Abstract
Introduction:
Child nutrition status is very important in all societies, which is influenced by the interaction of multiple factors including food security and socioeconomic status in both genders. The aim of this study was to examine the relationship between food security and socioeconomic status with anthropometric indices among 2–5-year-old urban children in eight different cities in Iran.
Materials and Methods:
In this cross-sectional study, anthropometric Z scores of 7028 children of urban area were measured by using World Health Organization (WHO) Anthro software based on WHO 2007 standards. Family food security was assessed by using HFIAS 9-item questionnaire. Socioeconomic status as well as health factors were analyzed using the SPSS.
Results:
Based on the present study, significant correlation was observed between sleep time, birth weight, and food security (P < 0.05) with body mass index (BMI), while the rest of the variables including age, family size, number of children, parents’ education, breastfeeding duration, watching TV, playing computer games, playing outdoors, number of main eating, and number of snacks showed no significant relation (P > 0.05).
Conclusion:
It was shown that 2–5 years old children's life are the most vital and vulnerable to the hazards of undernutrition or overweight and obesity, which could affect the whole health of the person. As food security affects BMI, it is important to focus more on this issue in order to improve child's health status.
Keywords: Body mass index, malnutrition, obesity, overweight, thinness
Introduction
Obesity has become one of the major risk factors for many chronic diseases, which makes it as foremost epidemiologic challenges of today around the world. Numerous comorbid conditions have been connected with obesity, including type 2 diabetes, hypertension, hyperlipidemia, and non-alcoholic fatty liver disease.[1] According to the World Health Organization (WHO), among children younger than 5 years of age, 41 million were obese or overweight in 2017, and if the present trend remains unchanged the number of overweight or obese infants and young children globally will increase to 70 million by 2025.[2] In Iran, based on the National Integrated Micronutrient Survey 2012 (NIMS-2), overweight and obesity among 15–23 months and 6 years old children are 5.6% and 13.5%, respectively. Moreover, in some regions like Gilan and Mazandaran, the north of Iran, the rate of obesity and overweight is much higher than national average.[3] There is much evidence showing that the incidence of obesity and overweight has been significantly enlarged among children in recent years. Overweight or obese children are at risk for high blood pressure, dyslipidemia, and type 2 diabetes and may become overweight or obese adults at the end.[4]
Many factors could be involved in child's weight status. Among these factors, food security is quite interesting issues these days, which might affect as a double sword on child's body mass index (BMI).[5,6] Food security is the product of food availability, food access, stability of supplies, and biological utilization.[7] In a very basic meaning it is regularly having enough food to eat for all time.[8] It could also be affected by socioeconomic status.[9] Due to worldwide studies, food security has a strong connection with human health especially among children and could affect anthropometrical indices.[10,11]
The aim of this study was to examine the relationship between food security and socioeconomic status with anthropometric indices among 2–5-year-old urban children in eight different cities in Iran.
Materials and Methods
After getting approval from the ethical committee, in a cross-sectional study data of 7028 children aged 2–5 years from eight different cities of Iran was gathered through healthcare centers. The sampling method was randomized cluster sampling, and 47 clusters and 15 sub clusters in each cluster were studied. After briefing and training sessions for the questioning teams and checking for their activities accuracy, the team addresses were announced to the members. Later by finding each cluster, the child was studied after having the consent of the mother. After filling the consent form by the mothers, the questionnaires including general information, socioeconomic status, food security, physical activity, and child feeding were completed. A comprehensive questionnaire is used for determining socioeconomic status, physical activities, and child feeding. The questions included were family size, parents’ job and education, the gender of the head of family, playing time of child in the yard or street around his/her, child TV hours, child playing computer hours, child sleeping hours, the duration of child breastfeeding, the number of child feeding meals and snacks, eating child breakfast, mothers perception on child's weight, child physical activity, and chubby child. Food security status was performed based of Iranian Household Food Insecurity Access Scale (HFIAS).[12] The HFIAS is a national food security tool for determining food insecurity in some countries. It includes nine questions for distinguishing food security status among families that adapted for Iranian people. The weight and height of the child were measured using standard methods. Weight and height of all registered kids were measured. The weight was measured using the Seca weighing scale to the nearest 0.1 kg. The height was measured using the Seca Bodymeter to the nearest 0.1 cm in order to find the relationship between food security and anthropometric indices, Z score of these indices, including weight-for-age (WAZ), height-for-age (HAZ), and BMI for age (BAZ) were calculated using Anthro V.3.2.4 software of the WHO. All the results were categorized based on WHO child growth standards guideline.[13]
Statistical analysis
Data were expressed as means ± SD and frequencies, using IBM SPSS Statistics Software (V.24, Chicago, IL, USA). Normality of all the results was tested by the Kolmogorov–Smirnov test. Statistical differences between genders were determined using independent sample t-test and Mann–Whitney U test based on the data. Correlation between factors was tested by using Pearson and Spearman Rho regarding quantitative or qualitative variables. Multiple regression was also analyzed in order to find better conclusion on associated factors to BMI among children. Statistical differences of anthropometric indices between food security groups were determined using one-way repeated measures analysis of variance (ANOVA) followed by Tukey's multiple comparison test. Differences between groups were considered significantly different when the P- value was <0.05.
Results
As Table 1 shows, significant differences were revealed on anthropometric indices between different levels of food security in children. As it illustrated, secured groups had much better healthy indices as compared to mild, moderate, and severe unsecured group. Moreover, it was found that boys as compared to the girls have anthropometric indices except in HAZ index. As Table 2 shows, no significant difference was observed on mother's perception on child activity (P = 0.130), eating breakfast (P = 0.132), number of main food (P = 0.202), number of snacks (P = 0.643), body weight of their children (P = 0.447), and their idea on chubby child (P = 0.609) between genders. No differences were observed on food security between genders as well and about 70% of children were food secure and about 9% in both genders were insecure [Figure 1]. As Table 3 shows, there was a significant difference in playing computer games, outdoor play time, sleep time, birth weight, present weight, height, BMI, WAZ, HAZ, BAZ, and weight-for-height among genders (P < 0.01). The other components did not show any significant difference between the genders (P > 0.05). As Figures 2 and 3 illustrated, the slope of BAZ and HAZ curves in both sexes indicating a shortage relative proportions to the WHO standard.
Table 1.
Comparison of the anthropometric indices based on food security between girls and boys
| Index | Severe insecure | Moderate insecure | Mild insecure | Secure | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Girls | Boys | p | Total | Girls | Boys | p | Total | Girls | Boys | p | Total | Girls | Boys | p | Total | |
| BMI | 15.15±1.89 | 15.44±2.09 | 0.06 | 15.30±2.00a | 15.05±1.76 | 15.42±1.66 | 0.002* | 15.25±1.71a | 15.03±1.60 | 15.52±1.71 | 0.001* | 15.30±1.68a | 15.34±1.80 | 15.67±1.86 | 0.001* | 15.51±1.84b |
| WAZ | -0.51±1.13 | -0.42±1.20 | 0.33 | -0.46±1.16a | -0.42±1.01 | -0.37±1.07 | 0.55 | -0.39±1.04a | -0.52±1.01 | -0.24±1.16 | 0.03* | -0.37±1.10a | -0.23±1.10 | -0.10±1.17 | 0.001* | -0.16±1.14b |
| HAZ | -0.54±1.25 | -0.49±1.35 | 0.60 | -0.52±1.30a | -0.33±1.18 | -0.41±1.32 | 0.37 | -0.37±1.26a | -0.50±1.31 | -0.31±1.36 | 0.09 | -0.40±1.34a | -0.28±1.35 | -0.20±1.37 | 0.02* | -0.24±1.36b |
| BAZ | -0.29±1.37 | -0.15±1.57 | 0.22 | -0.22±1.47a | -0.34±1.26 | -0.18±1.31 | 0.07 | -0.25±1.29a | -0.37±1.19 | -0.07±1.28 | 0.004* | -0.21±1.25a | -0.17±1.24 | 0.01±1.36 | 0.001* | -0.08±1.30b |
| WHZ | -0.29±1.32 | -0.21±1.51 | 0.45 | -0.25±1.42a | -0.35±1.24 | -0.22±1.25 | 0.12 | -0.28±1.24a | -0.37±1.18 | -0.10±1.26 | 0.009* | -0.22±1.23ab | -0.15±1.24 | -0.01±1.34 | 0.001* | -0.08±1.29b |
*abValues in the same column with different superscripts are significantly different at P<0.05 based on one-way ANOVA and Tukey’s comparison multiple post-hoc test
Table 2.
Mother’s idea about eating and activity of their children
| Variable | Boys (n=3674) | Girls (n=3354) | Total (n=7028) | p |
|---|---|---|---|---|
| Overeating foods | ||||
| Over eating | 206 (5.6) | 143 (4.3) | 349 (5.0) | 0.016* |
| Normal eating | 3453 (94.0) | 3199 (95.4) | 6652 (94.6) | |
| Not sure | 15 (0.4) | 12 (0.4) | 27 (0.4) | |
| Picky eating | ||||
| Yes | 1764 (48.0) | 1570 (46.8) | 3334 (47.4) | 0.360 |
| No | 1897 (51.6) | 1779 (53.0) | 3676 (52.3) | |
| Not sure | 13 (0.4) | 5 (0.1) | 18 (0.3) | |
| Child activity | ||||
| Low | 168 (4.6) | 180 (5.4) | 348 (5.0) | 0.130 |
| Normal | 3498 (95.2) | 3167 (94.4) | 6665 (94.8) | |
| Not sure | 8 (0.2) | 7 (0.2) | 15 (0.2) | |
| Eating breakfast | ||||
| Regular | 2879 (78.4) | 2578 (76.9) | 5457 (77.6) | 0.132 |
| Irregular | 795 (21.6) | 776 (23.1) | 1571 (22.4) | |
| Number of main food (n) | ||||
| 1 | 18 (0.5) | 33 (1.0) | 51 (0.7) | 0.202 |
| 2 | 571 (15.5) | 543 (16.2) | 1114 (15.9) | |
| 3 | 2961 (80.6) | 2667 (79.5) | 5628 (80.1) | |
| 4 | 96 (2.6) | 77 (2.3) | 173 (2.5) | |
| 5 | 28 (0.8) | 34 (1.0) | 62 (0.9) | |
| Number of snacks (n) | ||||
| 0 | 155 (4.2) | 115 (3.4) | 270 (3.8) | 0.643 |
| 1 | 801 (21.8) | 781 (23.3) | 1582 (22.5) | |
| 2 | 1890 (51.4) | 1710 (51.0) | 3600 (51.2) | |
| 3 | 578 (15.7) | 535 (16.0) | 1113 (15.8) | |
| 4 | 150 (4.1) | 141 (4.2) | 291 (4.1) | |
| 5 | 100 (2.7) | 72 (2.1) | 172 (2.4) | |
| Mother’s perception of her child weight status | ||||
| He/she is thin | 1218 (33.2) | 1144 (34.1) | 2362 (33.6) | 0.447 |
| He/she is normal | 2363 (64.3) | 2122 (63.3) | 4485 (63.8) | |
| He/she is overweight | 44 (1.2) | 49 (1.5) | 93 (1.3) | |
| He/she is obese | 19 (0.5) | 20 (0.6) | 39 (0.6) | |
| Not sure | 30 (0.8) | 19 (0.6) | 49 (0.7) | |
| Mother’s idea on chubby child | ||||
| It is sign of health | 122 (3.3) | 98 (2.9) | 220 (3.1) | 0.609 |
| It is not sign of health | 3507 (95.5) | 3220 (96.0) | 6727 (95.7) | |
| Not sure | 45 (1.2) | 36 (1.1) | 81 (1.2) |
*Based on Mann–Whitney U test.
Figure 1.
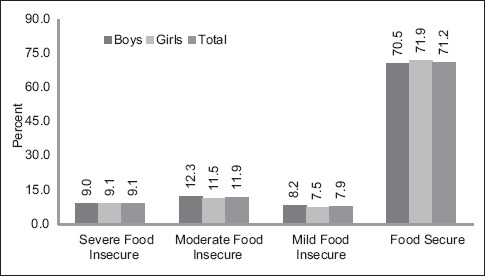
Gender-based comparison of food security among children
Table 3.
Comparison of influenced factors on BMI between girls and boys
| Boys (n=3674) | Girls (n=3354) | Total (n=7028) | p | |
|---|---|---|---|---|
| Age | 41.72±10.16 | 41.96±10.36 | 41.83±10.25 | 0.334 |
| Breastfeeding duration (month) | 19.67±9.13 | 19.57±8.58 | 19.62±8.87 | 0.656 |
| Watching TV (min) | 135.18±101.81 | 132.81±99.45 | 134.05±100.69 | 0.326 |
| Playing computer games (min) | 38.95±64.35 | 33.72±59.21 | 36.45±62.00 | 0.001* |
| Playing outdoors (min) | 142.94±121.48 | 127.08±114.63 | 135.37±118.52 | 0.001* |
| Sleep time (hours) | 10.89±1.57 | 10.96±1.52 | 10.92±1.55 | 0.074 |
| Birth weight (kg) | 3.26±0.54 | 3.16±0.52 | 3.22±0.53 | 0.001* |
| Present weight (kg) | 15.10±2.85 | 14.44±2.69 | 14.79±2.79 | 0.001* |
| Height | 98.22±7.89 | 97.13±7.73 | 97.70±7.83 | 0.001* |
| BMI | 15.61±1.85 | 15.26±1.79 | 15.44±1.83 | 0.001* |
| Weight-for-age | −0.17±1.17 | −0.30±1.09 | −0.23±1.13 | 0.001* |
| Height-for-age | −0.26±1.36 | −0.33±1.32 | −0.29±1.34 | 0.030* |
| BMI-for-age | −0.04±1.37 | −0.22±1.25 | −0.12±1.32 | 0.001* |
| Weight-for-height | −0.06±1.34 | −0.20±1.24 | −0.13±1.30 | 0.001* |
*Based on independent sample t-test.
Figure 2.
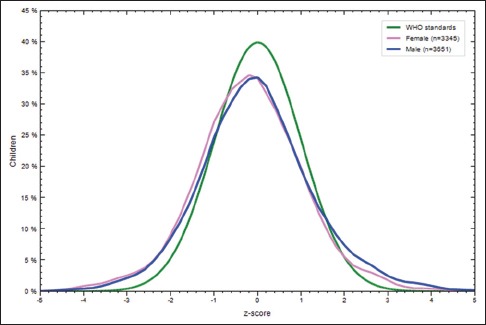
Gender-based comparison of BAZ Z-score with WHO standard
Figure 3.
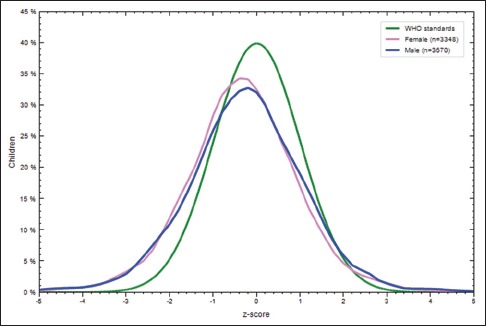
Gender-based comparison of HAZ Z-score with WHO standard
As Table 4 demonstrates, significant correlation was observed between sleep time, birth weight, and food security (P < 0.05), while the rest of the variables including age, family size, number of children, parents’ education, playing computer games, and playing outdoors showed no significant relation (P > 0.05).
Table 4.
Comparison of the correlation/regression of BMI and affected factors between girls and boys
| Variables | Unstandardized coefficients | Standardized coefficients | t | R | Sig. | Correlations | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | Beta | Zero-order | Partial | |||||||||||
| Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | Boys | Girls | |
| Age | 0.002 | 0.0001 | 0.031 | 0.0001 | 1.827 | −0.021 | 0.036 | 0.005 | 0.068 | 0.983 | 0.036 | 0.005 | 0.030 | 0.0001 |
| Family size | −0.016 | −0.017 | −0.025 | −0.029 | −1.405 | −1.587 | 0.021 | 0.031 | 0.160 | 0.113 | −0.022 | −0.031 | −0.023 | −0.027 |
| Number of children | 0.011 | 0.024 | 0.006 | 0.014 | 0.338 | 0.784 | 0.009 | 0.007 | 0.736 | 0.433 | −0.009 | −0.007 | 0.006 | 0.014 |
| Mother education | −0.002 | 0.009 | −0.005 | 0.027 | −0.246 | 1.208 | 0.008 | 0.015 | 0.806 | 0.227 | 0.011 | 0.035 | −0.004 | 0.021 |
| Father education | 0.004 | -0.003 | 0.009 | −0.009 | 0.454 | −0.432 | 0.018 | 0.005 | 0.650 | 0.666 | 0.016 | 0.018 | 0.008 | −0.007 |
| Breastfeeding Duration (month) | −0.002 | −0.001 | −0.037 | −0.023 | −2.204 | −1.319 | 0.024 | 0.011 | 0.028 | 0.187 | −0.024 | −0.011 | −0.036 | −0.023 |
| Watching TV (min) | 0.0001 | 0.0001 | 0.0001 | −0.003 | 0.0001 | −0.186 | 0.014 | 0.005 | 1.000 | 0.852 | 0.014 | 0.005 | 0.000 | −0.003 |
| Playing computer games (min) | 0.0001 | 0.0001 | 0.023 | 0.025 | 1.376 | 1.423 | 0.034 | 0.030 | 0.169 | 0.155 | 0.034 | 0.030 | 0.023 | 0.025 |
| Playing outdoors (min) | 0.0001 | 0.0001 | 0.023 | 0.017 | 1.339 | 0.979 | 0.025 | 0.018 | 0.181 | 0.328 | 0.025 | 0.018 | 0.022 | 0.017 |
| Sleep time (hours) | −0.007 | −0.018 | −0.019 | −0.056 | −1.109 | −3.182 | 0.022 | 0.054 | 0.268 | 0.001* | −0.022 | −0.054 | −0.018 | −0.055 |
| Birth weight (kg) | 0.093 | 0.095 | 0.091 | 0.103 | 5.384 | 5.828 | 0.085 | 0.099 | 0.0001* | 0.0001* | 0.086 | 0.099 | 0.089 | 0.100 |
| Number of main eating | 0.002 | 0.013 | 0.002 | 0.013 | 0.122 | 0.742 | 0.004 | 0.007 | 0.903 | 0.458 | −0.004 | 0.007 | 0.002 | 0.013 |
| Number of snacks | 0.020 | 0.005 | 0.035 | 0.011 | 2.096 | 0.608 | 0.039 | 0.016 | 0.036* | 0.543 | 0.039 | 0.016 | 0.035 | 0.011 |
| Food security | 0.018 | 0.020 | 0.034 | 0.042 | 2.047 | 2.405 | 0.034 | 0.042 | 0.041* | 0.016* | 0.034 | 0.042 | 0.034 | 0.042 |
*Correlation analysis based on Pearson and Spearman Rho regarding quantitative or qualitative variables. R was calculated using multiple regression test.
Discussion
The present study revealed, food security has significant effect on both genders. Food security as one of the main key factor has an important role in both children and adult health. It is strongly related to household income and can affect both physical and mental health of family.[14] Previous studies showed that one of the main food insecurity consequences is its effects on anthropometrical indices of children,[15] which is also noted in the present study as well. Along with previous studies, in the present study it showed, child's BMI had positive correlation with household food security status.[16,17,18] Unfortunately, food insecurity works as a double blade sword. It not only can decelerate height of children, but also can increase their weight in a noteworthy proportion of preschool-aged children as the literature has explored.[15] Even though the present study showed about 70% food security among studied population, some important factors should be noted. First of all, food security questionnaire has many challenges which under/over reporting is one of the common problem.[19] For example, some over reporting might exist due to Persians’ family pride, which is related to Iranian culture.[20] Therefore, it is good to note these facts to have better conclusion.
Nutritionally-related health patterns in the Middle East have changed significantly during the last two decades. These changes are mirrored in nutritional and health upshots. Rising obesity rates and high levels of chronic and degenerative diseases are observed. While several countries of the region have obesity rates exceeding 30%, rates of undernutrition, particularly stunting, among under-five children in low- and middle-income countries remain high.[21] The present study, likewise global data, stunting was the major risk. Payandeh et al.[22] found high risk of stunting in Iranian children. Prevalence estimations for stunting and overweight are relatively robust. It is, therefore, possible to track global and regional changes in these two conditions over time.[23] A key indicator of chronic malnutrition is stunting based on the WHO child growth standards. Weight and height both reflect the size of the individual. However, weight by itself is a poor indicator of thinness or obesity. Moreover, despite the benefits of BMI in this issue, due to the effect of height on BAZ of children, reports about obesity and overweight could be a false alarm in some of studies due to low HAZ. Even in normal WAZ for children, low HAZ lead to higher BAZ.
Concerning the differences between mothers’ belief on their child nibbling, it should be noted that in traditional communities still we could see parents treat boys and girls differently which might explain this result as it was seen in previous studies as well which follows gender schema theories.[24,25,26,27,28] Even though about 53% of mothers of the girls believe that their daughter has nibbling, while 51% of boys’ mothers have similar idea, no significant difference was observed. This finding was similar to the Southampton Women's Survey (SWS) as one of the largest study in this area.[29] Moreover, this fact should not be forgotten that many studies confirmed that many parents did not even identify that their children were overweight and, as shown in other studies, tended to be unconcerned about the issue.[30,31] A parent's awareness about their child's overweight status is a chief herald or determinant of preventative actions. Acknowledgment of and fear for, overweight may be vapid by the parent's own weight status, whereas engaging in healthy behaviors at home may promote healthy weight status.[32]
In conclusion, it should be noted that preschool children are most vital and vulnerable to the hazards of undernutrition or overweight and obesity, which could affect the whole health of the person. All efforts should be prepared so that preschool children are given a balanced and nutritious home-based diet.[33]
Conclusion
As food security affects children's BMI, and 2–5 years old children's life are the most vital and susceptible to the threats of undernutrition or overweight and obesity, which could affect the whole health of the person., in order to improve child's health status and community health, it is essential to focus more on this issue.
Financial support and sponsorship
Nutrition Community Department of Ministry of Health and Medical Education.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors wish to thank Ministry of Health and all parents who joined in the present study.
References
- 1.Hurt RT, Kulisek C, Buchanan LA, McClave SA. The obesity epidemic: Challenges, health initiatives, and implications for gastroenterologists. Gastroenterol Hepatol. 2010;6:780–92. [PMC free article] [PubMed] [Google Scholar]
- 2.WHO. Facts and figures on childhood obesity. World Health Organisation. World Health Organization. 2017 [Google Scholar]
- 3.Siassi F. 1st ed. Tehran: Andisheh Mandegar; 2016. National Integrated Micronutrient Survey 2012 (NIMS-2) pp. 1–254. [Google Scholar]
- 4.Kelishadi R, Cook SR, Amra B, Adibi A. Factors associated with insulin resistance and non-alcoholic fatty liver disease among youths. Atherosclerosis. 2009;204:538–43. doi: 10.1016/j.atherosclerosis.2008.09.034. [DOI] [PubMed] [Google Scholar]
- 5.Franklin B, Jones A, Love D, Puckett S, Macklin J, White-Means S. Exploring mediators of food insecurity and obesity: A review of recent literature. J Community Health. 2012;37:253–64. doi: 10.1007/s10900-011-9420-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Troy LM, Miller EA, Olson S. The National Acadamies Press. US: National Academies Press; 2011. Socioeconomic Disparities: Food Insecurity and Obesity; pp. 3–50. [Google Scholar]
- 7.FAO. The state of food insecurity in the world 2001. 1st ed. Rome, Italy: Food and Agriculture Organization of the United Nations; 2001. p. 58. [Google Scholar]
- 8.Gibson M. Food Security—A Commentary: What Is It and Why Is It So Complicated? Foods. 2012;1:18–27. doi: 10.3390/foods1010018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sarki M, Robertson A, Parlesak A. Association between socioeconomic status of mothers, food security, food safety practices and the double burden of malnutrition in the Lalitpur district, Nepal. Arch Public Health. 2016;74:35. doi: 10.1186/s13690-016-0150-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Humphries DL, Dearden KA, Crookston BT, Fernald LC, Stein AD, Woldehanna T, et al. Cross-Sectional and Longitudinal Associations between Household Food Security and Child Anthropometry at Ages 5 and 8 Years in. J Nutr. 2015;145:1924–33. doi: 10.3945/jn.115.210229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mukhopadhyay DK, Biswas AB. Food security and anthropometric failure among tribal children in Bankura, West Bengal. Indian Pediatr. 2011;48:311–4. doi: 10.1007/s13312-011-0057-2. [DOI] [PubMed] [Google Scholar]
- 12.Mohammadi F, Omidvar N, Houshiar-Rad A, Khoshfetrat M-R, Abdollahi M, Mehrabi Y. Validity of an adapted Household Food Insecurity Access Scale in urban households in Iran. Public Health Nutr. 2012;15:149–57. doi: 10.1017/S1368980011001376. [DOI] [PubMed] [Google Scholar]
- 13.World Health Organization, United Nations Childrens Fund. WHO child growth standards and the identification of severe acute malnutrition in infants and children. [Last retrieved on 2018 April 12];World Heal Organ. 2009 11 Available from: http://apps.who.int/iris/bitstream/10665/44129/1/9789241598163_eng.pdf . [PubMed] [Google Scholar]
- 14.Friel S, Berry H, Dinh H, O’Brien L, Walls HL. The impact of drought on the association between food security and mental health in a nationally representative Australian sample. BMC Public Health. 2014;14:1102. doi: 10.1186/1471-2458-14-1102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Speirs KE, Fiese BH STRONG Kids Research Team. The Relationship Between Food Insecurity and BMI for Preschool Children. Matern Child Health J. 2016;20:925–33. doi: 10.1007/s10995-015-1881-0. [DOI] [PubMed] [Google Scholar]
- 16.Ebrahimzadehkor B, Kalantari N, Abadi A, Kabir M. Nutritional Status and Related Factors in Children, Bandar Turkmen District, Iran. Zahedan J Res Med Sci. 2014;16:29–33. [Google Scholar]
- 17.Sheykhi M, Eftekhari Nia M, Hadipour M, Esmaillzadeh A. Prevalence of Stunting, Underweight and Wasting According to National Center for Health Statistics Criteria in Rural Children Aged under Six Years in Zahedan, Iran, in 2010. J Heal Syst Res. 2013;9:153–8. [Google Scholar]
- 18.Houshiar Rad A, Dorosty Motlagh A, Kalantari N, Abdollahi M, Abtahi M. The prevalence of stunting, underweight, wasting and overweight among children under five years of Iran (2000-2002) Nutr Sci Food Ind Iran. 2008;3:49–56. [Google Scholar]
- 19.Frongillo EA, Chowdhury N, Ekströ E-C, Naved RT. Community and International Nutrition Understanding the Experience of Household Food Insecurity in Rural Bangladesh Leads to a Measure Different from That Used in Other Countries. J Nutr. 2003;133:4158–62. doi: 10.1093/jn/133.12.4158. [DOI] [PubMed] [Google Scholar]
- 20.IES. Cultural Atlas - Iranian Culture. Cultural Atlas. 2018. [Last accessed on 2018 Jun 5]. Available from: https://culturalatlas.sbs.com.au/iranian-culture/core-concepts-9b3009e7-06a2-488e-8020-cfcf906fd10c .
- 21.Rahim HFA, Sibai A, Khader Y, Hwalla N, Fadhil I, Alsiyabi H, et al. Non-communicable diseases in the Arab world. Lancet (London, England) 2014;383:356–67. doi: 10.1016/S0140-6736(13)62383-1. [DOI] [PubMed] [Google Scholar]
- 22.Payandeh A, Saki A, Safarian M, Tabesh H, Siadat Z. Prevalence of Malnutrition among Preschool Children in Northeast of Iran, A Result of a Population Based Study. Glob J Health Sci. 2013;5:208–12. doi: 10.5539/gjhs.v5n2p208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Unicef, WHO, Bank TW. Levels and Trends in Child malnutrition. Midwifery. 2014;4 [Google Scholar]
- 24.Bem SL. Gender schema theory: A cognitive account of sex typing. Psychol Rev. 1981;88:354–64. [Google Scholar]
- 25.Zahn-Waxler C, Shirtcliff EA, Marceau K. Disorders of childhood and adolescence: Gender and psychopathology. Annu Rev Clin Psychol. 2008;4:275–303. doi: 10.1146/annurev.clinpsy.3.022806.091358. [DOI] [PubMed] [Google Scholar]
- 26.Black SE, Devereux PJ, Salvanes KG. The More the Merrier? The Effect of Family Size and Birth Order on Children's Education. Q J Econ. 2005;120:669–700. [Google Scholar]
- 27.Endendijk JJ, Groeneveld MG, Bakermans-Kranenburg MJ, Mesman J. Gender-Differentiated Parenting Revisited: Meta-Analysis Reveals Very Few Differences in Parental Control of Boys and Girls. PLoS One. 2016;11:e0159193. doi: 10.1371/journal.pone.0159193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.He M, Evans A. Are parents aware that their children are overweight or obese? Do they care? Can Fam Physician. 2007;53:1493–9. [PMC free article] [PubMed] [Google Scholar]
- 29.Inskip HM, Godfrey KM, Robinson SM, Law CM, Barker DJP, Cooper C SWS Study Group. Cohort profile: The Southampton Women's Survey. Int J Epidemiol. 2006;35:42–8. doi: 10.1093/ije/dyi202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Eckstein KC. Parents’ Perceptions of Their Child's Weight and Health. Pediatrics. 2006;117:681–90. doi: 10.1542/peds.2005-0910. [DOI] [PubMed] [Google Scholar]
- 31.Jeffery AN, Voss LD, Metcalf BS, Alba S, Wilkin TJ. Parents’ awareness of overweight in themselves and their children: Cross sectional study within a cohort (EarlyBird 21) BMJ. 2005;330:23–4. doi: 10.1136/bmj.38315.451539.F7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Peyer KL, Welk G, Bailey-Davis L, Yang S, Kim J-K. Factors associated with parent concern for child weight and parenting behaviors. Child Obes. 2015;11:269–74. doi: 10.1089/chi.2014.0111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Singh M. Role of micronutrients for physical growth and mental development. Indian J Pediatr. 2004;71:59–62. doi: 10.1007/BF02725658. [DOI] [PubMed] [Google Scholar]


