Abstract
Here, we report the diagnostic challenge of a female patient of Russian descent with autosomal recessive hypotrichosis with juvenile macular dystrophy (HJMD). She presented to dermatology age one and a half years with sparse hair growth on her scalp, her parents were reassured this would grow, but it never manifested. She was found to be hypermetropic and prescribed glasses from age 2 but no retinal findings were noted. At age 23 years, the patient undertook an internet search and discovered the association of symptoms pointing towards HJMD. She sought genetic testing, revealing a homozygous missense mutation in Cadherin-3 (CDH3) gene. The patient presented to our Genetic Eye Disease Service at Moorfields Eye Hospital age 27 years, with reduced colour, central distance and near vision. Fundus examination and imaging confirmed atrophic macular changes. Currently, HJMD has no treatment, she wears a wig, UV-protected sunglasses in sunlight and maintains a healthy balanced diet.
Keywords: dermatology, ophthalmology
Background
Hypotrichosis with juvenile macular dystrophy (HJMD, OMIM #601553) is an autosomal recessive disorder with pathognomonic features including sparse scalp hair growth from birth and progressive vision loss leading to blindness from juvenile macular dystrophy.1 HJMD is an ultra-rare condition, first described in 1935 in two sisters from Germany by Wagner. There have only been approximately 50 cases reported in the literature.2 The clinical phenotype requires cross-disciplinary input from both dermatologists and ophthalmologists, hence both specialties must be aware of this association in order to expedite a molecular diagnosis for the patient as this has implications for informed genetic counselling including family planning, and psychosocial support for dysmorphia and progressive sight loss. Mutations in the Cadherin-3 (CDH3) gene (OMIM #114021) have been found to cause this disorder.
Case presentation
At age one and a half years, the parents noticed sparse hair growth over the scalp and visited a dermatologist who diagnosed congenital hypotrichosis (but advised that the hair would grow over time). The patient first presented to the ophthalmology department at age 2 as she was experiencing difficulties with vision at nursery. She was diagnosed with hypermetropia and prescribed glasses. She was born full term with no complications and an unremarkable pregnancy. Her medical history, drug and family history were unremarkable with no consanguinity. Her full systems examination was normal except for the restricted hair growth pattern. She was followed up for several years without any further information or investigations. She had a brother 8 years younger, who developed similar signs with sparse scalp hair and reduced vision by age 6 with difficulty reading. He was prescribed glasses but these did not help and he reported progressive vision loss.
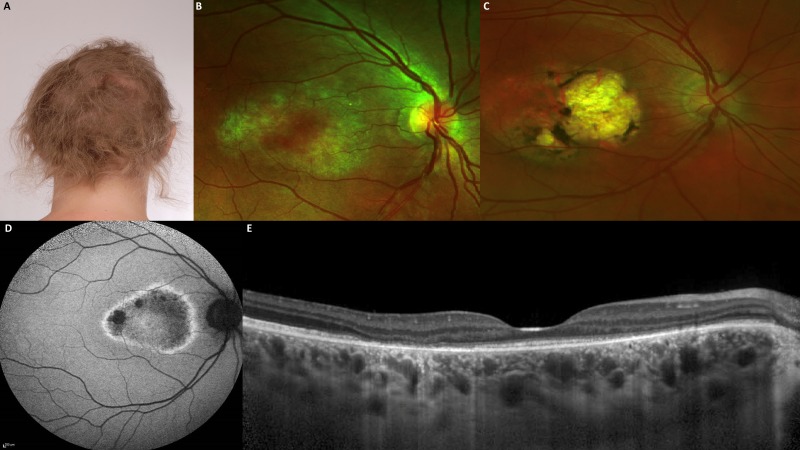
When the patient was 23 years old and her brother was 15 years old, they searched the internet to discover the association of sparse scalp hair growth and progressive vision loss leading to a diagnosis of HJMD. They contacted their clinical geneticist and requested they be screened for mutations in CDH3. This genetic testing revealed a homozygous CDH3 missense mutation c.1508G>A, p.(Arg503His). At age 27 she presented to our hospital to enquire about potential research and therapies under development for HJMD. She was wearing a hair piece to conceal her sparse hair growth (figure 1A). Her best-corrected LogMAR vision at 4 m was 0.34 in the right eye and 0.40 in the left eye, colour vision using the Ishihara chart was 4/17 in the right eye and 6/17 in the left eye, no relative afferent pupillary defect and intraocular pressure was 15 mm Hg in both eyes. Fields to confrontation revealed a large central scotoma, peripheral vision was intact. Lid and anterior segment examination was normal with a clear cornea and lens. Fundus examination showed symmetrical atrophic changes at both macula (figure 1B), with unremarkable optic discs, retinal vasculature and periphery. Her younger affected brother displayed a more severe phenotype; his vision was 0.80 in the right eye and 0.50 in the left eye using LogMAR vision at 4 m, and the macula region showed distinct chorioretinal atrophy with pigmentation (figure 1C).
Figure 1.
Features of hypotrichosis with juvenile macular dystrophy. (A) Photograph of the affected patient with sparse hair and thinning (hypotrichosis) age 27. (B) Right fundus photograph of patient showing atrophic macular changes age 27. (C) Right fundus photograph of affected brother age 20 showing severe macular chorioretinal atrophy and pigmentation. (D) Fundus autofluorescence showing retinal pigment epithelium loss at the macula with a demarcating hyperfluorescent ring around the diseased area in the right fundus. (E) Spectral-domain optical coherence tomography showing patchy loss of the outer nuclear layer, photoreceptor outer and inner segments and the retinal pigment epithelium.
Investigations
Retinal imaging was undertaken including optos colour fundus imaging, fundus autofluorescence (FAF) and spectral-domain optical coherence tomography (SD-OCT) to delineate the macular changes (figure 1). FAF showed retinal pigment epithelium (RPE) loss at the macula with a hyperfluorescent ring demarcating the diseased area (figure 1D). SD-OCT revealed patchy loss of the outer nuclear layer, photoreceptor outer and inner segments and RPE (figure 1E). Genetic diagnosis had already been established with homozygous missense mutations in CDH3, however, next-generation sequencing with retinal dystrophy clinical exome panels are mainstay.
Differential diagnosis
Mutations in CDH3 also give rise to ectodermal dysplasia (abnormal nails, missing teeth and dry skin), ectrodactyly (abnormal or missing digits) and macular dystrophy syndrome (EEMS, OMIM #225280), which is rarer than HJMD with only about 15 cases documented.3 It is characterised by hypotrichosis, dental anomalies, syndactyly or cleft hand, and atrophic and pigmentary macular changes.
Sparse scalp hair from birth heralds the first sign of HJMD, however before the onset of sight loss, causes of congenital hypotrichosis should be investigated such as hypotrichosis simplex, congenital atrichia, loose anagen syndrome, uncombable hair syndrome, ectodermal dysplasia syndromes and Marie-Unna hereditary hypotrichosis caused by mutations in U2HR and recently EPS8L3, cartilage-hair hypoplasia caused by mutations in RMRP and autosomal recessive hypotrichosis caused by mutations in the LIPH, LPAR6 or DSG4 genes.
There are no other macular dystrophies associated with hair loss, but early-onset macular dystrophies include Stargardt’s disease, Best disease or North Carolina macular dystrophy (OMIM #136550).
Treatment
No treatment is available for this condition.
Outcome and follow-up
The patient has been advised to eat a healthy balanced diet full of fruit and green leafy vegetables rich in antioxidants. She was encouraged to wear UV-protected sunglasses in bright light and use blue-light screen protectors on computer screens and smartphone devices. These patients should be offered low-vision aids and assistive digital technologies to support them with their activities of daily living at work and in the home. Twelve-month follow-up is required to monitor for disease progression. Hypotrichosis, combined with sight loss, can lead to an enormous emotional burden with low self-confidence, impaired quality of life and psychological disorders. Attention to well-being is paramount with the appropriate psychological, and genetic counselling must be offered.
Discussion
HJMD is rare with approximately 50 reported cases in the literature. It is an autosomal recessive condition caused by mutations in the CDH3 gene located on chromosome 16, encoding the transmembrane protein P-cadherin. This plays a role in tight junctions between cells with highest expression in hair follicles and the RPE, hence giving rise to the classic signs.4 HJMD has been described in families of Spanish,5 Pakistani,6 Turkish and Israeli origin,4 our family is the first reported of Russian descent.
There are hundreds of types of genetic hypotrichoses and as this is the first presenting feature in HJMD, it is important that dermatologists are aware of this association and undertake genetic testing early on to reach a definitive diagnosis in order to recruit the correct multidisciplinary team to reduce any comorbidities. The proband was wearing a wig to cover up the hypotrichosis, thus ophthalmologists must take a detailed systemic history in order to establish this key feature.
With the first approved gene therapy, Luxturna, for biallelic mutations in the RPE65 gene causing a form of Leber congenital amaurosis is available in the USA and Europe. Ophthalmology is a front runner for several clinical gene replacement and genetic therapies. Small molecule drugs, for example, ataluren, are now available to suppress nonsense mutations and there have been cases of HJMD that could benefit from this in the future. Hence the importance of reaching a molecular diagnosis and potentially instigating treatment before the sight loss advances. There is significant inter- and intra-familial variability in inherited retinal disease, this was highlighted in this family where the younger brother had more severe macular involvement and visual outcome. Early intervention, even with the use of low vision aids, can enable patients to be supported during schooling and enter into employment. This condition is progressive and wider involvement of the retina with peripheral RPE atrophy and pigmentary changes will impact on the visual field.
In summary, due to the extremely low prevalence of HJMD, accurate diagnosis remains a challenge to clinicians. Patients who present with congenital hypotrichosis should be followed up and investigated by dermatologists specialising in genetic conditions. If patients present to ophthalmology with sparse scalp hair, they should also be aware of this association and instigate referral to an ophthalmic genetic specialist or clinical genetics who can undertake timely genetic testing. More detailed ophthalmological assessment including electrophysiology with pattern electroretinograms can detect early macular changes.
Patient’s perspective.
When I was 2 years old, the ophthalmologist discovered I was long-sighted and was given glasses. Before this, my parents had noticed that my hair was short and thin and did not grow properly. They consulted a dermatologist and were reassured that the hair would still grow and not to worry. My little brother was 7 years younger but soon we could see that his hair looked like mine and grew badly. When he started school, he realised he had trouble reading and the ophthalmologist found some spots on his retina but did not know the cause. He was referred to a specialist centre and investigated for North Carolina macular dystrophy but had no genetic result. When I was 23 years old, I asked our local eye doctor to examine my retina to look for similar spots and once an OCT was done, their presence was confirmed. We visited the specialist centre again but never did a doctor make the connection between macular dystrophy and our hair growth. I decided to google the symptoms and I found the website www.hjmd.de and after reading everything, it was clear that was our diagnosis. We arranged a genetic test for ourselves and confirmed the diagnosis. Having this certainty gives me a good feeling. Sometimes I'm scared of what's coming, but I can accept it now. After the diagnosis, I decided to wear a wig, because I know that there is no way for my hair to grow. If hair growth is conspicuously reduced or absent while the child enters early nursery/school age, an eye examination should be done by an ophthalmologist. The child should always be considered holistically and different characteristics should be judged in relation to each other.
Learning points.
Hypotrichosis with juvenile macular dystrophy (HJMD) is a rare genetic disease that clinicians are unlikely to have encountered.
Patients usually initially present with sparse scalp hair (congenital hypotrichosis) from birth HJMD is a rare genetic disease that clinicians are unlikely to have encountered.
This is accompanied by decreasing visual acuity and progressive macular dystrophy within the first decade of life leading to progressive sight loss.
Genetic testing can identify the disease causing gene Cadherin-3 (CDH3).
Psychological and social support is key for these patients as no treatment currently exists.
Acknowledgments
Thank you to Dr Mariya Moosajee for her support and advice with this paper.
Footnotes
Correction notice: This article has been corrected since it was first published. The affiliation of the author "Mariya Moosajee" has been corrected.
Contributors: MM treated the patient as a clinician and was responsible for data acquisition, analysis and interpretation. AN wrote the first draft of the manuscript and MM was involved in revising and critically appraising manuscript. AN and MM were involved in the final approval for publication.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Wagner H, Maculaaffektion WH. Maculaaffektion, vergesellschaftet MIT Haarabnormität von Lanugotypus, beide vielleicht angeboren bei zwei Geschwistern. Albrecht von Græfes Archiv für Ophthalmologie 1935;134:74–81. 10.1007/BF01854763 [DOI] [Google Scholar]
- 2. Vicente LP, Finzi S, Susanna Júnior R, Susanna R, et al. Hypotrichosis with juvenile macular dystrophy: a case report with molecular study. Arq Bras Oftalmol 2017;80:49–51. 10.5935/0004-2749.20170013 [DOI] [PubMed] [Google Scholar]
- 3. Basel-Vanagaite L, Pasmanik-Chor M, Lurie R, et al. <i>CDH3</i>-Related Syndromes: Report on a New Mutation and Overview of the Genotype-Phenotype Correlations. Mol Syndromol 2011;1:223–30. 10.1159/000327156 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Halford S, Holt R, Németh AH, et al. Homozygous deletion in CDH3 and hypotrichosis with juvenile macular dystrophy. Arch Ophthal 2012;130:1490–2. 10.1001/archophthalmol.2012.708 [DOI] [PubMed] [Google Scholar]
- 5. Blanco-Kelly F, Rodrigues-Jacy da Silva L, Sanchez-Navarro I, et al. New CDH3 mutation in the first Spanish case of hypotrichosis with juvenile macular dystrophy, a case report. BMC Med Genet 2017;18:1 10.1186/s12881-016-0364-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Indelman M, Hamel CP, Bergman R, et al. Phenotypic diversity and mutation spectrum in hypotrichosis with juvenile macular dystrophy. J Invest Dermatol 2003;121:1217–20. 10.1046/j.1523-1747.2003.12550_1.x [DOI] [PubMed] [Google Scholar]