Abstract
Foreign body impaction in the oesophagus is a common cause of acute dysphagia. Oesophageal impaction of sharp objects such as dentures can be life threatening due to the risk of oesophageal perforation. This condition requires urgent treatment, and therefore prompt diagnosis and management is vital to avoid complications. Diagnosing oesophageal foreign body can be challenging due to its poor localising symptoms. We describe a case of an impacted denture in which considerable delays to treatment were encountered, and discuss the pitfalls and lessons learnt. This case and review of the literature draw attention to clinical assessment, investigation and treatment options for oesophageal foreign body impaction.
Keywords: ear, nose and throat/otolaryngology; endoscopy; oesophagus; head and neck surgery
Background
Although foreign body (FB) ingestion mainly occurs in the paediatric population between ages 6 months and 6 years, adults are also at risk.1 2 In 75% of cases of oesophageal food bolus impaction there is underlying oesophageal pathology.1The incidence of non-food FB ingestion is greater in adults with mental health disorders, learning difficulties, alcohol intoxication, prisoners, and those using dentures.1 2 Whilst the majority of ingested foreign bodies pass spontaneously, 10%–20% require intervention.1 The complications of oesophageal FB ingestion include impaction, perforation and obstruction.2
Denture ingestion has a high misdiagnosis rate of 47%.3 The published literature contains reports of patients discharged home from the emergency department (ED) with missed impacted dentures in the oropharynx and upper oesophagus.4 5 The consequences can be disastrous such as requirement for tracheostomy,5 mortality4 and litigation.3 The diagnostic difficulty may be related to unclear history from patients with sensory deficit due to neurological conditions, cognitive deficit in older people, lack of clinical signs and radiolucency of dentures. We discuss these diagnostic barriers and provide a systematic approach to assessment and management in this case report and review of the literature.
Case presentation
A man in his late 30s presented to the ED minor injuries unit at a university teaching hospital with accidental ingestion of his denture while eating. He complained of discomfort and FB sensation in his lower throat with inability to swallow any solids, managing small quantities of fluid only. He had no significant comorbidities or previous dysphagia. He was a cigarette smoker and admitted to alcohol excess. The patient was initially seen by an emergency nurse practioner and referred to the on-call ear, nose and throat (ENT) team. A full head and neck examination including nasendoscopy of the pharynx and larynx was performed by an ENT junior doctor at core surgical trainee 1 level (equivalent to senior house officer / SHO). No abnormality was identified on examination. The patient was referred and accepted by the medical team. He was booked to have a flexible oesophagogastroduodenoscopy (OGD) by the gastroenterologists.
The patient was admitted under the care of a medical team. No further ENT input occurred until 3 days into hospital admission when the ENT SHO who initially reviewed the patient in ED recognised him on the ward. The patient was still on the waiting list for an OGD. He had received supportive treatment including analgesics and intravenous fluid maintenance therapy. The patient’s OGD slot had been postponed multiple times due to other cases that were given higher priority by the gastroenterologists. On each occasion he was being starved for the procedure. During this period the patient’s temperature, pulse and respiratory rate remained within normal range. The ENT registrar (higher surgical trainee) reviewed the patient to re-evaluate the patient’s condition. The patient was symptomatic but had no signs of sepsis or perforation. Repeat nasendoscopic examination was normal. The ENT registrar attempted to expedite the OGD; however, there was no availability that day. To avoid further delay, the patient was taken to the emergency theatre.
Investigations
Plain film radiographs of his neck (figure 1), chest and abdomen were performed in ED on admission. The radiographs were unremarkable. On the second review by the ENT team after 3 days, the ENT registrar discussed the case with the on-call consultant radiologist to obtain a CT scan to confirm the site of the FB in view of the delay. The radiologist declined the request as the patient was clinically stable and he felt a CT scan would not alter the treatment plan, which consisted of endoscopic evaluation of the upper gastrointestinal tract and retrieval of the FB.
Figure 1.
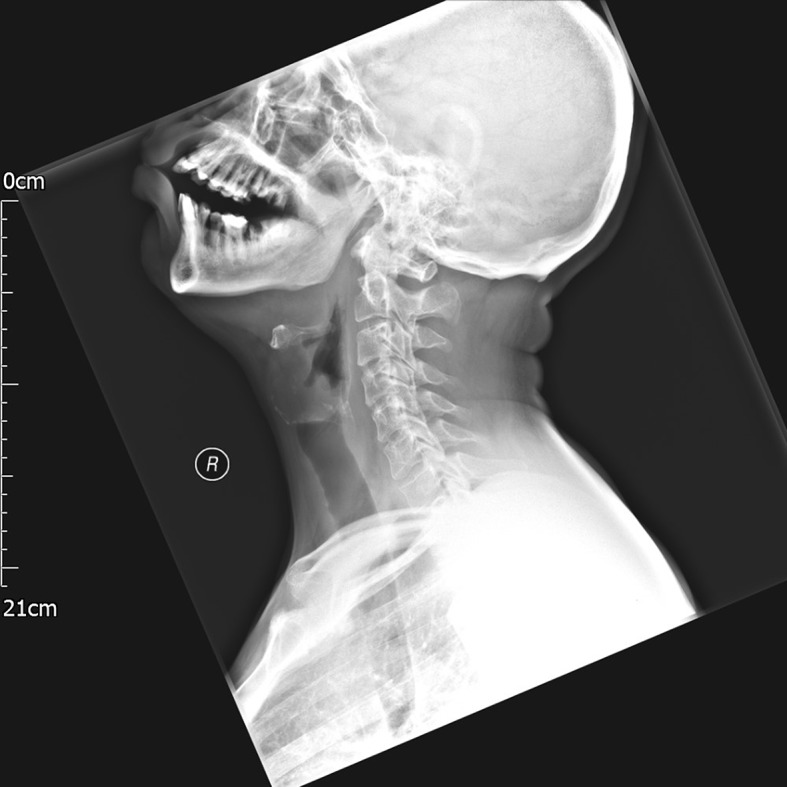
Plain radiograph lateral soft tissue neck.
Treatment
Endoscopy was performed with a 30 cm rigid oesophagoscope under general anaesthetic. A denture was found in the oesophagus at 25 cm from the upper central incisors (figure 2). The denture was obliquely impacted with surrounding mucosal oedema. The intact FB was removed cautiously with grasping forceps. As the FB exceeded the diameter of the oesophagoscope lumen, it was removed together with the oesophagoscope. The oesophagus was re-inspected and only mucosal abrasion at the site of impaction was noted.
Figure 2.
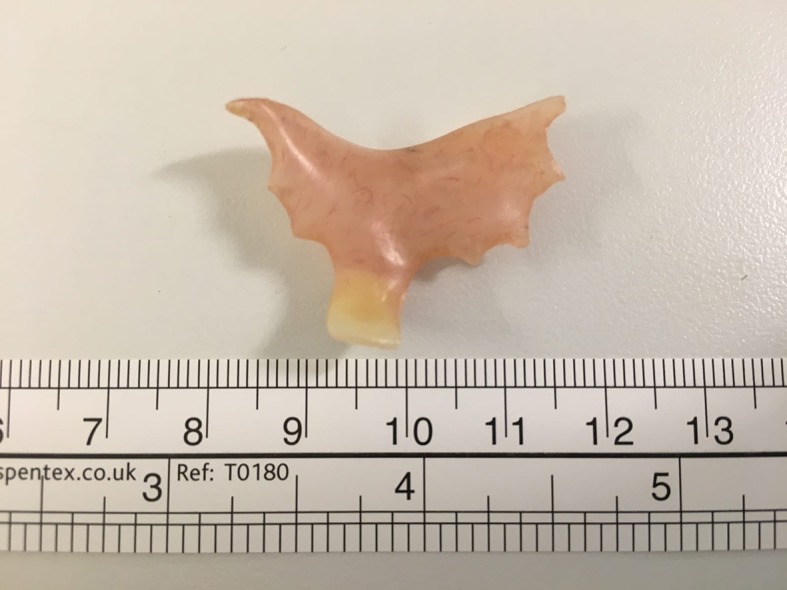
Photograph of denture removed from oesophagus.
Outcome
After a period of nil by mouth and observation, the patient returned to his normal diet the next day. The patient had an uneventful postoperative recovery and was discharged from hospital the following day after his procedure. He was advised not to use his denture until review by his dentist.
Discussion
Oesophageal foreign bodies
Obstruction tends to occur at natural constrictions, the upper oesophageal sphincter (cricopharyngeus), aortic arch, left main bronchus and lower oesophageal sphincter.1 2 The upper sphincter is the narrowest4 and is the most common site of FB impaction.6 Competent adults are usually able to give a clear history of FB ingestion and commonly complain of discomfort, dysphagia, odynophagia, retrosternal pain, sore throat, FB sensation, retching and vomiting.1 2 4 The patient’s subjective description of the level of FB sensation or discomfort can be misleading as it correlates poorly with anatomical level of impaction.1 2 Bandyopadhyay et al6 reported a series of 47 patients with upper oesophageal denture impaction and found that dysphagia and tracheal tenderness were the most consistent clinical findings. Oesophageal FB impaction can cause airway compromise by tracheal compression, progressive oedema and aspiration of saliva, and therefore patients may present with respiratory symptoms such as choking, stridor and dyspnoea.1 Signs of complications such as perforation, especially with a history of sharp or pointed FB, need to be routinely excluded by examining for neck swelling, fever, chest pain, tachycardia and subcutaneous emphysema.2 The patient in our case provided a clear account of swallowing his denture and his alcohol intoxication was a risk factor for FB ingestion. A high index of suspicion for oesophageal FB should be maintained,6 therefore the presence of persistent symptoms warrants further investigation to confirm or exclude oesophageal impaction.
Investigations
Radiographs with anterior-posterior and lateral views are useful in determining the presence, location, number, type, size and shape of foreign bodies.7 A lateral soft tissue neck radiograph is the initial investigation of choice.8 Direct and indirect signs of an FB on neck radiograph are listed in box 1.7 8 A negative neck radiograph usually requires imaging to be extended to include the chest, abdomen and pelvis, which leads to higher levels of cumulative radiation dose.9 An alternative modality is low-dose Statscan (LODOX), which is a full body X-ray scan used in polytrauma patients in some centres.9 Application of this technology in investigating FB ingestion has demonstrated higher sensitivity, specificity and visualised area, and reduced dose of radiation by up to 65% compared with conventional radiographs.9
Box 1. Signs of upper oesophageal foreign body (FB) on lateral neck radiograph.
Direct visualisation of FB.
Prevertebral soft tissue widening (more than half the width of the adjacent vertebral body at the level of C2, more than the total width of the adjacent vertebral body at the level of C7).
Loss of cervical lordosis.
Column of air in the proximal oesophagus.
Plain film radiographs have the advantage of identifying steak bones and showing signs of perforation such as free mediastinal and peritoneal air.2 However fish bones, chicken bones, plastic, wood, glass and thin metal objects are not readily visible.2 The false-negative rate for plain films in detecting non-bony food bolus impaction without complications has been reported to be as high as 87%.1 Therefore guidelines from the USA2 and Europe1 recommend that radiographs are not necessarily required for non-bony food bolus impaction, rather to proceed to endoscopy. The sensitivity of identifying sharp or pointed FBs on plain films is 42%–47%.10 Multidetector CT scans can improve detection reaching sensitivities up to 97%.10 The use of intravenous contrast in CT for ingested FB is not clearly defined but may unmask complications such as abscess formation, mediastinitis and aortic/tracheal fistulation.1 Although plain film radiographs were negative in our case, obtaining a CT scan was not necessary as there was sufficient ground to proceed to endoscopy in view of his strong history of FB ingestion and persistent odynophagia and dysphagia to solids.
Dentures
The majority of dentures are made from poly(methylmethacrylate) (PMMA) plastics, which are radiolucent.3 Radiolucency of dentures is a well-documented cause for misdiagnosis and delayed treatment,3 a significant contributory factor in our case too. However indirect signs on neck radiograph (box 1) can sometimes be present and make early detection, referral to ENT and prompt retrieval possible, as illustrated in a case reported by Firth et al.8 Although none of the indirect signs listed in box 1 have high positive predictive value,8 our case demonstrates the need to perform neck radiographs even for radiolucent dentures as a screening investigation.8 Missing radiographic signs can have catastrophic consequences, as illustrated in a case where a patient suffered prolonged asphyxiation and death.4 These cases stress the importance of accurate interpretation of neck radiographs and awareness of abnormal signs (box 1). Some dentures may contain a combination of materials, including metal components, making radiological detection possible. Despite attempts to increase the radio-opacity of acrylic (PMMA) dentures, none of the techniques have been adopted widely.3
Treatment
The approach to a patient with ingested FB requires a systematic assessment of airway patency. The airway may be threatened and therefore this is regarded as a medical emergency requiring immediate retrieval.1 2 A patient demonstrating signs of airway compromise requires prompt resuscitation with high flow oxygen and endotracheal intubation for airway protection.2 Once the airway is secured, the offending FB, most likely situated in the proximal oesophagus, must be retrieved via rigid oesophagoscopy under general anaesthesia by an ENT surgeon.
In the absence of airway compromise, the management depends on the type of FB, which can be classified as soft and hard. Soft (non-bony) food bolus impaction can be managed with medical therapy, such as hyoscine butylbromide in the first instance. However failure of the FB to progress into the stomach requires escalation of treatment to endoscopy. The efficacy of medical treatment is debatable and therefore should not delay definitive endoscopic treatment.1 2 As an exception, the asymptomatic clinically well patient with oesophageal soft FB can be observed for 24 hours, but failure of the FB to spontaneously pass after this period is an indication for endoscopy.2 Any FB impaction greater than 24 hours is associated with an increased risk of major complications such as perforation, mediastinitis, retropharyngeal abscess and aorto-oesophageal fistulation.11 Hard (sharp and pointed) foreign bodies are treated with a heightened sense of urgency. They should be retrieved immediately, preferably within 2 hours.1 7 In a retrospective review of complications from OGD during FB removal, sharp or pointed objects, and impaction time greater than 12 hours, were found to be independent factors associated with greater risk of complications including perforation, ulceration, laceration, abscess and failure of retrieval.12 Button battery impaction in the oesophagus is also an emergency due to its erosive potential, and requires immediate removal.1 2
The majority of FBs in adults can be managed with flexible OGD under conscious sedation, and it is generally considered first-line treatment.1 2 A variety of adjuncts are available to the endoscopist to aid in retrieval including overtubes, baskets and forceps, and more recently a transparent cap device has been shown to be effective with shorter operation time and clearer visual field.13 14 Retrieval can be en-bloc or piecemeal, or alternatively offending matter can be pushed into stomach.13 Rigid oesophagoscopy has the disadvantage of requiring general anaesthesia; however, it is more suitable for FBs impacted at the upper oesophageal sphincter and in providing airway protection.2 There is no statistically significant difference in efficacy or complication rate between flexible and rigid oesophagoscopy according to meta-analysis data, although no randomised controlled trial has been conducted on this topic.15 In difficult retrievals, a crossover strategy between flexible to rigid and vice versa may be useful.15 In cases of failed endoscopic retrieval, successful management with open pharyngo-oesophagotomy via a transcervical approach has been described.16 Other indications for open surgery include complications such as parapharyngeal or retropharyngeal abscess, mediastinitis, empyema, perforation, FB migration into adjacent structures and aorto-oesophageal fistula.16
ENT surgeons or gastroenterologists?
There were failures in triaging and prioritising our patient for endoscopic treatment. This case was discussed in both ENT and gastroenterology ‘morbidity and mortality’ meetings. The delay to OGD was deemed unacceptable. To mitigate delays in future, a new local guideline was developed at our hospital. It stated that ENT would look after patients with oesophageal foreign bodies at the level of the cricopharyngeus, and gastroenterology would take responsibility for patients with obstruction below this level. We recommend that other hospitals should also have clear protocols in place on specialty roles in management of oesophageal FB impaction, as this may vary between units depending on local preferences, skillset and available resources.
Both ENT and gastroenterology specialties are able to manage oesophageal foreign bodies with rigid and flexible oesophagoscopy respectively. This distinction has recently become blurred by the advent of flexible transnasal oesophagoscopy (TNO), practiced by ENT surgeons. TNO involves a small calibre flexible videoscope that allows evaluation of the oesophagus, and a number of interventions including retrieval of FBs.17 For example, Olympus (Japan) manufactures a TNO videoscope (ENF-VT3) with a 4.8 mm outer diameter.18 The instrument channel has an inner diameter of 2 mm.18 Compatible accessory instruments include biopsy forceps, grasping forceps, injectors and electrosurgical devices.18 Four-direction angulation capability is also available to improve the approach to an oesophageal FB.18 TNO in general has a significant advantage over other endoscopic modalities because it can be performed as an office procedure in the awake patient under topical anaesthesia.17 There are currently insufficient data to compare TNO with the more established techniques already mentioned, and the skillset to perform it is not widely available.
Learning points.
The history given by the patient is paramount in obtaining the diagnosis, planning investigations and determining treatment for oesophageal denture impaction.
Dentures are usually radiolucent and therefore a negative plain film radiograph does not exclude its presence in the oesophagus.
A low threshold for CT scan is required if the diagnosis is uncertain or there is a concern about complications.
Treatment by endoscopic retrieval must be performed urgently for sharp and pointed objects in the oesophagus.
Generally flexible oesophagogastroduodenoscopy is preferred for impacted foreign body in the oesophagus, except at the level of cricopharyngeus where a rigid oesophagoscope is more appropriate.
Footnotes
Contributors: ZM and RD were involved in the conception of the work, acquisition of data, drafting the work and final approval. ARC was involved in conception of the work, acquisition of data, drafting the work, revising it, and final approval. BN was involved in conception of the work, revising it and final approval.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1. Birk M, Bauerfeind P, Deprez PH, et al. . Removal of foreign bodies in the upper gastrointestinal tract in adults: European Society of gastrointestinal endoscopy (ESGE) clinical guideline. Endoscopy 2016;48:489–96. 10.1055/s-0042-100456 [DOI] [PubMed] [Google Scholar]
- 2. Ikenberry SO, Jue TL, Anderson MA, et al. . Management of ingested foreign bodies and food impactions. Gastrointest Endosc 2011;73:1085–91. 10.1016/j.gie.2010.11.010 [DOI] [PubMed] [Google Scholar]
- 3. Hashmi S, Walter J, Smith W, et al. . Swallowed partial dentures. J R Soc Med 2004;97:72–5. 10.1177/014107680409700206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Funayama K, Fujihara J, Takeshita H, et al. . An autopsy case of prolonged asphyxial death caused by the impacted denture in the esophagus. Leg Med 2016;23:95–8. 10.1016/j.legalmed.2016.10.006 [DOI] [PubMed] [Google Scholar]
- 5. Nayyer NV, Macluskey M. An unusual case of a misplaced denture. Oral Surg 2014;7:88–91. 10.1111/ors.12114 [DOI] [Google Scholar]
- 6. Bandyopadhyay SN, Das S, Das SK, et al. . Impacted dentures in the oesophagus. J Laryngol Otol 2014;128:468–74. 10.1017/S002221511400070X [DOI] [PubMed] [Google Scholar]
- 7. Guelfguat M, Kaplinskiy V, Reddy SH, et al. . Clinical guidelines for imaging and reporting ingested foreign bodies. AJR Am J Roentgenol 2014;203:37–53. 10.2214/AJR.13.12185 [DOI] [PubMed] [Google Scholar]
- 8. Firth AL, Moor J, Goodyear PWA, et al. . Dentures may be radiolucent. Emerg Med J 2003;20:562–3. 10.1136/emj.20.6.562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mantokoudis G, Hegner S, Dubach P, et al. . How reliable and safe is full-body low-dose radiography (LODOX Statscan) in detecting foreign bodies ingested by adults? Emerg Med J 2013;30:559–64. 10.1136/emermed-2011-200911 [DOI] [PubMed] [Google Scholar]
- 10. Ma J, Kang DK, Bae J-I, et al. . Value of MDCT in diagnosis and management of esophageal sharp or pointed foreign bodies according to level of esophagus. AJR Am J Roentgenol 2013;201:W707–11. 10.2214/AJR.12.8517 [DOI] [PubMed] [Google Scholar]
- 11. Loh KS, Tan LK, Smith JD, et al. . Complications of foreign bodies in the esophagus. Otolaryngol Head Neck Surg 2000;123:613–6. 10.1067/mhn.2000.110616 [DOI] [PubMed] [Google Scholar]
- 12. Hong KH, Kim YJ, Kim JH, et al. . Risk factors for complications associated with upper gastrointestinal foreign bodies. World J Gastroenterol 2015;21:8125–31. 10.3748/wjg.v21.i26.8125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Ooi M, Young EJ, Nguyen NQ. Effectiveness of a cap-assisted device in the endoscopic removal of food bolus obstruction from the esophagus. Gastrointest Endosc 2018;87:1198–203. 10.1016/j.gie.2017.12.022 [DOI] [PubMed] [Google Scholar]
- 14. Zhang S, Wang J, Wang J, et al. . Transparent cap-assisted endoscopic management of foreign bodies in the upper esophagus: a randomized, controlled trial. J Gastroenterol Hepatol 2013;28:1339–42. 10.1111/jgh.12215 [DOI] [PubMed] [Google Scholar]
- 15. Ferrari D, Aiolfi A, Bonitta G, et al. . Flexible versus rigid endoscopy in the management of esophageal foreign body impaction: systematic review and meta-analysis. World J Emerg Surg 2018;13 10.1186/s13017-018-0203-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Shreshtha D, Sikka K, Singh CA, et al. . Foreign body esophagus: when endoscopic removal fails…. Indian J Otolaryngol Head Neck Surg 2013;65:380–2. 10.1007/s12070-013-0662-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Sabirin J, Abd Rahman M, Rajan P. Changing trends in oesophageal endoscopy: a systematic review of transnasal oesophagoscopy. ISRN Otolaryngol 2013;2013:1–8. 10.1155/2013/586973 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Olympus Medical Systems Corp Brochure: Rhino-Laryngo Videoscope ENF-VT3 World’s First 4-Angle Observation and Treatment with High-Quality Imaging. Shinjuku Monolith, 2-3-1 Nishi-Shinjuku, Shinjuku-ku, Tokyo 163-0914, Japan. Printed in Japan N8600805-092017, 2017. [Google Scholar]


