Abstract
Background & objectives:
Hypertension is a health problem of global priority. Screening and early diagnosis is important to plan appropriate interventions. The present study objectives were to screen the urban population aged 30 yr and above and diagnose for hypertension and to identify the factors associated with poor screening for hypertension, if any.
Methods:
A community-based descriptive cross-sectional study was conducted in urban field practice area of a tertiary care hospital in Puducherry, India, among individuals aged 30 yr and above. Individuals were asked if they have tested themselves for hypertension in the past two years. Pretested questionnaire was used for data collection. Data collection was done during regular working time of the health centre. All eligible participants from consecutive households were included till the required sample size of 394 was achieved.
Results:
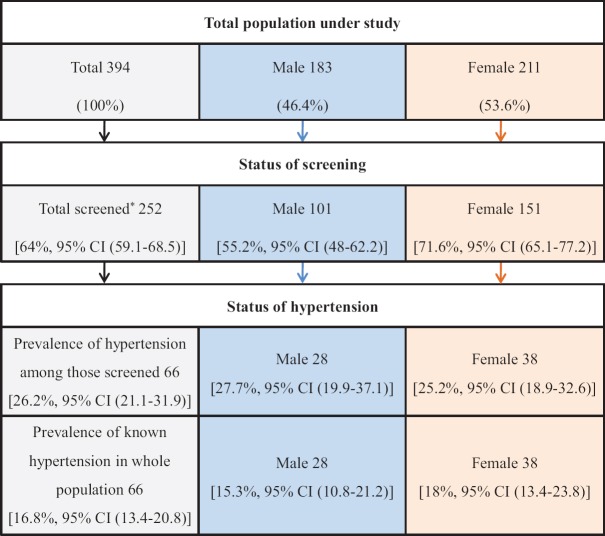
Of the 394 individuals interviewed, 252 (64%) had undergone screening for hypertension. The prevalence of self-reported hypertension among those screened was 26.2 per cent with no significant gender-wise differences. Screening for hypertension was better among females (71.6%) as compared to males (55.2%). Population who were at a higher risk of not getting screened for hypertension were relatively younger (30-44 yr) individuals and males.
Interpretation & conclusions:
The prevalence of self-reported hypertension among those screened was 26.2 per cent [95% confidence interval (21.1-31.9)]. Screening needs to be targeted more towards males and younger population.
Keywords: Adults, hypertension, India, screening, urban
Hypertension is the most common of cardiovascular disorders, and is defined as a systolic blood pressure of ≥140 mmHg and /or a diastolic reading ≥90 mmHg1,2. Stroke, heart failure, myocardial infarction, chronic kidney disease, peripheral vascular disease, retinopathy, dementia and premature mortality are the proven adverse health consequences of persistently elevated blood pressure3. Globally, it accounts for the death of 9.4 million people each year due to complications arising out of it4. In India, it is estimated that 10 per cent of all deaths are attributable to hypertension5.
Patient awareness regarding the diseased condition as well as their health-seeking behaviour influences tackling of this modern epidemic6. Hypertension is often asymptomatic in the early stages, and hence, many people go undiagnosed. Screening is simple and economic and helps in early diagnosis and treatment, which in the long run can prevent complications4. The present study was thus planned to screen the population 30 yr and above of an urban field practice area of a tertiary care hospital in southern India for hypertension and identify the factors associated with poor screening.
Material & Methods
It was a community-based cross-sectional study conducted over a period of two months from July to August 2015, and included adults, aged 30 yr and above, who were residing in urban field practice area of Jawaharlal Institute of Postgraduate Medical Education & Research (JIPMER), Puducherry, India, for more than six months. Due approval of the Institute Ethics Committee of JIPMER, Puducherry, was sought before undertaking data collection.
Study tool: Pretested questionnaire was used to elicit necessary information from the study population. Self-reported history regarding screening for hypertension was assessed over the past two years. All the individuals giving positive history of having undergone blood pressure measurement in the past two years, irrespective of the place or reasons for blood pressure measurement, were considered as 'screened for hypertension'. It was assumed that the proportion of population aged 30 yr and above, screened for hypertension, was 50 per cent; considering confidence interval of 95 and 5 per cent absolute precision, the estimated sample size required for the study was 394.
Study setting, sampling and procedure: The study area catered to a population of around 8000, distributed over four wards, namely Kurusukuppam, Chinnayapuram, Vaithikuppam and Vazhaikulam. For convenience, the study was restricted to one of the wards (Chinnayapuram) which was randomly selected. All consecutive households with eligible participants available during the data collection period were included in the study till the required sample size was achieved. The targeted sample size was achieved by recruiting individuals from 174 of the total 410 households present in the area. All the locked houses were visited second time before those were excluded. Informed written consent was obtained from the head of each family. The standard definition recommended in census7 was used for assessing education status. Modified Prasad's classification8 was used for assessing socio-economic status. Occupation was operationally categorized into those not working, work involving 'manual and less regular work' and work involving 'less manual but more regular work'.
Statistical analysis: Data collected were entered using EpiData version 3.1 (EpiData Association, Copenhagen, Denmark) and were analyzed using EpiData analysis version 2.2.2.183 (EpiData Association, Odense, Denmark). Results were expressed in proportions. Bivariate analysis was performed to find the association of these factors with those not screened for hypertension. Unadjusted odds ratio (OR) and adjusted OR (aOR) with 95 per cent confidence intervals (CIs) were used to describe the associations between groups. The prevalence of hypertension among those screened was analyzed using proportions.
Results & Discussion
About two-third [(n=252) 64%; 95% CI (59.1-68.5)] of the study population reported to have been screened for hypertension status at least once in the past two years. The prevalence of self-reported hypertension among those screened was 26.2 per cent (n=66), [95% CI (21.1-31.9)] and the prevalence of known hypertension in entire population was 16.8 per cent (66/394), [95 % CI (13.4-20.8)].
Screening for hypertension, as shown in Figure, was more among females (71.6%) as compared to males (55.2%). I also shows that the population who were significantly at higher risk of not getting screened for hypertension were males [aOR 2.3, 95% CI (1.2-4.1)] and younger adults aged 30-44 yr [aOR 3.8, 95% CI (1.6-8.9)].
Figure.
Flowchart showing gender differences in screening and diagnosis of hypertension. *Among 252 individuals who were screened, 8 individuals (3.2%) did not know the results of screening. Among these 8 individuals, 5 were male and 3 were female.
Table.
Sociodemographic determinants for not undergoing screening for hypertension in the past two years, among individuals aged 30 yr and above, in an urban field practice area (n=394)
| Characteristics | n (%) | Not screened (n=142; 36.1%) | Screened£ (n=252; 63.9%) | 95% CI | |
|---|---|---|---|---|---|
| Unadjusted OR | aOR | ||||
| Gender (n=394) | |||||
| Male | 183 (46.4) | 82 (44.8) | 101 (55.2) | 2.04 (1.35-3.10) | 2.3 (1.2-4.1) |
| Female | 211 (53.6) | 60 (28.4) | 151 (71.6) | 1 | 1 |
| Age (n=394) (yr) | |||||
| 30-44 | 229 (58.1) | 103 (45.0) | 126 (55.0) | 4.09 (2.03-8.21) | 3.8 (1.6-8.9) |
| 45-59 | 99 (25.1) | 28 (28.3) | 71 (71.7) | 1.97 (0.90-4.31) | 2.1 (0.8-5.05) |
| 60 yr and above | 66 (16.7) | 11 (16.7) | 55 (83.3) | 1 | 1 |
| Marital status (n=394) | |||||
| Married | 293 (74.4) | 114 (38.9) | 179 (61.1) | 1.66 (1.01-2.72) | 1.0 (0.5-1.8) |
| Single/widow | 101 (25.6) | 28 (27.7) | 73 (72.3) | 1 | 1 |
| Family type (n=394) | |||||
| Joint/three generations | 76 (19.3) | 31 (40.8) | 45 (59.2) | 1.28 (0.77-2.14) | 0.8 (0.3-1.8) |
| Nuclear | 318 (80.7) | 111 (34.9) | 207 (65.1) | 1 | 1 |
| Education* (n=390) | |||||
| Higher secondary and above | 51 (13.1) | 19 (37.3) | 32 (62.7) | 1.75 (0.88-3.47) | 1.4 (0.8-2.4) |
| Primary/middle/secondary | 201 (51.5) | 86 (42.8) | 115 (57.2) | 2.20 (1.37-3.54) | 1.1 (0.4-2.5) |
| Illiterate | 138 (35.4) | 35 (25.4) | 103 (74.6) | 1 | 1 |
| Occupation* (n=390) | |||||
| Manual and less regular work$ | 163 (41.8) | 69 (42.3) | 94 (57.7) | 1.63 (1.05-2.51) | 0.6 (0.3-1.2) |
| Less manual but more regular work$ | 34 (8.7) | 11 (32.4) | 23 (67.6) | 1.06 (0.49-2.31) | 0.4 (0.1-1.2) |
| Unemployed/retired/homemakers# | 193 (49.5) | 60 (31.1) | 133 (68.9) | 1 | 1 |
| Socio-economic status† (n=394) | |||||
| Class 3 and above | 225 (57.1) | 89 (39.6) | 136 (60.4) | 1.43 (0.94-2.18) | 0.7 (0.4-1.1) |
| Class 1 and 2 | 169 (42.9) | 53 (31.4) | 116 (68.6) | 1 | 1 |
*Four individuals were excluded from analysis due to incomplete response; #157 (housewives), 23 (unemployed) and 13 (retired); †Modified Prasad’s classification updated May 2014; $Occupations such as manual labourers, painter, fishermen, craftsman, machine operators, tailors and carpenter were categorized as Manual and less regular jobs and occupations such as professionals, office managers and clerks. Salespersons, etc., were categorized as ‘Less manual but more regular work’; £Among those screened, 66 (28 males and 38 females) reported having hypertension. OR, odds ratio; aOR, adjusted OR; CI, confidence interval
There are many community-based studies estimating the prevalence of hypertension6,9. The limitation of the present study was that selection bias could have affected the true estimates of the population that were screened, as it was carried out during the working period when young active population, particularly man were busy in their workplaces. This could be the reason for better hypertension screening among females and the elderly in our study. Another limitation was that the recall bias might have affected the results of self-reported hypertension as history was taken for the past two years. In Joint National Committee (JNC)-7 guidelines2, it is recommended that screening for hypertension among individuals with normal or optimal blood pressure should be done at least once every two years. Assuming that, majority of the individuals in the population were normal; we assessed the proportion of individuals who got themselves tested for hypertension in the past two years.
Non-availability of medical reports with many patients at the time of interview was a major limitation to relate self-reported hypertension status with that of their medical records. The clustering of hypertension cases in the households was not considered during sample size calculation; this was another limitation of the study.
In conclusion, almost two-third of the population (64%) was screened for hypertension, and prevalence of self reported hypertension was 26.2 per cent among those screened for hypertension in the past-two years. Overall, prevalence of self reported hypertension was 16.8 per cent.
Acknowledgment
Authors acknowledge the contribution of staff of JIPMER Urban Health Centre (JIUHC) and Anganwadi workers posted in JIUHC service area for their support during this study.
Footnotes
Financial support & sponsorship: The first author (SD) acknowledges the Indian Council of Medical Research, New Delhi, for providing Short Term Studentship (STS no. 2015-01380).
Conflicts of Interest: None.
References
- 1.Mahal A, Karan A, Engelgau M. The economic implications of non-communicable disease for India. Washington, DC: The World Bank; 2010. [accessed on October 28, 2017]. Available from: http://www.siteresources.worldbank.org/HEALTHNUTRITIONANDPOPULATION/R esources/281627-1095698140167/EconomicImplicationsof NCDforIndia.pdf . [Google Scholar]
- 2.Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: The JNC 7 report. JAMA. 2003;289:2560–72. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 3.Flack JM, Peters R, Shafi T, Alrefai H, Nasser SA, Crook E. Prevention of hypertension and its complications: Theoretical basis and guidelines for treatment. J Am Soc Nephrol. 2003;14:S92–8. doi: 10.1097/01.asn.0000070142.14843.8e. [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization. Silent killer, global public health crisis. World Health Day. Geneva: WHO; 2013. [accessed on October 28, 2017]. A global brief on hypertension. Available from: http://www.ishworld.com/downloads/pdf/global_brief_hypertension.pdf . [Google Scholar]
- 5.Indian Council of Medical Research. Hypertension: The silent killer. New Delhi: Department of Health Research, Ministry of Health & Family Welfare, Government of India; 2018. [accessed on July 8, 2018]. Available from: https://www.icmr.nic.in/sites/default/files/press_realease_files/Hypertension.pdf . [Google Scholar]
- 6.Mohan V, Deepa M, Farooq S, Datta M, Deepa R. Prevalence, awareness and control of hypertension in Chennai – The Chennai urban rural epidemiology study (CURES-52) J Assoc Physicians India. 2007;55:326–32. [PubMed] [Google Scholar]
- 7.Department Of School Education & Literacy. Educational statistics at a glance. New Delhi: Ministry of Human Resource Development, Government of India; 2016. [accessed on July 8, 2018]. Available from: https://mhrd.gov.in/sites/upload_files/mhrd/files/statistics-new/ESG2016.pdf . [Google Scholar]
- 8.Mangal A, Kumar V, Panesar S, Talwar R, Raut D, Singh S. Updated BG Prasad socioeconomic classification, 2014: A commentary. Indian J Public Health. 2015;59:42–4. doi: 10.4103/0019-557X.152859. [DOI] [PubMed] [Google Scholar]
- 9.Devi P, Rao M, Sigamani A, Faruqui A, Jose M, Gupta R, et al. Prevalence, risk factors and awareness of hypertension in India: A systematic review. J Hum Hypertens. 2013;27:281–7. doi: 10.1038/jhh.2012.33. [DOI] [PubMed] [Google Scholar]