (NNF16OC0018658) and received an institutional grant from Abbott, United States. H.K.J. is supported by an unrestricted grant from the Novo Nordisk Foundation, Denmark (NNF18OC0031258) and received lecture fees from Abbott, United States and Biosense Webster, United States. All other authors have no conflict of interest to declare.
References
- 1.Danish Pacemaker and ICD Register. Danish Pacemaker and ICD Register Annual report 2015. https://ssl.icddata.dk/download/Danish_Pacemaker_and_ICD_Register_Annual_Report_2015b.pdf (21 January 2019, date last accessed).
- 2. Zoob M, Smith KS.. The aetiology of complete heart-block. Br Med J 1963;2:1149–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lenegre J. Etiology and pathology of bilateral bundle branch block in relation to complete heart block. Prog Cardiovasc Dis 1964;6:409–44. [DOI] [PubMed] [Google Scholar]
- 4. Udo EO, van Hemel NM, Zuithoff NP, Doevendans PA, Moons KG.. Prognosis of the bradycardia pacemaker recipient assessed at first implantation: a nationwide cohort study. Heart 2013;99:1573–8. [DOI] [PubMed] [Google Scholar]
- 5. van Rijsingen IA, Arbustini E, Elliott PM, Mogensen J, Hermans-van Ast JF, van der Kooi AJ. et al. Risk factors for malignant ventricular arrhythmias in lamin A/C mutation carriers: a European Cohort Study. J Am Coll Cardiol 2012;59:493–500. [DOI] [PubMed] [Google Scholar]
- 6. Anselme F, Moubarak G, Savoure A, Godin B, Borz B, Drouin-Garraud V. et al. Implantable cardioverter-defibrillators in lamin A/C mutation carriers with cardiac conduction disorders. Heart Rhythm 2013;10:1492–8. [DOI] [PubMed] [Google Scholar]
- 7. Kumar S, Baldinger SH, Gandjbakhch E, Maury P, Sellal JM, Androulakis AF. et al. Long-term arrhythmic and nonarrhythmic outcomes of lamin A/C mutation carriers. J Am Coll Cardiol 2016;68:2299–307. [DOI] [PubMed] [Google Scholar]
- 8. Moak JP, Barron KS, Hougen TJ, Wiles HB, Balaji S, Sreeram N. et al. Congenital heart block: development of late-onset cardiomyopathy, a previously underappreciated sequela. J Am Coll Cardiol 2001;37:238–42. [DOI] [PubMed] [Google Scholar]
- 9. Villain E, Coastedoat-Chalumeau N, Marijon E, Boudjemline Y, Piette JC, Bonnet D.. Presentation and prognosis of complete atrioventricular block in childhood, according to maternal antibody status. J Am Coll Cardiol 2006;48:1682–7. [DOI] [PubMed] [Google Scholar]
- 10. Kandolin R, Lehtonen J, Kupari M.. Cardiac sarcoidosis and giant cell myocarditis as causes of atrioventricular block in young and middle-aged adults. Circ Arrhythm Electrophysiol 2011;4:303–9. [DOI] [PubMed] [Google Scholar]
- 11. Nery PB, Beanlands RS, Nair GM, Green M, Yang J, McArdle BA. et al. Atrioventricular block as the initial manifestation of cardiac sarcoidosis in middle-aged adults. J Cardiovasc Electrophysiol 2014;25:875–81. [DOI] [PubMed] [Google Scholar]
- 12. Birnie DH, Nery PB, Ha AC, Beanlands RS.. Cardiac sarcoidosis. J Am Coll Cardiol 2016;68:411–21. [DOI] [PubMed] [Google Scholar]
- 13. Schmidt M, Pedersen L, Sorensen HT.. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol 2014;29:541–9. [DOI] [PubMed] [Google Scholar]
- 14. Brignole M, Auricchio A, Baron-Esquivias G, Bordachar P, Boriani G, Breithardt OA. et al. 2013 ESC Guidelines on cardiac pacing and cardiac resynchronization therapy: the task force on cardiac pacing and resynchronization therapy of the European Society of Cardiology (ESC). Developed in collaboration with the European Heart Rhythm Association (EHRA). Europace 2013;15:1070–118. [DOI] [PubMed] [Google Scholar]
- 15. Carlson SK, Patel AR, Chang PM.. Bradyarrhythmias in congenital heart disease. Card Electrophysiol Clin 2017;9:177–87. [DOI] [PubMed] [Google Scholar]
- 16. Kasar T, Ayyildiz P, Tunca Sahin G, Ozturk E, Gokalp S, Haydin S. et al. Rhythm disturbances and treatment strategies in children with congenitally corrected transposition of the great arteries. Congenit Heart Dis 2018;13:450–7. [DOI] [PubMed] [Google Scholar]
- 17. Strauss DG, Selvester RH, Lima JA, Arheden H, Miller JM, Gerstenblith G. et al. ECG quantification of myocardial scar in cardiomyopathy patients with or without conduction defects: correlation with cardiac magnetic resonance and arrhythmogenesis. Circ Arrhythm Electrophysiol 2008;1:327–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Groh WJ. Arrhythmias in the muscular dystrophies. Heart Rhythm 2012;9:1890–5. [DOI] [PubMed] [Google Scholar]
- 19. Brignole M, Deharo JC, De Roy L, Menozzi C, Blommaert D, Dabiri L. et al. Syncope due to idiopathic paroxysmal atrioventricular block: long-term follow-up of a distinct form of atrioventricular block. J Am Coll Cardiol 2011;58:167–73. [DOI] [PubMed] [Google Scholar]
- 20. Valeyre D, Prasse A, Nunes H, Uzunhan Y, Brillet PY, Muller-Quernheim J.. Sarcoidosis. Lancet 2014;383:1155–67. [DOI] [PubMed] [Google Scholar]
- 21. Gregoratos G, Cheitlin MD, Conill A, Epstein AE, Fellows C, Ferguson TB Jr. et al. ACC/AHA guidelines for implantation of cardiac pacemakers and antiarrhythmia devices: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Committee on Pacemaker Implantation). J Am Coll Cardiol 1998;31:1175–209. [DOI] [PubMed] [Google Scholar]
- 22.Global Burden of Disease Study 2013 Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990-2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 2015;386:743–800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ogunbayo GO, Elayi SC, Ha LD, Olorunfemi O, Elbadawi A, Saheed D. et al. Outcomes of heart block in myocarditis: a review of 31,760 patients. Heart Lung Circ 2019;28:272–6. [DOI] [PubMed] [Google Scholar]
- 24. Zysko D, Gajek J, Kozluk E, Mazurek W.. Electrocardiographic characteristics of atrioventricular block induced by tilt testing. Europace 2008;11:225–30. [DOI] [PubMed] [Google Scholar]
- 25. Brignole M, Moya A, de Lange FJ, Deharo JC, Elliott PM, Fanciulli A. et al. 2018 ESC guidelines for the diagnosis and management of syncope. Eur Heart J 2018;39:1883–948. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.