Abstract
Background:
Shared decision-making (SDM) has been found to be significantly and positively associated with improved patient outcomes. For an SDM process to occur, patients require functional, communicative, and critical health literacy (HL) skills.
Objective:
This study aimed to evaluate the impact of a program to improve health literacy skills for SDM in adults with lower literacy.
Methods:
An HL program including an SDM component (HL + SDM) and teaching of the three “AskShareKnow” questions was delivered in adult basic education settings in New South Wales, Australia. The program was evaluated using a partially cluster-randomized controlled trial comparing it to standard language, literacy, and numeracy (LLN) training. We measured the effect of these programs on (1) HL skills for SDM (conceptual knowledge, graphical literacy, health numeracy), (2) types of questions considered important for health decision-making, (3) preferences for control in decision-making, and (4) decisional conflict. We also measured AskShareKnow question recall, use, and evaluation in HL + SDM participants.
Key Results:
There were 308 participants from 28 classes enrolled in the study. Most participants had limited functional HL (71%) and spoke a language other than English at home (60%). In the primary analysis, the HL + SDM program compared with the standard LLN program significantly increased conceptual knowledge (19.1% difference between groups in students achieving the competence threshold; p = .018) and health numeracy (10.9% difference; p = .032), but not graphical literacy (5.8% difference; p = .896). HL + SDM participants were significantly more likely to consider it important to ask questions that would enable SDM compared to standard LLN participants who prioritized nonmedical procedural questions (all p < .01). There was no difference in preferences for control in decision-making or in decisional conflict. Among HL + SDM participants, 79% (n = 85) correctly recalled at least one of the AskShareKnow questions immediately post-intervention, and 35% (n = 29) after 6 months.
Conclusions:
Teaching SDM content increased participants' HL skills for SDM and changed the nature of the questions they would ask health care professionals in a way that would enable shared health decisions. [HLRP: Health Literacy Research and Practice. 2019;3(Suppl.):S58–S74.]
Plain Language Summary:
We developed a health literacy program that included a shared decision-making (SDM) section. The program was delivered in adult basic education classes by trained educators and compared to standard language, literacy, and numeracy training. Teaching SDM content increased participants' health literacy skills for SDM and changed the nature of the questions they would ask health care professionals.
Health care reforms in many countries have positioned the patient as a “consumer,” encouraging a more informed and active role in his or her health care. Shared decision-making (SDM) is the embodiment of this, and it involves patients and health professionals working together to make health care decisions (Charles, Gafni, & Whelan, 1997). The justifications for engaging patients in health care decision-making are many (Elwyn, Edwards, & Thompson, 2016). In addition to the ethical imperative, SDM is supported by evidence from 105 studies involving 31,043 people showing that patients have greater knowledge, are better informed, and are clearer about what matters most to them after receiving SDM support (Stacey et al., 2017). In many situations, informed patients elect for more conservative treatment options (Knops, Legemate, Goossens, Bossuyt & Ubbink, 2013).
Over time, SDM has been conceptualized both as a process and as an outcome. For an SDM process to occur, patients must communicate effectively and share information with health professionals, as well as be able to access, understand, and act on information about the nature of the condition and the clinical services available (including alternative options, risks, benefits, and uncertainties) (Makoul & Clayman, 2006; Towle & Godolphin, 1999). Patients also need the confidence and skills to communicate verbally with health care professionals and express personal values and preferences (Lown, Hanson, & Clark, 2009). These skills are consistent with the broader term “health literacy” (Nutbeam, 1998). In fact, research has shown that, at different times in the SDM process, all levels of health literacy skills (functional, communicative, and critical) (Nutbeam, 2000) are required for engagement with health care professionals (Smith, Nutbeam & McCaffery, 2013; Muscat, Shepherd et al., 2017). As an outcome, the ability to make a shared health decision is a positive measure of higher-level health literacy skills.
There has been significant growth in research and interventions throughout the past decade to address the causes and consequences of low health literacy in the community (Jacobs, Lou, Ownby, & Caballero, 2014; Sheridan et al., 2011). However, there are few examples of interventions to develop health literacy skills that facilitate autonomy and empowerment as well as promote collaborative decision-making between professionals and consumers. Similarly, although there has been steady growth in the number of studies of SDM interventions, there is relatively little work targeting adults with lower literacy, who are the people typically least involved in health decision-making yet potentially could benefit the most from greater participation (Durand et al., 2014). This is consistent with a previous analysis of a systematic review of patient decision aids that showed patients with lower baseline levels of knowledge had a relatively greater benefit than those with higher knowledge levels (Gentles, Stacey, Bennett, Alshurafa, & Walter, 2013).
Health care consumers with poor literacy are a “hard-to-reach” group, as they often feel ashamed about their literacy skills and are not able to disclose them to health care professionals (Parikh, Parker, Nurss, Baker, & Williams, 1996). The constraints of clinical care often result in limited time to adequately prepare consumers to participate in decision-making (Joseph-Williams, Elwyn & Edwards 2014), and the delivery of interventions by coaches or literacy specialists in clinical settings is practically difficult and unsustainable (Joseph-Williams, Edwards & Elywn, 2014). An alternative approach to engaging consumers with lower literacy is through established adult education programs (Rowlands & Nutbeam, 2013). The feasibility of this type of partnership has been examined elsewhere and shown to facilitate meaningful support in health-related learning for those most in need (Chen, Goodson, & Acosta, 2015; Tavistock Institute and Shared Intelligence, 2008). Conceptually, SDM aligns with several theories of adult learning. Knowles' Adult Learning Theory, for example, suggests that adults have a deep psychological need to be self-directing and responsible for their own lives; however it acknowledges that they may need support in assuming a self-directing role in contexts in which they have typically been more dependent (Knowles, 1980; Tiedeman & Knowles, 1979).
Objective
This study aimed to evaluate the impact of a program designed to improve health literacy skills for SDM in adults with lower literacy.
Methods
Intervention
We developed a health literacy program for adults with lower literacy to be run through established adult learning programs in New South Wales (NSW), Australia (McCaffery et al., 2016). The program was adapted from the United Kingdom Skilled for Health program (Tavistock Institute and Shared Intelligence, 2008) to focus on Australian public health priorities and included 30 health topics (10 core units and 20 elective units). We added a core 6-hour SDM component that aimed to build students' skills and self-efficacy to participate in health care decision-making. SDM content was developed in collaboration with an adult education expert and revised on the basis of feedback from three adult education teachers (Muscat et al., 2015). The content is summarized in Table 1. This article focuses on the evaluation of SDM outcomes only.
Table 1.
Shared Decision-Making Content Overview
| Part 1: Introduction to Shared Decision-Making | |
| Content Patients' rights to be involved in health decision-making The role of values and preferences in health decision-making |
Selected classroom activities and resources Class discussion of students' past experiences making health decisions, with supplementary visual representation of shared decision-making Individual written activity (cloze-passage) defining shared decision-making Class discussion about potential contributions of doctors (e.g., medical knowledge for diagnosis) and patients (e.g., values and preferences) to health care decision-making, with supplementary cut-and-paste activity |
| Part 2: Engaging in Shared Decision-Making by Asking Questions | |
| Content The AskShareKnow questions (Shepherd et al., 2011) as a means to participate in shared decision-making: What are my options? What are the benefits and harms of those options? How likely are each of those benefits and harms to happen to me? Development of skills for numerical and graphical risk under-standing |
Selected classroom activities and resources Group reading activity introducing the AskShareKnow questions Class discussions about AskShareKnow terminology with supplementary worksheets Conceptual risk worksheets with non-clinical (e.g. likelihood that winter will be colder than summer) and clinical examples (e.g., likelihood of harms from beta-blocker medications for different patients) Numerical risk worksheets (percentages; fractions; icon arrays) with multiple representations and worked examples Class brainstorming about the potential benefits of using the AskShareKnow questions |
| Part 3: Developing Self-Efficacy to Participate in Decision-Making | |
| Content Overcoming barriers to shared decision-making Cognitive and behavioral rehearsal of learned information |
Selected classroom activities and resources AskShareKnow modelling video. Class role play of engaging in shared decision-making in a health care encounter Class discussion about ways to overcome common barriers to shared decision-making Individual lesson revision worksheet |
Study Setting and Design
This study was conducted at Technical and Further Education (TAFE) institutes during 2014. TAFE institutes in NSW provide low-cost and government-funded adult basic education courses across the state, including metropolitan and regional areas. Students may enroll without completing secondary schooling, and courses are delivered by trained adult educators.
This study was intended to be a matched cluster- randomized controlled trial (McCaffery et al., 2016). However, the final study was a partial cluster-randomized controlled trial (see below and McCaffery et al., 2019 for details). The University of Sydney Human Research Ethics Committee (2013/938) and each participating TAFE institute approved the trial.
Recruitment and Randomization
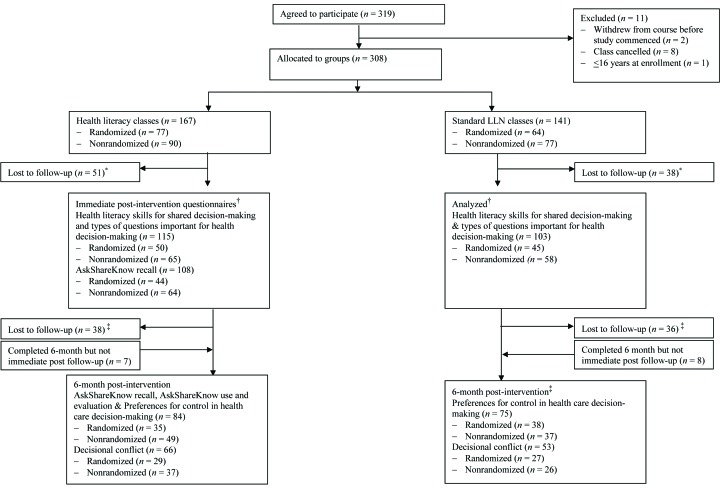
At enrollment, students older than age 16 years in matched classes at the same site were randomized into classes when possible. Students who had already been allocated to classes prior to joining the study (e.g., classes who had already been working with the same teacher in a prior semester, or classes at different sites) were randomized at the class level. Some TAFE sites indicated they would not participate in the study if they could not select which classes received the intervention. In some cases, this was due to a strong preference for the health content and for others it was because teachers felt the standard program was needed for students to focus on employment-related skills such as improving computer literacy. In total, 12 (of 28) classes were randomized (Figure 1). All participants were blinded to the intervention insofar as they were not informed that the purpose of the study was to evaluate a health literacy program.
Figure 1.
Flow of participants through trial. LLN = language, literacy, and numeracy. *Reasons for loss to immediate follow-up (course dropout or absence during data collection sessions) include sickness, overseas travel, gained employment. †Time between shared decision-making training and immediate follow-up could range from 2 to 6 weeks. ‡Reasons for loss to 6-month follow-up include changed address and difficulty completing forms.
Study Groups
Language, literacy, and numeracy (LLN) courses seek to improve general skills in reading, writing, numeracy, listening, and speaking. Standard LLN participants received one semester of basic/beginner skills training embedded within non-health topics (e.g., employment skills, environment). Health literacy participants also received one semester of basic/beginner LLN skills training delivered by a trained adult educator but embedded within health-related topics (e.g. taking temperatures, reading medicine labels [see McCaffery et al., 2019 for a full list of topics]). These participants were informed of the focus on health by their teacher at the beginning of the semester. SDM was included as a core topic (6 hours of class time).
Data Collection and Outcome Measures
Demographic information (e.g., age, gender, health literacy, language spoken at home) was collected at baseline. SDM outcomes were compared between groups post-intervention only (immediately and 6-months post-intervention) using four outcome measures: (1) health literacy skills for SDM (i.e., conceptual knowledge, graphical literacy, health numeracy), (2) types of questions considered important for health decision-making, (3) preferences for control in health care decision-making, and (4) decisional conflict. We also measured AskShareKnow question recall, use, and evaluation among participants in the health literacy arm (Table 2). All data were collected in English using paper-based questionnaires within regular classroom instruction time. Although teachers were present and could assist students in reading difficult words, students were required to answer questions independently.
Table 2.
Shared Decision-Making Outcomes and Data Collection Schedule
| Measure | Description of Measure and Scoring | Immediate Follow-Up | 6-Month Follow-Up | ||
|---|---|---|---|---|---|
| HL +SDM | Standard LLN | Health Literacy | HL + SDM | ||
| Health literacy skills for shared decision-making |
Measure: A 14-item curriculum-based questionnaire, purpose-designed for this study. The questionnaire was comprised of four multiple-choice items assessing conceptual knowledge of shared decision-making, seven multiple-choice graphical literacy items based on a purpose-designed 100-item icon array, and three health numeracy items that were taken from an existing numeracy scale (Lipkus, Samsa, & Rimer, 2001). These reflected the components of literacy as identified by Kindig, Panzer, and Nielsen-Bohlman (2004). Adult education experts conducted an external review of questionnaire content. We developed a shortened (5-item) version of the questionnaire for classes experiencing difficulty completing assessments Scoring: A marking scheme was developed a priori. We used the 3-level Anghoff method to determine a passing (cut) score for the questionnaire overall and for each subscale (Yudkowsky, Downing, & Popescu, 2008). Eight experts in shared decision-making independently rated if a hypothetical minimally competent learner would perform each item correctly: yes (1), maybe (0.5), or no (0). Scores were summed across items and totals were averaged across raters to determine the cut or passing score. For the overall measure, an a priori competence threshold of 9 of 14 items correct was set |
X | X | ||
| Types of questions considered important for health decision-making |
Measure: “Think about the next time you will visit your doctor. If your doctor tells you about a new test or treatment, what are three questions you might ask about the test or treatment?” in a free-response format Scoring: The content of individual responses was analyzed via content analysis (Hsieh & Shannon, 2005) |
X | X | ||
| Preferences for control in health care decision-making |
Measure: Control Preferences Scale (Solari et al., 2013). We used the “pick-one” administration method in which respondents are asked to pick a single response option that best corresponds with their control preference: (a) active, (b) active-shared, (c) collaborative, (d) passive-shared, and (e) passive. Scoring: Responses were categorized as patient-led (a–c) or physician-led (d–e) (Seo, Goodman, Politi, Blanchard, & Kaphingst, 2016) |
X | X | ||
| Decisional conflicta,b |
Measure: SURE (Sure of myself; Understand information; Risk-benefit ratio; Encouragement) 4-item test Scoring: Respondents reporting “no” to at least 1 of the SURE items (e.g., Did you feel SURE about the best choice for you?) categorized as experiencing decisional conflict (Légaré et al., 2010) |
X | X | ||
| AskShareKnow question recall |
Measure: Free-response format following methodology by Shepherd et al. (2016) Scoring: Two blinded markers scored responses (1 = correct recall; 0 = no evidence of correct recall), with any discrepancies resolved through discussion. Observed inter-rater agreement was >95% for all questions |
X | X | ||
| AskShareKnow question use |
Measure: Single item asking if participants had used each of the AskShareKnow questions (yes/no). If they had not used the questions, they were asked to indicate why in a free-response format Scoring: We analyzed the content of free responses through a process of coding and identifying themes to determine reasons that some participants did not use AskShareKnow questions (Hsieh & Shannon, 2005) |
X | |||
| AskShareKnow question evaluation |
Measure: All health literacy participants were asked to rate if they would recommend the AskShareKnow questions to others on a 4-point scale from 1 (definitely not) to 4 (yes, definitely) Scoring: Recommendations were combined into two categories: would recommend (1 and 2) and would not recommend (3 and 4) |
X | |||
Note. HL = health literacy; LLN = language, literacy, and numeracy; SDM = shared-decision making.
Decisional conflict refers to an individual's perception of uncertainty about the course of action to take when the choices involve risk, loss, regret, or a challenge to personal life values. It indicates an individual's level of comfort with a decision (Légaré et al., 2010). Although SURE was designed as a screening instrument to identify patients experiencing clinically significant decisional conflict prior to the consultation, the authors state that clinicians can “reduce the downstream effects of unresolved decisional conflict by ... providing appropriate support” (Légaré et al., 2010), and some empirical studies have found that increased patient involvement decreases decisional conflict (Hölzel, Kriston, & Härter, 2013).
Administered with participants who reported they had seen a health care professional since program completion only.
Statistical Analysis
Analyses were conducted using SPSS for Windows version 21 software. The significance threshold was set at p < .05. For all binary dependent variables, we fitted logistic regression models. Analyses were adjusted for baseline health literacy and clustering by class using generalized estimating equations with an exchangeable correlation matrix. In cases of complete separation (one question), we did not adjust for baseline health literacy.
An a priori decision was made by researchers and the study statistician to conduct the primary analysis with all participants (randomized and nonrandomized) while controlling for baseline differences to maximize sample size (Krzywinski & Altman, 2013). Given the issues with randomization, we conducted all analyses twice; once including all classes (28/28), and once including randomized classes only (12/28). Results from analyses including randomized participants only are summarized in the text and included in full in Table A, Table B, and Table C. Qualitative data was analyzed via content analysis (Table D).
Table A.
Analyses Including Randomized Participants Only
| Health literacy skills for shared decision-making (health literacy and standard language, literacy, and numeracy (LLN) arms) |
| Table C shows the number and percentage of participants in both groups who answered each health literacy skills item correctly. Forty of the 50 randomized health literacy participants who completed the whole measure (80.0%) had adequate overall health literacy skills (i.e., achieved the a priori competence threshold of 9 of 14 items correct) compared with 30 of 38 (78.9%) participants in the standard LLN group (p = .426). When looking at conceptual subscales, compared to standard language, literacy, and numeracy (LLN) participants, more randomized health literacy participants scored above the cut-score on the conceptual knowledge subscale (23.9% difference; p =. 106) and the health numeracy subscale (4.3% difference; p = .689). 78% of randomized health literacy participants had adequate graphical literacy scores compared to 74% of randomized standard LLN participants (p = .689). |
| Assessment of questions important for health decision-making (health literacy and standard LLN arms) |
| Of the 95 randomized participants who completed the assessment of questions important to health decision-making, health literacy participants were significantly more likely to consider questions about options, the benefits and harms of options, and the personal likelihood of the benefits and harms of different options to be important compared to standard LLN participants (all p < .01). Standard LLN participants were more likely to consider questions about harms only, process questions (covering questions about test/treatment location, timing, administration, and cost), and procedure clarification questions important to discuss with their doctor (all p < .05) (Table D). |
| Preferences for control in health care decision-making and decisional conflict (health literacy and standard LLN participants) |
| Most randomized participants in both groups (75% health literacy, 77% standard LLN) indicated a patient-involved decision-making preference (p = .870). Of those participants who had seen a health care professional since program completion, 69% of health literacy participants indicated that they did not experience decisional conflict compared to 60% of standard LLN participants (p = .129). |
Table B.
Analysis of Health Literacy Skills for Shared Decision-Making and AskShareKnow Question Recall and Use: Analyses with Randomized Participants Only (N = 95)
| Health Literacy Skill | HL (n = 50) | Standard LLN (n = 45) | Difference, % | p Value |
|---|---|---|---|---|
| n (% Correct) | n (% Correct) | |||
| Conceptual knowledge | ||||
| 1. What is shared decision-making? | 42 (84) | 32 (71.1) | 12.9 | |
| 2. Which word is most like the word options?a | 38 (76) | 28 (73.7) | 2.3 | |
| 3. Which word is most like the word benefit?a | 39 (78) | 25 (65.8) | 12.2 | |
| 4. Which word is most like the word harm?a | 43 (86) | 32 (84.2) | 1.8 | |
| ≥Subscale cut-score | 33 (66) | 16 (42.1) | 23.9 | .016 |
| Graphical literacyb | ||||
| 5. Which side effect is most likely? | 41 (82) | 43 (95.6) | −13.6 | |
| 6. Which side effect is least likely? | 36 (72) | 37 (82.2) | −10.2 | |
| 7. People are more likely to (experience/not experience side effects) | 36 (72) | 29 (64.4) | 7.6 | |
| 8. Out of 100 people, how many people will have a fever? | 44 (88) | 41 (91.1) | −3.1 | |
| 9. Out of 100 people, how many people will have headaches? | 44 (88) | 45 (100) | −12 | |
| 10. Choose a word to describe the risk of fevera,c | 32 (64) | 21 (55.3) | 8.7 | |
| 11. Choose a word to describe the risk of headachesa,c | 30 (60) | 16 (42.1) | 17.9 | |
| ≥Subscale cut-score | .426 | |||
| Health numeracyd | ||||
| 12. Which of the following numbers represents the biggest risk of getting a disease? (frequency)a | 35 (70) | 27 (71.1) | 1.1 | |
| 13. Which of the following numbers represents the biggest risk of getting a disease? (percentage)a | 43 (86) | 31 (81.6) | 4.4 | |
| 14. If the chance of getting a disease is 20 out of 100, this would be the same as a ___% chance of getting the diseasea | 38 (76) | 28 (73.7) | 2.3 | |
| ≥Subscale cut-score | 39 (78) | 28 (73.7) | 4.3 | .689 |
Note: HL = health literacy; LLN = language, literacy, and numeracy.
Question excluded from shortened health literacy skills questionnaire; data missing for seven Standard LLN participants.
Items based on a purpose-designed 100-patient icon array.
Multiple response options marked correct for items 6 and 7, which required participants to select verbal probability labels (e.g., Likely) to represent numerical risk estimates (e.g., 33/100) given individual variation in understanding verbal probability labels (Beyth-Marom, 1982; Budescu & Wallsten, 1985).
Health numeracy questions were items 1, 2, and 6 on the Expanded Numeracy Scale (Lipkus et al., 2001) assessing percentage and natural frequency presentations of risk to best reflect the numeracy content of our shared decision-making program.
Table C.
Assessment of Questions Important for Health Decision-Making: Analyses with Randomized Participants Only (N = 95)
| Category | Definition | Example of Questions from Participantsa | Health Literacy (n= 50) | Standard LLN (n= 45) | Test Statistics |
|---|---|---|---|---|---|
| n(%) | n(%) | p Value | |||
| Options | Questions about whether there are alternative test or treatment options available to choose from | “Could you tell me which are my options please?” | 28 (56) | 1 (2.2) | .001 |
| Benefits and harms | Questions about both potential benefits and potential harms of test and treatment options | “What is the benefit for me, anything can harm me?” | 25 (50) | 1 (2.2) | .004 |
| Personal likelihood of benefits and harms | Questions about the likelihood of benefits and harms occurring to individual patients | “How likely are they [benefits and harms] to happen to me?” | 17 (34) | 1 (2.2) | .016 |
| Harms only | Questions about the harms, or side-effects, associated with different test or treatment options, without asking about benefits | “What side effects would I have from it?” | 9 (18) | 18 (40) | .038 |
| Benefits only | Questions about benefits associated with different test or treatment options, without asking about harms | “What is the benefits from the treatment?” | 2 (4) | 1 (2.2) | .816 |
| Process | Questions about the process involved in undergoing the test/treatment, such as what actions need to be taken, test/treatment duration, when and where the test/treatment is performed and by whom, and how much the test/treatment costs | “When will I need to start treatment?” | 13 (26) | 30 (66.7) | <.001 |
| Procedure clarification | Questions about why the patient is undergoing a new test/treatment, and if it was going to work | “Why I do the test?” | 9 (18) | 22 (48.9) | .003 |
| Results/outcome | Questions about what test results might show/what would be the clinical outcome after treatment | “How long does it take to see any changes/improvements?” | 2 (4) | 4 (8.9) | .424 |
| Unable to interpret/miscellaneous | Questions that do not fit into any other category or that the research team cannot interpret | “I going to the doctor because I my sick” | 9 (18) | 16 (35.6) | .014 |
Note.
Questions were transcribed verbatim from participant responses and are not all grammatically correct.
Table D.
Content Analysis Methods: Assessment of Questions Important for Health Decision-Making
| Coding began deductively based on shared decision-making concepts embodied in the AskShareKnow questions. Two double-blinded coders reviewed all data and coded any questions that matched 1 of 5 categories: (1) options, (2) the benefits and harms of options, (3) the personal likelihood of the benefits and harms, (4) harms only, and (5) benefits only (items 1–5, Table 2) (Elo & Kyngäs, 2008). Any discrepancies were resolved through discussion between markers (inter-rater agreement >95% for all questions). Remaining responses were coded inductively with categories derived from the data (Elo & Kyngäs, 2008). Inductive codes were collected by the first author to form coding sheets and categories were freely generated and grouped through the abstraction process (Elo & Kyngäs, 2008). The coding scheme was revised over a three-round iterative process of discussion and revision involving D. M., K. J. M., S. M., S. K. S., H. L. S., and H. M. D. We created four categories from the remaining responses: (1) process questions (covering questions about test/treatment location, timing, administration and cost), (2) procedure clarification, (3) test/treatment outcomes, and (4) miscellaneous/unable to interpret. |
Results
In total, 319 students from 10 TAFE institutes of NSW agreed to participate in the program. After exclusions, 308 participated in the study; 167 in the health literacy plus SDM training (HL + SDM) arm, and 141 in the standard LLN arm. Immediately post-intervention, 115 (69%) of HL + SDM participants and 103 (73%) of standard LLN participants completed the health literacy skills for SDM questionnaire and the assessment of questions important for health decision-making. Reasons for dropout are described in McCaffery et al. (2019). One hundred and eight (65%) HL + SDM participants completed the AskShareKnow question recall, use, and evaluation. Six-month assessments were completed by 84 (50%) of HL + SDM participants and 75 (53%) of standard LLN participants (Figure 1).
Demographic Characteristics
The demographic characteristics presented here and in Table 3 differ slightly from that presented in the companion article in this issue (McCaffery et al., 2019), as the latter only reports the characteristics of the sample with both baseline and immediate follow-up data on at least one primary outcome measure for that study. Most participants were female (72%), spoke a language other than English at home (60%), and were from metropolitan areas (65%). Mean age at baseline was 46 years. Most participants (71%) had limited functional health literacy (i.e., had Newest Vital Sign scores <4), and 68% reported having a longstanding illness or disability.
Table 3.
Demographic Information and Baseline Health Literacy for All Participants Enrolled in the Study
| Participant Information | Overall | Health Literacy | Standard LLN | |||
|---|---|---|---|---|---|---|
|
|
|
|
||||
| n | M (SD) or % | n | M (SD) or % | n | M (SD) or % | |
|
| ||||||
| Demographicsa | ||||||
|
| ||||||
| Age (years) | ||||||
| Mean (SD) | 303 | 46.3 (14.8) | 166 | 44.9 (14) | 137 | 48 (15.5) |
| Mean (SD) randomized only | 136 | 47.9 (13.2) | 76 | 48.7 (11.9) | 60 | 46.9 (14.6) |
|
| ||||||
| Gender | ||||||
| Female | 303 | 72 | 165 | 69 | 138 | 77 |
| Female randomized only | 139 | 79 | 77 | 78 | 62 | 81 |
|
| ||||||
| Region (metropolitan/regional) | ||||||
| Metropolitan | 308 | 65 | 167 | 67 | 141 | 63 |
| Metropolitan randomized only | 141 | 87 | 77 | 87 | 64 | 86 |
|
| ||||||
| Language spoken at home | ||||||
| English | 278 | 40 | 147 | 33 | 131 | 47 |
| English randomized only | 135 | 28 | 72 | 26 | 63 | 30 |
|
| ||||||
| Longstanding illness/disability | ||||||
| Yes | 289 | 65 | 161 | 70 | 128 | 59 |
| Yes randomized only | 133 | 68 | 77 | 75 | 56 | 57 |
|
| ||||||
| Baseline health literacy | ||||||
|
| ||||||
| Newest Vital Sign | ||||||
| Limited HL (0–3) | 285 | 71 | 158 | 79 | 127 | 60 |
| Limited HL randomized only | 133 | 76% | 77 | 78 | 56 | 73 |
|
| ||||||
| Self-rated reading ability | ||||||
| Limited HL | 257 | 61 | 138 | 65 | 119 | 58 |
| Limited HL randomized only | 115 | 75 | 65 | 77 | 50 | 72 |
|
| ||||||
| Single item literacy screener | ||||||
| Limited HL | 264 | 75 | 143 | 80 | 121 | 69 |
| Limited HL randomized only | 123 | 80 | 70 | 79 | 53 | 81 |
Note. HL = health literacy; LLN = language, literacy, and numeracy.
Demographics differ slightly from the companion article (McCaffery et al., 2019), which only reports demographic characteristics of the sample with both baseline and immediate follow-up data on at least one primary outcome measure for that study.
Analyses Including Randomized and Nonrandomized Participants
Health literacy skills for SDM (HL + SDM and standard LLN arms). Table 4 shows the number and percentage of participants in both arms who answered each health literacy skills item correctly. Two thirds (n = 77; 67%) of the 115 HL + SDM participants had adequate overall health literacy skills (i.e., achieved the a priori competence threshold of 9 of 14 items correct) compared with 46 (48%) of 96 participants in the standard LLN group (p = .217). Compared to standard LLN participants, more HL + SDM participants scored above the cut-score on the conceptual knowledge subscale (19.1% difference; p =.018) and the health numeracy subscale (10.9% difference; p = .032). Seventy-two percent of HL + SDM participants had adequate graphical literacy scores compared to 78% of standard LLN participants (p =.896).
Table 4.
Analysis of Health Literacy Skills for Shared Decision-Making (N = 218)
| Questions | HL (n = 115) | Standard LLN (n = 103) | Difference, % | p Value |
|---|---|---|---|---|
| n (%) Correct | n (%) Correct | |||
| Conceptual knowledge | ||||
| 1. What is shared decision-making? | 104 (90.4) | 80 (77.7) | 12.7 | |
| 2. Which word is most like the word options?a | 95 (82.6) | 69 (71.9) | 10.7 | |
| 3. Which word is most like the word benefit?a | 91 (79.1) | 65 (67.7) | 11.4 | |
| 4. Which word is most like the word harm?a | 94 (81.7) | 77 (80.2) | 1.5 | |
| ≥ Subscale cut-score | 77 (67) | 46 (47.9) | 19.1 | .018 |
| Graphical literacyb | ||||
| 5. Which side effect is most likely? | 97 (84.3) | 88 (85.4) | −1.1 | |
| 6. Which side effect is least likely? | 85 (73.9) | 81 (78.6) | −4.7 | |
| 7. People are more likely to (experience/not experience side effects) | 80 (69.6) | 72 (69.9) | −0.3 | |
| 8. Out of 100 people, how many people will have a fever? | 101 (87.8) | 93 (90.3) | −2.5 | |
| 9. Out of 100 people, how many people will have headaches? | 101 (87.8) | 98 (95.1) | −7.3 | |
| 10. Choose a word to describe the risk of fevera,c | 78 (67.8) | 56 (58.3) | 9.5 | |
| 11. Choose a word to describe the risk of headachesa,c | 71 (61.7) | 45 (46.9) | 14.8 | |
| ≥ Subscale cut-score | 82 (71.3) | 74 (77.1) | −5.8 | .896 |
| Health numeracyd | ||||
| 12. Which of the following numbers represents the biggest risk of getting a disease? (frequency)a | 80 (69.6) | 57 (59.4) | 10.5 | |
| 13. Which of the following numbers represents the biggest risk of getting a disease? (percentage)a | 93 (80.9) | 72 (75) | 5.9 | |
| 14. If the chance of getting a disease is 20 out of 100, this would be the same as a ___% chance of getting the disease?a | 88 (76.5) | 65 (67.7) | 8.8 | |
| ≥ Subscale cut-score | 88 (76.5) | 63 (65.6) | 10.9 | .032 |
Note. HL = health literacy; LLN = language, literacy, and numeracy.
Question excluded from shortened health literacy skills questionnaire; data missing for seven Standard LLN participants.
Items based on a purpose-designed 100-patient icon array.
Multiple response options marked correct for items 6 and 7, which required participants to select verbal probability labels (e.g., Likely) to represent numerical risk estimates (e.g., 33/100) given individual variation in understanding verbal probability labels (Beyth-Marom, 1982; Budescu & Wallsten, 1985).
Health numeracy questions were items 1, 2, and 6 on the Expanded Numeracy Scale (Lipkus et al., 2001) assessing percentage and natural frequency presentations of risk to best reflect the numeracy content of our shared decision-making program.
Types of questions considered important for health decision-making (HL + SDM and standard LLN arms). Of the 218 participants who completed the assessment of questions important to health decision-making, HL + SDM participants were significantly more likely to consider questions about options, the benefits and harms of options, and the personal likelihood of the benefits and harms of different options to be important compared to standard LLN participants (all p <.01). Standard LLN participants were more likely to consider procedural questions (covering questions about test/treatment location, timing, administration, and cost) and clarification questions important to discuss with their doctor (all p <.01) (Table 5).
Table 5.
Assessment of Questions Important for Health Decision-Making (N = 218)
| Category | Definition | Example | HL+SDM (n = 115) | Standard LLN (n = 103) | Test Statistics |
|---|---|---|---|---|---|
| n(%) | n(%) | p Value | |||
| Options | Questions about whether there are alternative test or treatment options available to choose from | Could you tell me which are my options please? | 62 (53.9) | 1 (1) | <.001 |
| Benefits and harms | Questions about both potential benefits and potential harms of test and treatment options | What is the benefit for me, anything can [sic] harm me? | 57 (49.6) | 3 (2.9) | <.001 |
| Personal likelihood of benefits and harms | Questions about the likelihood of benefits and harms occurring to individual patients | How likely are they [benefits and harms] to happen to me? | 43 (37.4) | 1 (1) | .001 |
| Harms only | Questions about the harms, or side-effects, associated with different test or treatment options, without asking about benefits | What side effects would I have from it? | 31 (27) | 40 (38.8) | .243 |
| Benefits only | Questions about benefits associated with different test or treatment options, without asking about harms | What is [sic] the benefits from the treatment? | 3 (2.6) | 2 (1.9) | .775 |
| Procedural questions | Questions about the procedures involved in undergoing the test/treatment, such as what actions need to be taken, test/treatment duration, when and where the test/treatment is performed and by whom, and how much the test/treatment costs | When will I need to start treatment? | 38 (33) | 77 (74.8) | <.001 |
| Clarification questions | Questions about why the patient is undergoing a new test/treatment | Why do I need the test? | 20 (17.4) | 48 (46.6) | .001 |
| Results/outcome | Questions about what test results might show or what would be the clinical outcome after treatment | How long does it take to see any changes/improvements? | 3 (2.6) | 8 (7.8) | .218 |
| Unable to interpret/miscellaneous | Questions that do not fit into any other category or cannot be interpreted by the research team | I am going to the doctor because I my [sic] sick | 13 (11.3) | 26 (25.2) | .013 |
Note: HL = health literacy; LLN = language, literacy, and numeracy. SDM = shared decision-making.
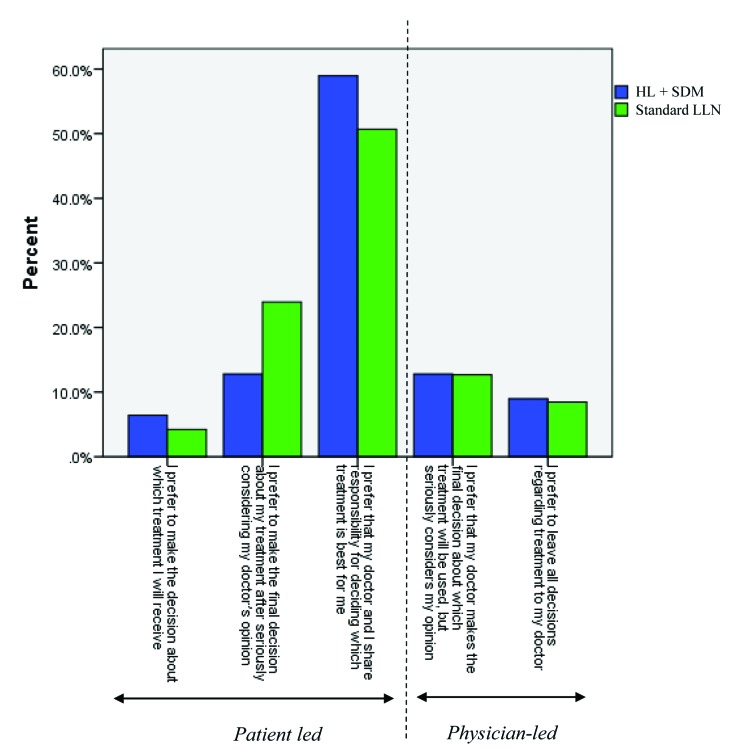
Preferences for control in health care decision-making and decisional conflict (HL + SDM and standard LLN arms). Most participants in both groups (78% HL + SDM, 79% standard LLN) indicated a patient-led decision-making preference (p = .920) (Figure 2). Of those participants who had seen a health care professional since program completion, 68% of HL + SDM participants indicated that they did not experience decisional conflict compared to 60% of standard LLN participants (p = .458). There were no statistically significant differences between groups.
Figure 2.
Percentage of participants selecting each item on the Control Preferences Scale, stratified by group. HL = health literacy; LLN = language, literacy, and numeracy. SDM = shared decision-making.
Analyses Including Randomized Participants Only
Results from analyses including randomized participants only are reported in full in Table A, Table B, and Table C. Summarized here are any outcomes for which the statistical significance differed between the two sets of analyses.
For health literacy skills for SDM, there was no longer a statistically significant difference between study arms in the number of participants with adequate knowledge on the conceptual knowledge subscale or the numeracy subscale after controlling for baseline health literacy. Thirty-three (66%) of HL + SDM participants achieved the a priori competence threshold for conceptual knowledge compared to 16 (42%) of standard LLN participants (24% difference; p = .106). Thirty-nine (78%) of HL + SDM participants achieved the a priori competence threshold for health numeracy compared to 28 (74%) of standard LLN participants (4% difference; p = .689).
For the types of questions important for health decision-making, after controlling for baseline health literacy, significantly more standard LLN participants (n = 18; 40%) asked about harms only compared to randomized HL + SDM participants (n = 9; 18%) (p = .038).
For all other outcomes, there were no differences between the analyses including all participants and the analyses including randomized participants only.
Recall and Use of AskShareKnow Questions (Health Literacy Arm Only)
Recall of the AskShareKnow questions was assessed only in the HL + SDM arm. Of the 108 health literacy participants who completed the immediate post-intervention questionnaire, 79% (n = 85) correctly recalled at least one AskShareKnow question, with 55% (n = 59) correctly recalling all three questions. After 6 months, 35% (n = 29) recalled at least one question, and 30% (n = 25) all three (Table 6).
Table 6.
Analysis of AskShareKnow Question Recall and Use (N = 108)
| AskShareKnow Question | Recall | Use | |
|---|---|---|---|
| Immediate Post (n = 108) | 6 Months Post (n= 84) | 6 Months Post (n = 73) | |
| n (%) | n (%) | n (%) | |
| 1. What are my options? | 85 (78.7) | 29 (34.5) | 26 (35.6) |
| 2. What are the benefits and harms of those options? | 72 (66.7) | 26 (31) | 25 (34.2) |
| 3. How likely is each of those benefits and harms to happen to me? | 64 (59.3) | 26 (31) | 20 (27.4) |
| 4. All three questions | 59 (54.6) | 25(29.8) | 20 (27.4) |
| 5. At least one question | 85 (78.7) | 29 (34.5) | 26 (35.6) |
The majority (n = 73, 87%) of HL + SDM participants who completed the 6-month post-intervention questionnaire indicated that they had seen a health care professional since program completion. Of those, 36% (n = 26) reported asking at least one of the AskShareKnow questions (Table 6). Reported reasons for not asking the questions included (1) unable to remember the question, (2) forgot to ask the question during the consultation, and (3) felt they had adequate information without asking the questions.
In total, 91% of HL + SDM participants reported at 6-month follow-up that they would “definitely” or “probably” recommend the AskShareKnow questions to others who needed to make a health care decision.
Discussion
Our health literacy training program (including an SDM component) is one approach to developing health literacy capabilities, tested first within an adult basic education setting. In our study, most participants in both the HL + SDM and standard LLN arms indicated a preference to be involved in decision-making. However, after intervention delivery, our primary analysis indicated those in the HL + SDM group had significantly higher health literacy skills for SDM (including conceptual knowledge and health numeracy skills) and were more likely to consider it important to ask questions that would enable informed SDM (e.g., questions about test/treatment options). By contrast, standard LLN participants prioritized questions clarifying the recommended treatment or nonmedical procedural questions, which may reflect a more passive acceptance of the test/treatment options presented to them. Immediately post-intervention, health literacy participants had a high recall of generic SDM questions (AskShareKnow), and recall of at least one question was retained after 6 months by more than one-third of the health literacy group. There were no differences in decisional conflict between groups. In the analysis of the randomized-only groups, some differences between groups disappeared; the percentage of participants who achieved the a priori competence threshold for conceptual knowledge and health numeracy did not differ significantly between groups, but significantly more standard LLN participants asked about harms only compared to the health literacy arm. Because this analysis was underpowered, findings are inconclusive on these measures.
There are relatively few examples of interventions to develop functional, communicative, and critical health literacy skills that facilitate greater autonomy and empowerment, as well as promote collaborative decision-making between professionals and consumers with lower literacy (Manafo & Wong, 2012; Nutbeam, 2008). From a teaching perspective, our program has been shown to be feasible to implement (Muscat et al., 2016), with good fit between the SDM program content and institutional objectives (Muscat, Morony et al., 2017). Qualitative evaluation with teachers and students also suggests the course empowered students with confidence to play a more active role in their health care (Muscat, Shepherd et al., 2017). Together with the results presented here, this suggests that tailored interventions can address the specific challenges groups face in relation to SDM (e.g., language and numeracy challenges among adults with lower literacy) to build skills, confidence, and health literacy capacity for those most in need. As advocated in the context of adult learning, interventions to support SDM must shift from simple transmission of information to facilitating skills development for self-directed inquiry that can be used in multiple decision contexts over a consumers' life-course (Tiedeman & Knowles, 1979).
Strengths and Limitations
We experienced practical challenges in evaluating this program using a randomized design. Running an evaluation in a real-world setting, the need for engagement and commitment to the program meant that randomization was not possible in all participating TAFE colleges. To account for this in the analysis, we conducted all analyses twice: once with all participants and once with randomized participants only. A trial in which all participants are allocated to groups randomly would provide stronger evidence of the impact of SDM training for adults with lower literacy. In addition, the SDM program formed part of a larger semester-long health literacy intervention, including other health-related topics. Having a multicomponent intervention makes it difficult to specify the “active ingredients” of the intervention, and we may have varied effects if we delivered the SDM component as a stand-alone intervention (Craig et al., 2008). Although the inclusion of longer-term (6-month) follow-up is a strength, considerable attrition 6 months post-intervention increases the risk of bias in our study (although there was similar attrition across trial arms). Dropout may be partially attributable to restructuring of the Australian adult education system that occurred during the follow-up period, which meant that many students were no longer enrolled in TAFE colleges. However, high attrition is common in health literacy interventions and work is needed to investigate how to retain participants throughout health literacy trials (Brainard, Wilsher, Salter, & Loke, 2016).
In terms of measurement, currently, there are no general measures assessing consumer health literacy skills for SDM. We used a competency-based approach with input from adult education experts. We applied standard-setting to determine competence (as opposed to applying an arbitrary cut-score or a median split that is relative to the observed data) rather than an absolute standard (Ghanouni, Renzi, Meisel, & Waller, 2016). However, the 14-item curriculum-based measure is not validated. Further validation of the measure and competence cut-score would be useful to help to identify and address specific deficits in health literacy that would otherwise act as a barrier to SDM. Future studies may also benefit from more substantive patient-oriented outcomes such as assessing actual consultation behavior change rather than relying on self-reports that questions were asked, which is subject to social desirability bias (Brainard et al., 2016). For example, doctor-patient/consumer consultation recordings could be analyzed to assess the impact of the program on the quantity and type of information elicited from providers. This would also enable us to assess the impact of clinical (e.g., presenting symptoms/reason for the visit) and contextual (e.g., health care providers' receptiveness to question-asking) factors on students' capacity or willingness to use newfound skills or to ask questions.
Conclusion
Teaching SDM content increased participants' health literacy skills for SDM and changed the nature of the questions they would ask health care professionals in a way that would enable them to make informed health decisions. To meaningfully address health literacy, we need to continue to investigate tailored modes of support and sustainable avenues for delivery that can facilitate functional, communicative, and critical skill development. Our research suggests that by taking this approach we can support the development of skills that can facilitate autonomy and participation in health care decision-making for those most in need.
Acknowledgments
The authors thank the New South Wales (NSW) Technical and Further Education (TAFE) teachers and students who participated in the program. They thank the expert raters who helped determine the health literacy skills for the shared decision-making questionnaire cut-score using the Anghoff method, as well as Steve Forsyth, Joy Duncan, Leonie Lagana, Sandra Lawrence, and Llewella-Sue Cobbin (NSW TAFE) for helping us with the TAFE staff training, review of shared decision-making content and assessments, and for providing logistical support to run the program. The authors also thank the Linkage Partners who worked on this project: NSW Clinical Excellence Commission, NSW Health, NSW TAFE, and NPS MedicineWise.
References
- Beyth-Marom R. (1982). How probable is probable? A numerical translation of verbal probability expressions. Journal of Forecasting, 1(3), 257–269. 10.1002/for.3980010305 [DOI] [Google Scholar]
- Brainard J. Wilsher S. H. Salter C. Loke Y. K. (2016). Methodological review: Quality of randomized controlled trials in health literacy. BMC Health Services Research, 16(1), 246. 10.1186/s12913-016-1479-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budescu D. V. Wallsten T. S. (1985). Consistency in interpretation of probabilistic phrases. Organizational Behavior and Human Decision Processes, 36(3), 391–405. 10.1016/0749-5978(85)90007-X [DOI] [Google Scholar]
- Charles C. Gafni A. Whelan T. (1997). Shared decision-making in the medical encounter: What does it mean? (or it takes at least two to tango). Social Science & Medicine, 44(5), 681–692. 10.1016/S0277-9536(96)00221-3 [DOI] [PubMed] [Google Scholar]
- Chen X. Goodson P. Acosta S. (2015). Blending health literacy with an English as a second language curriculum: A systematic literature review. Journal of Health Communication, 20(2),101–111. 10.1080/10810730.2015.1066467 [DOI] [PubMed] [Google Scholar]
- Craig P. Dieppe P. Macintyre S. Mitchie S. Nazareth I. Petticrew M. (2008). Developing and evaluating complex interventions: The new Medical Research Council guidance. British Medical Journal, 337, a1655. 10.1136/bmj.a1655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durand M. Carpenter L. Dolan H. Bravo P. Mann M. Bunn F. Elwyn G. (2014). Do interventions designed to support shared decision-making reduce health inequalities? A systematic review and meta-analysis. Plos One, 9(4), e94670. 10.1371/journal.pone.0094670 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elo S. Kyngäs H. (2008). The qualitative content analysis process. Journal of Advanced Nursing, 62(1), 107–115. 10.1111/j.1365-2648.2007.04569.x [DOI] [PubMed] [Google Scholar]
- Elwyn G. Edwards A. Thompson R. (2016). Shared decision making in health care: Achieving evidence-based patient choice (3rd ed.). Oxford, UK: Oxford University Press; 10.1093/acprof:oso/9780198723448.001.0001 [DOI] [Google Scholar]
- Gentles S. J. Stacey D. Bennett C. Alshurafa M. Walter S. D. (2013). Factors explaining the heterogeneity of effects of patient decision aids on knowledge of outcome probabilities: A systematic review sub-analysis. Systematic Reviews, 21(2), 95. 10.1186/2046-4053-2-95 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghanouni A. Renzi C. Meisel S. F. Waller J. (2016). Common methods of measuring ‘informed choice’ in screening participation: Challenges and future directions. Preventive Medicine Reports, 4, 601–607. 10.1016/j.pmedr.2016.10.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hölzel L. P. Kriston L. Härter M. (2013). Patient preference for involvement, experienced involvement, decisional conflict, and satisfaction with physician: A structural equation model test. BMC Health Services Research, 13(1), 231–231. 10.1186/1472-6963-13-231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H.-F. Shannon S. E. (2005). Three approaches to qualitative content analysis. Qualitative Health Research, 15(9), 1277–1288. 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- Jacobs R. J. Lou J. Q. Ownby R. L. Caballero J. (2014). A systematic review of eHealth interventions to improve health literacy. Health Informatics Journal, 22(2), 81–98. 10.1177/1460458214534092 [DOI] [PubMed] [Google Scholar]
- Joseph-Williams N. Edwards A. Elwyn G. (2014). Power imbalance prevents shared decision making. British Medical Journal, 348, g3178. 10.1136/bmj.g3178 [DOI] [PubMed] [Google Scholar]
- Joseph-Williams N. Elwyn G. Edwards A. (2014). Knowledge is not power for patients: A systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Education and Counseling, 94, 291–309. 10.1016/j.pec.2013.10.031 [DOI] [PubMed] [Google Scholar]
- Kindig D. A., Panzer A. M., Nielsen-Bohlman L. (Eds). (2004). Health literacy: A prescription to end confusion. Retrieved from National Academies Press website: https://www.nap.edu/catalog/10883/health-literacy-a-prescription-to-end-confusion [PubMed]
- Krzywinski M. Altman N. (2013). Power and sample size. Nature Methods, 10, 1139–1140. 10.1038/nmeth.2738 [DOI] [Google Scholar]
- Knops A. M. Legemate D. A. Goossens A. Bossuyt P. M. Ubbink D. T. (2013). Decision aids for patients facing a surgical treatment decision: A systematic review and meta-analysis. Annals of Surgery, 257(5), 860–866. 10.1097/SLA.0b013e3182864fd6 [DOI] [PubMed] [Google Scholar]
- Knowles M. (1980). How do you get people to be self-directed learners? Training and Development Journal, 34(5), 96. [Google Scholar]
- Légaré F. Kearing S. Clay K. Gagnon S. D'Amours D. Rousseau M. O'Connor A. (2010). Are you SURE? Assessing patient decisional conflict with a 4-item screening test. Canadian Family Physician, 56(8), e308–e314. [PMC free article] [PubMed] [Google Scholar]
- Lipkus I. M. Samsa G. Rimer B. K. (2001). General performance on a numeracy scale among highly educated samples. Medical Decision Making, 21(1), 37–44. 10.1177/0272989X0102100105 [DOI] [PubMed] [Google Scholar]
- Lown B. A. Hanson J. L. Clark W. D. (2009). Mutual influence in shared decision making: A collaborative study of patients and physicians. Health Expectations, 12(2), 160–174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Makoul G. Clayman M. L. (2006). An integrative model of shared decision making in medical encounters. Patient Education and Counseling, 60(3), 301–312. 10.1016/j.pec.2005.06.010 [DOI] [PubMed] [Google Scholar]
- Manafo E. Wong S. (2012). Health literacy programs for older adults: A systematic literature review. Health Education and Research, 27(6), 947–960. 10.1093/her/cys067 [DOI] [PubMed] [Google Scholar]
- McCaffery K. Morony S. Muscat D. M. Smith S. K. Shepherd H. Dhillon H. Nutbeam D. (2016). Evaluation of an Australian health literacy training program for socially disadvantaged adults attending basic education classes: Study protocol for a cluster randomised controlled trial. BMC Public Health, 16, 454. 10.1186/s12889-016-3034-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaffery K. Morony S. Muscat D. M. Hayen A. Shepherd H. Dhillon H. Nutbeam D. (2019). Evaluation of an Australian health literacy program delivered in adult education settings. Health Literacy Research and Practice, 3(Suppl.), s42–s57. 10.3928/24748307-20190402-01 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat D. M. Morony S. Shepherd H. L. Smith S. K. Dhillon H. M. Trevena L. McCaffery K. (2015). Development and field testing of a consumer shared decision-making training program for adults with low literacy. Patient Education and Counseling, 98, 1180–1188. 10.1016/j.pec.2015.07.023 [DOI] [PubMed] [Google Scholar]
- Muscat D. M. Morony S. Smith S. K. Shepherd H. L. Dhillon H. Hayen A. McCaffery K. J. (2017). Qualitative insights into the experience of teaching shared decision-making within adult education health literacy programs for lower-literacy learners. Health Expectations, 20(6), 1393–1400. 10.1111/hex.12580 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat D. M. Shepherd H. L. Nutbeam D. Morony S. Smith S. K. Dhillon H. McCaffery K. J. (2017). Developing verbal health literacy with adult learners through training in shared decision making. HLRP: Health Literacy Research and Practice, 1(4), e257–e268. 10.3928/24748307-20171208-02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscat D. Smith S. Dhillon H. Morony S. Davies E. Luxford K. McCaffery K. (2016). Incorporating health literacy in education for socially disadvantaged adults: An Australian feasibility study. International Journal for Equity in Health, 15, 84. 10.1186/s12939-016-0373-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutbeam D. (1998). Health promotion glossary. Health Promotion International, 13, 349–364. 10.1093/heapro/13.4.349 [DOI] [Google Scholar]
- Nutbeam D. (2000). Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International, 15(3), 259–267. 10.1093/heapro/15.3.259 [DOI] [Google Scholar]
- Nutbeam D. (2008). The evolving concept of health literacy. Social Science and Medicine, 67(12), 2072–2078. 10.1016/j.socscimed.2008.09.050 [DOI] [PubMed] [Google Scholar]
- Parikh N. S. Parker R. M. Nurss J. R. Baker D. W. Williams M. V. (1996). Shame and health literacy: The unspoken connection. Patient Education and Counseling, 27(1), 33–39. 10.1016/0738-3991(95)00787-3 [DOI] [PubMed] [Google Scholar]
- Rowlands G. Nutbeam D. (2013). Health literacy and the ‘inverse information law’. British Journal of General Practice, 63(608), 120–121. 10.3399/bjgp13X664081 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Seo J. Goodman M. S. Politi M. Blanchard M. Kaphingst K. A. (2016). Effect of health literacy on decision-making preferences among medically underserved patients. Medical Decision Making, 36(4):550–556. 10.1177/0272989X16632197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd H. L. Barratt A. Jones A. Bateson D. Carey K. Trevena L. J. Weisberg E. (2016). Can consumers learn to ask three questions to improve shared decision making? A feasibility study of the ASK (AskShareKnow) patient-clinician communication model intervention in a primary health-care setting. Health Expectations, 19(5), 1160–1168. 10.1111/hex.12409 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shepherd H. L. Barratt A. Trevena L. J. McGeechan K. Carey K. Epstein R. M. Tattersall M. H. N. (2011). Three questions that patients can ask to improve the quality of information physicians give about treatment options: A cross-over trial. Patient Education and Counseling, 84(3), 379–385. 10.1016/j.pec.2011.07.022 [DOI] [PubMed] [Google Scholar]
- Sheridan S. L. Halpern D. J. Viera A. J. Berkman N. D. Donahue K. E. Crotty K. (2011). Interventions for individuals with low health literacy: A systematic review. Journal of Health Communication, 16(Suppl. 3), 30–54. 10.1080/10810730.2011.604391 [DOI] [PubMed] [Google Scholar]
- Smith S. Nutbeam D. McCaffery K. (2013). Insights into the concept and measurement of health literacy from a study of shared decision-making in a low literacy population. Journal of Health Psychology, 18(8), 1011–1022. 10.1177/1359105312468192 [DOI] [PubMed] [Google Scholar]
- Solari A. Giordano A. Kasper J. Drulovic J. Nunen A. V. Vahter L. Hessen C. (2013). Role preferences of people with multiple sclerosis: Image-revised, computerized self-administered version of the Control Preference Scale. PLoS One, 8(6), e66127. 10.1371/journal.pone.0066127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stacey D. Légaré F. Lewis K. Barry M. J. Bennett C. L Eden K. B. Trevena L. (2017). Decision aids for people facing health treatment or screening decisions. Cochrane Database of Systematic Reviews, 2017, 4, CD001431. 10.1002/14651858.CD001431.pub5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavistock Institute and Shared Intelligence. (2008). Evaluation of the second phase of the Skilled for Health programme. Retrieved from http://www.tavinstitute.org/projects/report-evaluation-of-phase-two-of-the-skilled-for-health-programme/
- Tiedeman D. Knowles M. (1979). The adult learner: A neglected species. Educational Researcher, 8(3), 20–22. 10.2307/1174362 [DOI] [Google Scholar]
- Towle A. Godolphin W. (1999). Framework for teaching and learning informed shared decision making. British Medical Journal, 319(7212), 766–771. 10.1136/bmj.319.7212.766 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yudkowsky R. Downing S. M. Popescu M. (2008). Setting standards for performance tests: A pilot study of a three-level Angoff method. Acad Med, 83(Suppl. 10), S13–S16. 10.1097/ACM.0b013e318183c683 [DOI] [PubMed] [Google Scholar]