Abstract
Objective
Volumetric laser endomicroscopy (VLE) is an advanced imaging modality used in Barrett’s oesophagus (BE) to help identify dysplasia in the oesophagus. VLE criteria exist for oesophageal dysplasia but not for dysplasia in the gastric cardia. The aim of this study was to determine if there are in vivo VLE features that can predict gastric cardia dysplasia in BE.
Design
This was a single-centre observational cohort study from August 2016 to August 2018. Patients were included if they had BE, were undergoing a VLE exam as standard of care, and had a suspicious target laser marked at the gastric cardia. The following VLE features were correlated to histology to determine if an association existed between histology subtype and VLE feature: wide crypts, irregular surface, one large isolated gland, multiple glands, and complex glands.
Results
A total of 110 in vivo gastric cardia targets in 77 patients with BE were analysed. The following abnormalities were identified: 61 wide crypts, 34 isolated glands, 16 irregular surfaces, 15 multiple glands, and 11 complex glands. Complex glands were the only VLE feature that correlated to any histology subtype. They were present in 71% of targets with high-grade dysplasia (HGD), T1a cancer or T1b cancer and had a sensitivity, specificity, and accuracy of 71%, 99%, and 85%, respectively. Of the 10 patients with complex glands on VLE and HGD/cancer on histology, 4 had a normal-appearing mucosa (40%) on endoscopy.
Conclusion
Identification of complex glands on VLE may aid in detection of HGD or early cancer in the gastric cardia in BE. This is particularly important, as dysplasia at the gastric cardia can be difficult to see endoscopically.
Keywords: oesophageal cancer, advanced imaging, ablation, dysplasia
Summary box.
What is already known about this subject?
Volumetric laser endomicroscopy (VLE) criteria exist for the oesophagus but not for the gastric cardia.
What are the new findings?
In this single-centre observational cohort study, we found that the presence of complex glands on VLE had a sensitivity, specificity, and accuracy of 71%, 99%, and 85%, respectively, for high-grade dysplasia or early cancer at the gastric cardia. In this cohort, 40% of the dysplasia or early cancer found on VLE was not seen on endoscopy.
How might it impact on clinical practice in the foreseeable future?
Surveillance endoscopy with VLE in Barrett’s oesophagus may be able to identify dysplasia or early cancer at the gastric cardia.
Introduction
Barrett’s oesophagus (BE) is defined as specialised intestinal metaplasia (IM) of the tubular oesophagus and is the known precursor to oesophageal cancer.1 Patients are at higher risk of developing oesophageal cancer if they have confirmed BE with histological low-grade dysplasia (LGD) or high-grade dysplasia (HGD).2–5 Ablation is recommended and is shown to reduce progression to adenocarcinoma.2 4 5 Thus, the goal of endoscopic surveillance in BE is to find possible dysplasia and to help risk stratify and reduce cancer progression through ablation. The current gold standard for surveillance is random biopsies within the endoscopically visualised area of BE. However, dysplasia is often focal and can be difficult to find.6 Random biopsy protocols often sample a minority of Barrett’s mucosa, and thus, it is possible to miss dysplasia; these protocols have been suggested as a mechanism for interval missed cancers in patients already enrolled in surveillance programs.7 8 Therefore, advanced imaging platforms have been proposed as a more effective modality to circumvent the sampling challenge in patients with Barrett’s metaplasia and dysplasia.9–11
One such technology that has been developed is volumetric laser endomicroscopy (VLE). This is second-generation optical coherence tomography (OCT) that uses infrared light to display high-resolution microstructure imaging. VLE can scan a 6 cm circumferential BE segment in 90 s. Laser marking is available to mark abnormal areas seen on VLE in order to help target these areas on white light endoscopy for biopsy. To date, in vivo OCT and ex vivo VLE criteria have been developed for VLE features of dysplasia in the oesophagus.12–15 These criteria have been used for more effective detection of oesophageal dysplasia in clinical practice.16–21
Although VLE criteria for dysplasia in the oesophagus have been established,12 14 15 there are limited data for VLE features of dysplasia in the gastric cardia in BE.22 23 Evaluation of VLE features of dysplasia at the gastric cardia is important as recurrences of dysplasia after ablation tend to occur at the gastric cardia.24 In addition, dysplasia in the gastric cardia may be difficult to see during endoscopy and is primarily discovered on random biopsy.24 25 The aim of this study was to determine if there are in vivo VLE features that can predict gastric cardia dysplasia or early cancer in BE.
Methods
This is a single-centre observational cohort study on consecutive patients with BE from August 2016 to August 2018. Patients were included in the study if they (1) had a prior histological diagnosis of BE; (2) were undergoing a scheduled VLE with laser marking (Nvision VLE; Ninepoint Medical, Bedford, MA, USA) for surveillance of BE (our centre uses advanced imaging with VLE for Barrett’s surveillance exams)16; (3) had a suspicious area that was VLE laser marked in the gastric cardia; (4) had corresponding histology from a biopsy or an endoscopic resection of the area with the laser mark; and (5) were greater than 18 years of age. The gastric cardia was defined as 1 cm proximal to and 2 cm distal to the top of the gastric folds per the standard definition in the literature.26 VLE exams were not performed in patients with a stricture, endoscopically visible oesophagitis or endoscopically visible carditis.
All procedures were performed by an experienced user in VLE imaging (AJT) as the standard of care for Barrett’s surveillance. All suspicious areas in the gastric cardia were classified and identified prospectively at the time of the procedure. A suspicious VLE target was one that did not contain the normal gastric cardia pattern and is defined further. Each target was laser marked with one laser mark on either side of an abnormal area. Correct laser mark placement was confirmed for each target by VLE confirmation (laser marks appear as discrete dark, hyper-reflective areas on either side of the abnormality.27 This confirmatory step was done as VLE laser marks may infrequently mark an unintended area due to oesophageal spam or motility. Each target’s associated VLE descriptors and locations were recorded on the reports at the time of the procedure. Tissue for histology was obtained from the area between each laser mark using a large-capacity biopsy forceps or by endoscopic mucosal resection of the area containing the laser marks. The histology obtained from each target was placed in a separate histology formalin jar and labelled as the corresponding VLE target.
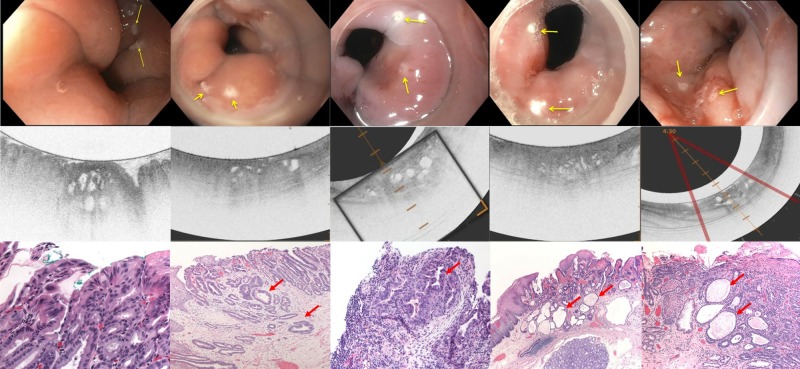
VLE descriptors used in this study that were recorded on procedure reports immediately after each procedure included (1) normal crypt and pit pattern if a normal appearance was seen on VLE (online supplementary figure 1A), (2) dilated crypts if dilated crypts were seen (online supplementary figure 1B), (3) irregular surface if the crypt and pit pattern was disrupted and was not clearly visible (online supplementary figure 2), (4) isolated glands for single glands seen, (5) multiple atypical glands if there were more than one gland that were spaced apart in a region of interest (online supplementary figure 2), and (6) complex glands defined on VLE as discrete multiple sieve-like or fused glands (figure 1). These VLE gastric cardia descriptors are routinely used in our unit based on multiple observations from previous VLE exams prior to when laser marking was available. Surface intensity and effacement are criteria often used to help identify dysplasia in the oesophagus.12 14 15 These terms were not used in this study as the gastric cardia normally has a high surface intensity compared with the subsurface and does not have layering.19 20 28
Figure 1.
Five examples of complex glands seen on VLE in this study with the corresponding laser marks and histology. The top row is the endoscopic images with laser marks (yellow arrows). The middle row is the VLE images that correspond to the above endoscopy image. The bottom row is the H&E stained histology images that correlate to the VLE images above them. Red arrows refer to complex glands. Columns 1, 2, 4, and 5 are from the endoscopic mucosal resection images. Column 3 is from a biopsy. VLE, volumetric laser endomicroscopy.
bmjgast-2019-000340supp001.pdf (1.5MB, pdf)
bmjgast-2019-000340supp002.pdf (3.1MB, pdf)
Pathology reports were then abstracted to correlate VLE features to specific histology types. This was done to determine if a VLE signature exists for carditis, IM without dysplasia, or IM with dysplasia or early cancer (T1 or T1b). If any specific VLE feature correlated to histology, then the corresponding histology slides were reviewed manually by an experienced gastrointestinal (GI) pathologist (AR). This was done in an attempt to understand and validate the VLE findings, as these should correlate with histology. Finally, patient charts were abstracted for patient characteristics.
Statistics
The Wilcoxon-Mann-Whitney test was used for comparisons of median values, and paired t-test was used for comparison of mean values. The categorical variables were compared using c2 tests or Fisher exact tests. All statistical tests were two-sided, and p<0.05 was considered significant. All analyses were conducted using SAS V.9.4 and Microsoft Excel 2019. For each VLE feature evaluated, accuracy, sensitivity and specificity was calculated. The area under the receiver operating characteristic (ROC) curve was calculated to assess the diagnostic accuracy for each VLE feature.
Results
A total of 110 in vivo gastric cardia targets in 77 patients with BE were analysed. Sixty-three (82%) of the patients were male, 35 (46%) had a hiatal hernia, and 15 (20%) patients had undergone prior endoscopic ablation. There were 61 targets that contained wide crypts, 34 that contained one isolated large gland, 16 that contained an irregular surface, 51 that contained multiple atypical glands, and 11 that contained complex glands. There were 16 targets that were normal histology, 54 targets that had carditis, 25 with IM, 1 with IM with LGD, 11 with IM with HGD or intramucosal (T1a) cancer, and three with T1b cancer. Figure 2 contains the breakdown of the histological correlates to these targets. All patients with dysplasia were naïve to endoscopic ablation therapy.
Figure 2.

Diagram showing the volumetric laser endomicroscopy features described in this study and corresponding histology. HGD, high-grade dysplasia; IM, intestinal metaplasia; IMCA, intramucosal cancer; LGD, low-grade dysplasia.
Wide crypts, an irregular surface, isolated gland, and multiple atypical glands were all seen in normal histology, carditis, IM, and IM with dysplasia. Complex glands appeared to be the only VLE feature that correlated to a specific histological subtype. It was predominantly present in dysplastic and neoplastic disease (67% and 71% of samples) with the exception of it being present in one target, which was carditis.
Table 1 shows the corresponding sensitivities and specificities for each VLE feature and the corresponding histological subtype. An irregular surface was highly sensitive and specific for LGD (100% and 86%), but this was based on one target. For all dysplasia, it was only 47% sensitive and 91% sensitive. The presence of multiple atypical glands had a sensitivity and specificity of 67% and 60%, respectively. The presence of complex glands had a sensitivity and a specificity of 64% and 99% for HGD/intramucosal cancer (IMCA). It was 100% and 93% for adenocarcinoma with T1b disease. Complex glands had a combined sensitivity and specificity of 71% and 99% for all HGD and cancer (T1a/T1b). Combining the subtypes with the highest sensitivities (multiple atypical glands and complex glands, each 67% sensitive for dysplasia) resulted in a higher sensitivity of 87%; however, the combination reduced the specificity for dysplasia to 57%. All other VLE features did not reach a high sensitivity or specificity for a specific histological subtype to be considered diagnostic (table 1).
Table 1.
Sensitivity and specificity for each VLE feature in predicting a histology subtype
| Histology | Wide crypts | Irregular surface | Isolated one gland | Multiple atypical glands | Complex glands | Combined atypical/complex glands |
| Normal | 10 (63%) 63%, 45% |
0 (0%) 0%, 83% |
7 (44%) 44%, 71% |
3 (19%) 19%, 52% |
0 (0%) 0%, 88% |
3 (19%) 19%, 48% |
| Carditis | 30 (56%) 56%, 43% |
4 (7%) 7.4%, 79% |
19 (35%) 35%, 73% |
24 (44%) 44%, 57% |
1 (2%) 2%, 82% |
25 (46%) 46%, 52% |
| Intestinal metaplasia | 16 (64%) 64%, 46% |
5 (20%) 20%, 87% |
7 (28%) 28%, 68% |
11 (44%) 44%, 56% |
0 (0%) 0%, 87% |
11 (44%) 44%, 52% |
| LGD | 1 (100%) 100%, 44% |
1 (100%) 100%,86% |
0 (0)% 0%, 69% |
1 (100%) 100%, 57% |
0 (0%) 0%, 89% |
1 (100%) 100%, 53% |
| HGD/IMCA | 5 (46%) 45%, 42% |
6 (55%) 55%, 90% |
1 (9%) 9%, 68% |
6 (55%) 55%, 61% |
7 (64%) 64%, 96% |
9 (82%) 81%, 57% |
| T1b | 0 (0%) 0%, 42% |
0 (0%) 0%, 85% |
0 (0%) 25%, 68% |
3 (100%) 100%, 58% |
3 (100%) 100%, 93% |
3 (100%) 100%, 54% |
| All dysplasia | 6 (40%) 40%, 41% |
7 (47%) 47%, 91% |
1 (7%) 7%, 65% |
10 (67%) 67%, 60% |
10 (67%) 67%, 99% |
13 (87%) 87%, 56% |
| Neoplasia: HGD/IMCA/T1b | 5 (36%) 36%, 40% |
6 (43%) 41%, 83% |
1 (7%) 7%, 66% |
9 (64%) 64%, 59% |
10 (71%) 71%, 99% |
12 (86%) 86%, 58% |
HGD, high-grade dysplasia; IMCA, intramucosal cancer; LGD, low-grade dysplasia.
Complex glands appeared to be the only VLE feature that has a high accuracy for prediction of any histology. It had an accuracy of 83% and 85% for dysplasia and early cancer, respectively. The corresponding ROC curve for HGD and early cancer is seen in figure 3.
Figure 3.
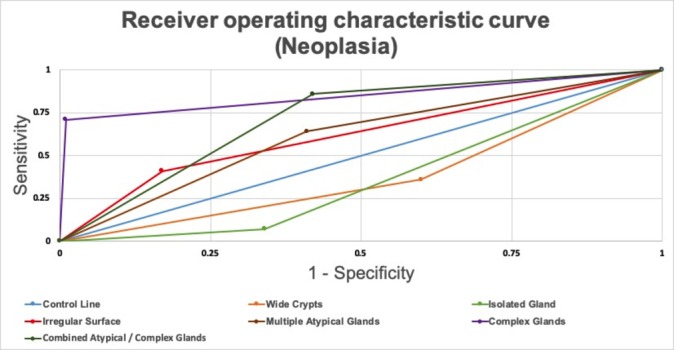
Receiver operating characteristic curve for volumetric laser endomicroscopy features described for high-grade dysplasia and early cancer (collectively called neoplasia).
Table 2 shows the correlation of cases with the VLE feature of complex glands with the histology that was reviewed by a GI pathologist, as this was the only VLE feature that correlated to a tissue subtype. Histological cribriform architecture was identified in 7 of 11 (63.6%) patients who exhibited complex glands on VLE. Cribriform glands have a specific histological pattern described in the pathology literature.29–31 Combined features of complex glands and cribriforming were noted in 9 of 11 (82%) patients. Figure 1 shows four examples of the correlation between VLE and histology. One patient had complex glands on VLE and did not have neoplasia. This patient had focally dilated pits on histology. One patient had complex glands on VLE but did not have complex or cribriform glands on histology. This patient also had cytological HGD and focally dilated pits on histology. Both of these patients had dilated pits on histology that appeared like complex glands on VLE. Of the 10 patients with complex glands on VLE and neoplasia on histology, 4 (40%) had normal-appearing mucosa on endoscopy, 3 (30%) had raised mucosa suggestive of dysplasia, and 3 (30%) had abnormal mucosa based on the pit pattern observed on narrow band imaging and high-definition white light endoscopy.
Table 2.
Comparison of endoscopic features, pathological diagnosis and histology architecture for patients with the VLE feature of complex glands
| Patient | Endoscopic features | Pathology diagnosis | Histology architecture |
| 1 | Normal-appearing mucosa | IM with HGD | Complex glands without cribriforming |
| 2 | Normal-appearing mucosa | Intramucosal adenocarcinoma (pT1a) | Complex dilated and cribriform glands |
| 3 | Abnormal-appearing mucosa | Adenocarcinoma (T1b) | Complex dilated and cribriform glands |
| 4 | Normal-appearing mucosa | Intramucosal adenocarcinoma (pT1a) | Complex dilated and cribriform glands |
| 5 | Raised mucosa | Intramucosal adenocarcinoma (pT1a) | Complex dilated and cribriform glands |
| 6 | Raised mucosa | Adenocarcinoma (T1b) | Complex glands without cribriforming |
| 7 | Normal-appearing mucosa | IM HGD | Complex glands without cribriforming |
| 8 | Abnormal-appearing mucosa | Intramucosal adenocarcinoma (pT1a) | Complex dilated and cribriform glands |
| 9 | Abnormal-appearing mucosa | Intramucosal adenocarcinoma (pT1a) | Complex dilated and cribriform glands |
| 10 | Raised mucosa | Intramucosal adenocarcinoma (pT1a) | Complex dilated and cribriform glands |
| 11 | Normal-appearing mucosa | Benign gastric cardia | Focally dilated benign gastric pits |
HGD, high-grade dysplasia; IM, intestinal metaplasia.
Discussion
After ablation for BE, recurrent or residual dysplasia tends to reoccur in the gastric cardia and may be invisible on endoscopy.24 Therefore, advanced imaging of the gastric cardia can be particularly helpful. This study examines VLE features seen in the gastric cardia in patients with BE and compares them to targeted regions of interest. There are limited data investigating VLE features of the gastric cardia in BE. Unlike for the oesophagus, there are not many reported VLE features that correlate with dysplasia or early cancer in the gastric cardia. This study adds to the literature as the presence of complex glands on VLE correlated to the histology of HGD or early cancer. Complex glands on VLE were present in 71% of targets with HGD or early cancer and had a sensitivity, specificity, and accuracy of 71%, 99%, and 85%, respectively. In this study, 40% of the patients with complex glands on VLE and dysplasia or neoplasia had normal gastric cardia endoscopic findings. This supports the growing literature that gastric cardia dysplasia may be endosocpically invisible.24 25 As this study supports, advanced imaging with VLE may help target these abnormal areas.
In the oesophagus, the presence of atypical glands in a region of interest may indicate dysplasia.14 In our practice, it is common to see numerous glands in the gastric cardia. Targeting these areas often returns a non-dysplastic result on histology. This current study confirms our suspicion that the presence of these glands at the gastric cardia/gastro-oesophageal junction on VLE may not correlate to clinically meaningful results. This was also confirmed in a pilot study, published in abstract form, examining real-time laser marking and correlation to histology.32 In that study, only 23% of laser-marked targeted biopsies were positive on histology (a positive result defined as IM, dysplasia or cancer) when glands were noted within 2 cm of the top of the gastric folds compared with a 73% positive rate in the oesophagus. Thus, the presence of glands can be seen in normal gastric cardia histology.
In our experience, we have noted that the histology of the gastric cardia is vastly different from that of the squamous or columnar-lined oesophagus with Barrett’s metaplasia. The gastric cardia shows a significantly large number of gastric pits/glands, which at places could have variable physiological dilatation of the lumen. Such glandular dilatation is often located in scattered areas and is rarely crowded or fused. This can explain the increased presence of glands seen in the gastric cardia compared with the oesophagus. However, the presence of complex and crowded glands with intervening sparse lamina propria on histology is abnormal and appears as complex glands on VLE. This can serve as a marker of dysplasia or cancer if seen on VLE.
Our study did not find a correlation between wide crypts or an irregular surface to a specific histological subtype. Although an irregular surface was more commonly seen in patients with HGD/IMCA (55% of the time), the sensitivity of 47% was not high enough to signify diagnostic criteria. The only histology predictor at the gastric cardia was the presence of complex glands, which indicated HGD or early cancer with a sensitivity, specificity, and accuracy of 71%, 99%, and 85%, respectively. Out of all the features investigated, complex glands are also the most visible as the glands are easily distinguishable from other glands and features on VLE. They are the easiest feature to interpret on VLE, given their distinct appearance (discrete multiple fused or sieve-like glands), thus making them a highly visible target.
To our knowledge, there is only one other study published23 in manuscript form examining VLE features of the gastric cardia. This study was novel in its approach but lacked targeted histology that corresponded to the VLE features seen. In addition, that series had only one patient with HGD or cancer. Complex glands were not mentioned as criteria for dysplasia likely due to the insufficient number of patients with HGD/early cancer in that series.
The main strength of our series is that in vivo targets were laser marked to allow accurate histology correlation. In addition, each laser-marked region of interest had VLE confirmation of correct placement to ensure the histology targeted was the correct site. Moreover, the inclusion of 77 patients with BE allowing for 110 laser marks in the gastric cardia allows these results to be generalisable to other BE surveillance centres. Finally, the VLE finding of complex glands was correlated to histology. This study does have limitations. This is a single-centre retrospective study and thus has the limitations associated with these types of studies. All exams were performed by one operator in a tertiary care BE centre that specialises in VLE. Thus, it is possible that other features indicative of histology subtypes at the gastric cardia exist and are not recognised in this study. There were a relatively small number of dysplastic samples at the gastric cardia that limit the gastric cardia feature discovery. Another limitation is that laser marking is influenced by endoscopic findings as a high-definition white light endoscopy is performed prior to VLE. Areas of abnormal mucosa are inherently more likely to be laser marked. In addition, of the dysplastic targets in this study, only one target was LGD, and thus these results are not generalisable for LGD. Moreover, only 4 out of the 10 patients had normal mucosa on high-definition white light endoscopy. Thus VLE in clinical practice would not find additional dysplasia in the majority of patients according to this study. However, an additional 40% yield of dysplasia detection is arguably acceptable. Finally, all of the patients in this study with dysplasia were naïve to ablation therapy, and thus this study cannot determine if there is a difference in dysplastic features at the cardia preablation and postablation.
Overall, this study contributes to the growing VLE literature in that VLE may be helpful in BE in diagnosing dysplasia not only within the oesophagus but also at the gastric cardia. There are perhaps additional features that may help improve the sensitivity of VLE for dysplasia detection in the gastric cardia. This will need to be examined in future studies at other high-volume VLE centres not only to confirm our findings but also for possible additional dysplasia feature discovery.
Footnotes
AJT and KLR contributed equally.
Contributors: Conception and design: AT. Analysis and interpretation of the data: AT, KLR, SI, AR. Drafting of the article: AT, KLR, SI, MS, JB, AV, MMcK, PB, AK, CLeg, CLee, DS, AR. Critical revision of the article for important intellectual content: AT, KLR, SI, MS, JB, AV, MMcK, PB, AK, CLeg, CLee, DS, AR. Final approval of the article: AT, KLR, SI, MS, JB, AV, MMcK, PB, AK, CLeg, CLee, DS, AR.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent for publication: Not required.
Ethics approval: Institutional review board (IRB) approval was granted by the Zucker School of Medicine at Hofstra/Northwell (IRB number 17-0033).
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data are available upon reasonable request.
References
- 1.Spechler SJ, Souza RF. Barrett's esophagus. N Engl J Med 2014;371:836–45. 10.1056/NEJMra1314704 [DOI] [PubMed] [Google Scholar]
- 2.Shaheen NJ, Falk GW, Iyer PG, et al. . ACG clinical guideline: diagnosis and management of Barrett's esophagus. Am J Gastroenterol 2016;111:30–50. quiz 51 10.1038/ajg.2015.322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Duits LC, van der Wel MJ, Cotton CC, et al. . Patients With Barrett's esophagus and confirmed persistent low-grade dysplasia are at increased risk for progression to neoplasia. Gastroenterology 2017;152:993–1001. 10.1053/j.gastro.2016.12.008 [DOI] [PubMed] [Google Scholar]
- 4.Shaheen NJ, Sharma P, Overholt BF, et al. . Radiofrequency ablation in Barrett's esophagus with dysplasia. N Engl J Med 2009;360:2277–88. 10.1056/NEJMoa0808145 [DOI] [PubMed] [Google Scholar]
- 5.Phoa KN, van Vilsteren FGI, Weusten BLAM, et al. . Radiofrequency ablation vs endoscopic surveillance for patients with Barrett esophagus and low-grade dysplasia: a randomized clinical trial. JAMA 2014;311:1209–17. 10.1001/jama.2014.2511 [DOI] [PubMed] [Google Scholar]
- 6.Anandasabapathy S. Advanced imaging in Barrett's esophagus: are we ready to relinquish the random? Clin Gastroenterol Hepatol 2013;11:1571–2. 10.1016/j.cgh.2013.07.032 [DOI] [PubMed] [Google Scholar]
- 7.Sharma P, Falk GW, Weston AP, et al. . Dysplasia and cancer in a large multicenter cohort of patients with Barrett's esophagus. Clin Gastroenterol Hepatol 2006;4:566–72. 10.1016/j.cgh.2006.03.001 [DOI] [PubMed] [Google Scholar]
- 8.Corley DA, Mehtani K, Quesenberry C, et al. . Impact of endoscopic surveillance on mortality from Barrett's esophagus-associated esophageal adenocarcinomas. Gastroenterology 2013;145:312–9. 10.1053/j.gastro.2013.05.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Qumseya BJ, Wang H, Badie N, et al. . Advanced imaging technologies increase detection of dysplasia and neoplasia in patients with Barrett's esophagus: a meta-analysis and systematic review. Clin Gastroenterol Hepatol 2013;11:1562–70. 10.1016/j.cgh.2013.06.017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Thosani N, Abu Dayyeh BK, Sharma P, et al. . ASGE technology Committee systematic review and meta-analysis assessing the ASGE preservation and incorporation of valuable endoscopic innovations thresholds for adopting real-time imaging-assisted endoscopic targeted biopsy during endoscopic surveillance of Barrett's esophagus. Gastrointest Endosc 2016;83:684–98. 10.1016/j.gie.2016.01.007 [DOI] [PubMed] [Google Scholar]
- 11.Sharma P, Brill J, Canto M, et al. . White paper AGA: advanced imaging in Barrett's esophagus. Clin Gastroenterol Hepatol 2015;13:2209–18. 10.1016/j.cgh.2015.09.017 [DOI] [PubMed] [Google Scholar]
- 12.Evans JA, Poneros JM, Bouma BE, et al. . Optical coherence tomography to identify intramucosal carcinoma and high-grade dysplasia in Barrett's esophagus. Clin Gastroenterol Hepatol 2006;4:38–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Poneros JM, Brand S, Bouma BE, et al. . Diagnosis of specialized intestinal metaplasia by optical coherence tomography. Gastroenterology 2001;120:7–12. 10.1053/gast.2001.20911 [DOI] [PubMed] [Google Scholar]
- 14.Leggett CL, Gorospe EC, Chan DK, et al. . Comparative diagnostic performance of volumetric laser endomicroscopy and confocal laser endomicroscopy in the detection of dysplasia associated with Barrett's esophagus. Gastrointest Endosc 2016;83:880–8. 10.1016/j.gie.2015.08.050 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Swager A-F, Tearney GJ, Leggett CL, et al. . Identification of volumetric laser endomicroscopy features predictive for early neoplasia in Barrett's esophagus using high-quality histological correlation. Gastrointest Endosc 2017;85:918–26. 10.1016/j.gie.2016.09.012 [DOI] [PubMed] [Google Scholar]
- 16.Alshelleh M, Inamdar S, McKinley M, et al. . Incremental yield of dysplasia detection in Barrett's esophagus using volumetric laser endomicroscopy with and without laser marking compared with a standardized random biopsy protocol. Gastrointest Endosc 2018;88:35–42. 10.1016/j.gie.2018.01.032 [DOI] [PubMed] [Google Scholar]
- 17.Trindade AJ, Inamdar S, Sejpal DV. Dysplasia detection in Barrett's esophagus by use of volumetric laser endomicroscopy with laser marking. VideoGIE 2017;2:217–8. 10.1016/j.vgie.2017.05.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Trindade AJ, Vamadevan AS, Sejpal DV. Finding a needle in a haystack: use of volumetric laser endomicroscopy in targeting focal dysplasia in long-segment Barrett's esophagus. Gastrointest Endosc 2015;82:756–7. 10.1016/j.gie.2015.03.1984 [DOI] [PubMed] [Google Scholar]
- 19.Trindade AJ, Leggett CL, Chang KJ. Volumetric laser endomicroscopy in the management of Barrett's esophagus. Curr Opin Gastroenterol 2017;33:254–60. 10.1097/MOG.0000000000000366 [DOI] [PubMed] [Google Scholar]
- 20.Trindade AJ, Inamdar S, Smith MS, et al. . Volumetric laser endomicroscopy in Barrett's esophagus: interobserver agreement for interpretation of Barrett's esophagus and associated neoplasia among high-frequency users. Gastrointest Endosc 2017;86:133–9. 10.1016/j.gie.2016.11.026 [DOI] [PubMed] [Google Scholar]
- 21.Trindade AJ, Inamdar S, Smith MS, et al. . Learning curve and competence for volumetric laser endomicroscopy in Barrett's esophagus using cumulative sum analysis. Endoscopy 2018;50:471–8. 10.1055/s-0043-121569 [DOI] [PubMed] [Google Scholar]
- 22.Trindade AJ, Inamdar S, Sejpal DV, et al. . Targeting neoplasia using volumetric laser endomicroscopy with laser marking. Endoscopy 2017;49:E54–5. 10.1055/s-0042-122144 [DOI] [PubMed] [Google Scholar]
- 23.Gupta N, Siddiqui U, Waxman I, et al. . Use of volumetric laser endomicroscopy for dysplasia detection at the gastroesophageal junction and gastric cardia. World J Gastrointest Endosc 2017;9:319 10.4253/wjge.v9.i7.319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Guthikonda A, Cotton CC, Madanick RD, et al. . Clinical outcomes following recurrence of intestinal metaplasia after successful treatment of Barrett's esophagus with radiofrequency ablation. Am J Gastroenterol 2017;112:87–94. 10.1038/ajg.2016.451 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Sami SS, Ravindran A, Kahn A, et al. . Timeline and location of recurrence following successful ablation in Barrett's oesophagus: an international multicentre study. Gut 2019;68:1379–85. 10.1136/gutjnl-2018-317513 [DOI] [PubMed] [Google Scholar]
- 26.Misumi A, Murakami A, Harada K, et al. . Definition of carcinoma of the gastric cardia. Langenbecks Arch Chir 1989;374:221–6. 10.1007/BF01359557 [DOI] [PubMed] [Google Scholar]
- 27.Swager A-F, de Groof AJ, Meijer SL, et al. . Feasibility of laser marking in Barrett's esophagus with volumetric laser endomicroscopy: first-in-man pilot study. Gastrointest Endosc 2017;86:464–72. 10.1016/j.gie.2017.01.030 [DOI] [PubMed] [Google Scholar]
- 28.Trindade AJ, Smith MS, Pleskow DK. The new kid on the block for advanced imaging in Barrett's esophagus: a review of volumetric laser endomicroscopy. Therap Adv Gastroenterol 2016;9:408–16. 10.1177/1756283X16639003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Minardi D, Mazzucchelli R, Scarpelli M, et al. . Prostate cancer glands with cribriform architecture and with glomeruloid features should be considered as Gleason pattern 4 and not pattern 3. Future Oncol 2016;12:1431–3. 10.2217/fon-2016-0113 [DOI] [PubMed] [Google Scholar]
- 30.Moreira AL, Joubert P, Downey RJ, et al. . Cribriform and fused glands are patterns of high-grade pulmonary adenocarcinoma. Hum Pathol 2014;45:213–20. 10.1016/j.humpath.2013.10.011 [DOI] [PubMed] [Google Scholar]
- 31.Humphrey PA. Cribriform adenocarcinoma of the prostate. J Urol 2015;193:1655–6. 10.1016/j.juro.2015.02.035 [DOI] [PubMed] [Google Scholar]
- 32.Chin MA, Chen C-lin, Samarasena JB, et al. . Tu1152 initial human experience with novel laser marking volumetric laser endomicroscopy in Barrett's esophagus: assessment of real-time targeting and the value of Co-Registration. Gastrointest Endosc 2017;85:AB558–9. 10.1016/j.gie.2017.03.1289 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjgast-2019-000340supp001.pdf (1.5MB, pdf)
bmjgast-2019-000340supp002.pdf (3.1MB, pdf)