Abstract
We report herein on two cases where high-risk osseous foreign bodies that incarcerated or penetrated the bronchial wall. The foreign bodies were unable to be removed via flexible bronchoscope (FB), with the foreign bodies close to the pulmonary artery and aortic artery. After preoperative evaluation and planning with the virtual bronchoscopic navigation (VBN) system, the airway foreign bodies were extracted effectively and safely using advanced therapeutic endoscopic technique by rigid bronchoscope (RB), thus avoiding the surgical thoracotomy.
Keywords: Virtual bronchoscopic navigation, LungPoint, Foreign body, High risk, Rigid bronchoscope, Removal, Artery
1. Introduction
Airway foreign bodies result from aspiration are common in not only in children, but also adults. For large osseous foreign bodies which are incarcerated or penetrated the bronchial wall, after many failed removal attempts by bronchoscope, surgical operation seems to be the only solution, especially when such foreign bodies are close to large vessels [1]. In clinical practice, however, many patients are not candidates for surgery due to the underlying diseases and complications. So how to remove the foreign bodies by bronchoscopy is still a central focus of interventional pulmonologists. Our paper reports on two cases of patients who were admitted to our hospital, both with osseous foreign bodies incarcerated or penetrated through the bronchial wall, close to major arteries and unable to be removed by flexible bronchoscope (FB). Leveraging preoperative evaluation and planning by VBN system, both of the osseous foreign bodies were completely, effectively and safely removed by the advanced therapeutic endoscopic technique of rigid bronchoscopy combined with flexible bronchoscopy.
2. Cases report
2.1. Case A
A 49-year old female who presented with aggravated cough along with fever since a fish bone was sucked up due to the accident while eating one month ago. The thoracic computer tomography (CT) revealed that an osseous foreign body was incarcerated in the lumen of the intermediate bronchus (BI) of accompanied by distal obstructive pneumonia of right middle lobe. Airway examination by FB at another hospital showed that the osseous foreign body was incarcerated in the lumen of BI firmly with obvious local proliferation of granulation tissue. Therapeutic flexible bronchoscopies were performed, however, were unable to remove the foreign bodies. The patient was referred to our hospital. One day later, the therapeutic bronchoscopies under moderate sedation was performed again in our bronchscopic suite. We firstly used mild sedation with propofol, until we inserted the jack wire and then we inserted a jet-catheter with heavy sedation, under jet-ventilation model. Firstly, we removed the granulation tissue around the foreign body by the high frequency electrocautery probe. Although we tried several different kinds of foreign body forceps, we still failed to remove the foreign bodies due to its incarceration. Then, the patient was administered intravenous anti-infection, as well as anti-inflammation treatment to reduce edema, expectoration and other symptomatic treatment for 1 week then the clinical symptoms such as chest pain, fever were alleviated. The Enhanced chest CT scan revealed that an unregular shape foreign body with high density was incarcerated in the BI lumen, with sharp tip very close to the right pulmonary artery. The nearest layer is less than 1.5mm from the right pulmonary artery. Localized pulmonary atelectasis of right middle lobe and slight inflammation of superior segment of left lower lobe (LLL) were shown on the CT scan (Fig. 1A, B).
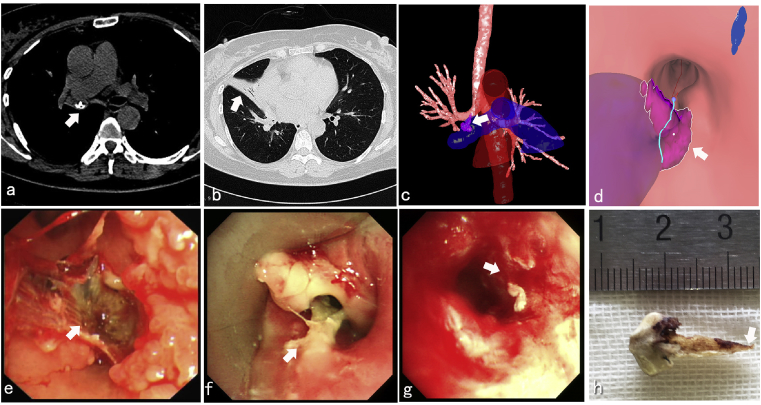
Fig. 1.
Patient procedure preparation.
We used the VBN system to conduct analysis of the airway foreign bodies: lung CT data were imported into the LungPoint® AR Bronchoscopic Navigation System. The system not only reconstructed the bronchial tree and major arteries nearby as three-dimensional (3D) structure (Fig. 1C), but also the 3D structure of the foreign body within the BI (Fig. 1D). The length of strip-shaped foreign body was 15mm. Both ends of the foreign body were arrow-like. The distal end of foreign body was more blunt and pointed towards the right middle lobe, close to the right BI lateral wall. The sharper arrow-like end was located in the lumen of right main bronchus (RMB), partly incarcerated in the interior wall of the RMB. According to the preoperative assessment provided by VBN, we formulated a plan to removal of the foreign body using rigid bronchoscopy under general anesthesia.
During the actual procedure, the STORZ rigid bronchoscope (RB) with 12.5mm outside diameter was intubated into the lumen of RMB, then observed that the osseous foreign body's size and location were consistent with preoperative evaluation of VBN (Fig. 1E). The distal end of the RB was carefully adjusted so that the proximal sharp end of the osseous foreign body entered the lumen of the RB (Fig. 1F). Then the therapeutic FB was intubated through the lumen of the RB. Under the view of the FB, we adjusted the angle of rigid forcep to clamp the proximal end of the foreign body. According to the direction indicated by the VBN assessment, we avoided pushing the foreign body forward and downward, which would have damaged the pulmonary artery. Instead, the foreign body was clamped directly into the lumen of RB, and then was dragged out of the RB. The foreign body was completely removed, and the mucosal ulcer caused by the foreign body on the lateral wall of the BI was seen, but there was no bleeding. The distal mucosa of BI was swollen with a small amount of sputum in the cavity, and the distal lumen was reopened after the suction. The osseous foreign body was 12 × 21 × 8mm in size and consistent with the reconstructed imaging of the foreign body by VBN (Fig. 1H). The full endoscopic procedure took about 25 minutes and estimated blood loss was less than 3ml. The patient recovered well after procedure without any complications. Follow-up with CT scan showed normal 1 month later.
2.2. Case B
A 45-year-old male sought medical care due to frequent cough and expectoration along with breathlessness for one month. The patient had suffered viral encephalitis 20 years ago, which result in hypophrenia and inability to live independently without being cared for by family. Thoracic CT at the local hospital revealed left pleural effusion (partly encysted) and LLL atelectasis. Therapeutic bronchoscopies was done and they found a suspicious osseous foreign body obstruction in the lumen of left inferior lobar bronchus with local granulation tissue hyperplasia. However, the foreign body could not be removed. Anti-infection, expectorant treatment and other symptomatic treatment did not work effectively. By 2 weeks ago, the patient had fever along with chest pain on the left side, breathlessness and dyspnea. The maximum body temperature was 38.9 °C. Cough and expectoration worsened. Sputum was white and hard to cough out. Then he was referred to our hospital. After hospitalized thoracic augmented CT scan was done, which revealed high-density curved osseous foreign body shadow in the lumen of left inferior lobar bronchus (Fig. 2A). It seemed that part of the foreign body penetrated the bronchial wall and stabbed into the pulmonary parenchyma. The distal end of foreign body was sharp and the closest distance to descending aorta was merely 3.37mm. Obstructive atelectasis in LLL along with moderate amount of pleural effusion in the left thoracic cavity was shown in the enhanced CT scan (Fig. 2B). The admission diagnosis was: 1) Transmural bronchial osseous foreign body in the LLL 2) Obstructive atelectasis in the basal segment of LLL 3) Pneumonia effusion in the LLL.
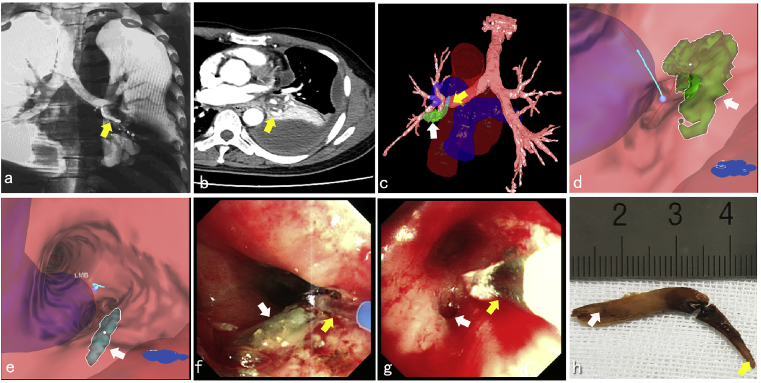
Fig. 2.
Patient procedure preparation.
After hospitalization, we used VBN System to carry out preoperative evaluation and endoscopic surgery planning: 3D anatomical structure was reconstructed by the LungPoint® AR Bronchoscopic Navigation system. The image showed the anatomical structure of the foreign body, bronchial tree and large vessels nearby (Fig. 2C). The shape of osseous foreign body was long and curved. Its distal end located in the lumen of left inferior basal segmental bronchus (Fig. 2C, D), while the proximal end penetrated through the bronchial wall of the orifice of LLL, stabbing into pulmonary parenchyma with 15mm in length. The proximal part of foreign body stabbed into pulmonary parenchyma had a very sharp tip and was very close to the descending aorta only 4mm away (Fig. 2C, E). According to the preoperative evaluation of VBN, we carried out the bronchoscopic surgery plan that first applied laser cutting to break the osseous foreign body in the airway and then extracted the pieces out one by one.
During the actual endoscopic procedure, the RB with 12.5mm outside diameter was intubated into the lumen of left main bronchus (LMB), then the therapeutic FB was intubated through the lumen of RB and located the foreign body in the left inferior basal segmental bronchus of LLL, which showed actual location consistent with the VBN preoperative evaluation. Firstly, the thulium laser probe was inserted and separated the intracavitary section of the osseous foreign body with 8W power (Fig. 2F). Next, the flexible foreign body forcep was used to catch and remove the intraluminal section of foreign body, then the outcrop of the extraluminal section of foreign body was clamped and pushed into the lumen of left inferior basal segmental of LLL, then removed through the RB completely. Endobronchial cryotherapy was applied to deal with the regional granulation tissue (Fig. 2G). The Long curved foreign body was measured with 35 × 20 × 3mm in size, which was consistent with VBN pre-operative evaluation (Fig. 2H). The endoscopic surgery took about 45 minutes totally and estimated hemorrhage was less than 2ml during the procedure. The patient recovered well after surgery, anti-inflammation and symptomatic treatment were applied. The follow-up CT revealed that encysted pleural effusion in left had been absorbed and left inferior lung was completed re-expanded 2 months later. The patient had no special complaints.
3. Discussion
Methods of removing airway foreign bodies include endoscopic removal and surgical removal. When patient's clinical symptoms and chest imaging are highly indicative of aspiration with airway foreign body, airway exam by FB is the preferred method. According to the literature statistics, about 90% of the airway foreign bodies can be removed by FB, while about 8% of the airway foreign bodies should be removed under general anesthesia by means of RB. Even so, there are still about 2% of airway foreign bodies which are high-risk or difficult to remove that require thoracic surgery. This kind of airway foreign bodies usually have such characteristics as long-term retention in body, large volume and osseous density. Flexible bronchoscopy is regarded as the first choice for the diagnosis and treatment process when airway foreign bodies is indicated by imaging. If airway foreign body is unable to be removed by FB or RB, thoracic surgery will be the last choice. Indications for surgical removal of difficult airway foreign bodies that cannot be removed endoscopically include: 1) Foreign bodies locating in the distal lumen of bronchus, long-time retention and adhesion to surrounding tissues, along with distal obstructive pneumonia. 2) Large or hard foreign bodies penetrating through the bronchial wall or even stabbed into pulmonary parenchyma. 3) Osseous or metallic foreign bodies, being close to large vessels with high risk of massive hemorrhage. Although the difficult or high risk airway foreign bodies could be in theory extracted by thoracic surgeries, unfortunately most of patients cannot tolerate the surgeries due to multiple underlying diseases or poor general conditions. What's more, thoracic surgery-related loss of lung function as well as potential bronchial fistula clearly increased the rate of postoperative complications [1,2]. So how to apply minimally endobronchial removal of difficult or high-risk foreign bodies with the help of preoperative formulation and evaluation by new technologies, is still an issue for interventional pulmonologists.
Virtual bronchoscopic technology originated in 1996. As a computer reconstruction system based on CT imaging and 3D airway anatomy, it was used to evaluate the degree of stenosis in the central airway, and it can also form the imaging of 3D structure. Therefore, CT 3D airway reconstruction has been applied to assist therapeutic procedures for complex airway stenosis disease by bronchoscope since the last century [3]. In the 21st century, with the progress of imaging technology, more and more earlier peripheral lung cancer can be screened by the low-dose spiral CT. A new generation VBN system derived from virtual imaging technology, has already been applied in clinic as a mature product for the endobronchial diagnostic procedures of peripheral lung lesions [[4], [5], [6]]. More importantly, there are distinct differences comparison with the previous 3D reconstruction by CT data and virtual bronchoscope technology. 3D construction by CT data refers to the airway 3D reconstruction carried out by radiologists. The effect of 3D construction depends on the radiologist's knowledge and experiences of the target region, functions of CT software and the radiologist willingness to invest the necessary time. VBN system is a preoperative evaluation and navigation system especially designed for pulmonologists and interventional pulmonologists, then the pulmonologists are able to use the VBN system for the preoperative evaluation without difficulties, so the change of the operator for data construction is beneficial to the endoscopic procedure. Moreover, functions that modern VBN possesses can also be expanded to the area of endobronchial therapeutic procedures [7], such as locating and evaluating bronchial pleural fistula and assisting in its endobronchial management [8]. It can also be used to locate and evaluate airway foreign body in child and assist in the strategy of endoscopic removal. Literature reported that for those diagnosis of children suspected of airway foreign bodies, where the child is symptomatic but negative in the conventional chest radiogram, using VBN evaluation can improve the sensitivity and specificity of the foreign body finding, up to 92.3% and 85.7%, respectively [9]. Takenaka et al. [10] located the residual surgical gauze in the peripheral lung, which cannot be found by FB and finally removed successfully with the help of VBN navigation.
Modern VBN system already possess the functions for locating, measuring and stereo imaging of lesions as well as navigation. It can reconstruct accurately not only 3D structure of lesions but also major vessels nearby, and it can also show the details of airway foreign body in 3D from endobronchial view, CT view, and anatomy view, which is conducive to make preoperative scheme for high-risk foreign bodies endobronchial removal. LungPoint® AR Bronchoscopic Navigation system has the real-time navigation function based on the combination of virtual reconstruction and actual endoscopic procedures, which decreases the rate of complications and increases the rate of success in the endobronchial removal of high risk airway foreign bodies [11]. Our cases of high-risk airway foreign bodies mentioned above were incarcerated and penetrated through the bronchial wall, unable to be removed by FB. In order to avoid surgical thoracotomy, the VBN system was used to carry out preoperative evaluation and formulate surgery scheme. For the first case, VBN shows the detailed 3D structure of the intraluminal foreign body and the exact location where it was incarcerated. On the basis of VBN's evaluation, it was decided not to use endoscopic laser to separate the osseous foreign body, which was liable to penetrate the wall and damage pulmonary artery. The distal of arrow-tip like foreign body was incarcerated in right middle segmental bronchi and the closest distance to right pulmonary artery is within 1.5mm. The solution was instead to use the rigid forcep to clamp the arrow tip-like foreign body and lift it upward directly into the pipeline of RB. As for the second osseous foreign body which penetrated through the bronchial wall. VBN system showed that the shape of airway foreign body was long and curved, with its proximal end penetrating through the bronchial wall and stabbing into left inferior lobar pulmonary parenchyma, and the distance between descending aorta and its proximal end was within 4mm. Hence, if we directly clamped the foreign body by foreign body forceps, the foreign body could not be removed and should likely damage pulmonary parenchyma or even descending aorta, which would lead to fatal hemoptysis. So we made a two-step plan. Firstly, we separated the intraluminal section by laser cutting, and removed the intraluminal section by forcep. After that, we remove the section outside the bronchial wall. We carried out the procedures successfully and effectively as planned. In actual practice, we still noted several limitations of the LungPoint AR system in its evaluation of the foreign body, planning and navigation, for examples, the reconstructed foreign body's image is not realistic enough, the extraction function of foreign body in lumen of distal bronchi is not perfect, imprecise measurement of foreign body size, lack of accurate navigation and so on. All of these need further improvements. Additionally, the successful extraction of the two high-risk foreign bodies was also due to comprehensive factors such as intravenous anti-infection, cortical hormone to anti-inflammation and using FB to clear granulation tissue surrounding the foreign body before procedures, using in combination with RB, experiences of the operator and so on [12,13].
In conclusion, for these two cases of high-risk airway foreign bodies which were unable to be removed by bronchoscope, after the comprehensive evaluation and surgical planning with the VBN system, the foreign bodies were both endobronchially removed safely and effectively, thus avoiding surgical thoracotomy. Therefore, as for these kinds of high-risk airway foreign bodies, VBN is recommended as a new tool for preoperative evaluation and formulating endobronchial plans, it offers value for further application and summarization in clinical practice.
Contributions
All authors contributed equally.
Declaration of competing interest
None to declare.
Acknowledgements
Funding: This work was supported by the Project of New Clinical Technology Development of Changhai Hospital, Shanghai, China (No. NT201506), the Project of Precision Medicine Transformation Application Research of the Second Military Medical University (2017JZ05).
Contributor Information
Paul Zarogoulidis, Email: pzarog@hotmail.com.
Chong Bai, Email: bai_chong@163.com.
References
- 1.Blanco Ramos M., Botana-Rial M., Garcia-Fontan E., Fernandez-Villar A., Gallas Torreira M. Update in the extraction of airway foreign bodies in adults. J. Thorac. Dis. 2016;8(11):3452–3456. doi: 10.21037/jtd.2016.11.32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dong Y.C., Zhou G.W., Bai C., Huang H.D., Sun Q.Y., Huang Y., Han Y.P., Li Q. Removal of tracheobronchial foreign bodies in adults using a flexible bronchoscope: experience with 200 cases in China. Intern. Med. 2012;51(18):2515–2519. doi: 10.2169/internalmedicine.51.7672. [DOI] [PubMed] [Google Scholar]
- 3.Asano F. Virtual bronchoscopic navigation. Clin. Chest Med. 2010;31(1):75–85. doi: 10.1016/j.ccm.2009.08.007. (Table of Contents) [DOI] [PubMed] [Google Scholar]
- 4.Asano F., Ishida T., Shinagawa N., Sukoh N., Anzai M., Kanazawa K., Tsuzuku A., Morita S. Virtual bronchoscopic navigation without X-ray fluoroscopy to diagnose peripheral pulmonary lesions: a randomized trial. BMC Pulm. Med. 2017;17(1):184. doi: 10.1186/s12890-017-0531-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tamiya M., Okamoto N., Sasada S., Shiroyama T., Morishita N., Suzuki H., Yoshida E., Hirashima T., Kawahara K., Kawase I. Diagnostic yield of combined bronchoscopy and endobronchial ultrasonography, under LungPoint guidance for small peripheral pulmonary lesions. Respirology. 2013;18(5):834–839. doi: 10.1111/resp.12095. [DOI] [PubMed] [Google Scholar]
- 6.Oki M., Saka H., Ando M., Asano F., Kurimoto N., Morita K., Kitagawa C., Kogure Y., Miyazawa T. Ultrathin bronchoscopy with multimodal devices for peripheral pulmonary lesions. A randomized trial. Am. J. Respir. Crit. Care Med. 2015;192(4):468–476. doi: 10.1164/rccm.201502-0205OC. [DOI] [PubMed] [Google Scholar]
- 7.Okimasa S., Shibata S., Awaya Y., Nagao Y., Murakami I., Shigeto E. Virtual bronchoscopy aids management of lung cancer. Respirology. 2007;12(4):607–609. doi: 10.1111/j.1440-1843.2007.01090.x. [DOI] [PubMed] [Google Scholar]
- 8.Hayama M., Sato S., Shiroyama T., Nishida T., Nishihara T., Okamoto N. Endoscopic bronchial occlusion with silicone spigots under virtual bronchoscopic navigation. Respirol. Case Rep. 2016;4(4) doi: 10.1002/rcr2.157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bhat K.V., Hegde J.S., Nagalotimath U.S., Patil G.C. Evaluation of computed tomography virtual bronchoscopy in paediatric tracheobronchial foreign body aspiration. J. Laryngol. Otol. 2010;124(8):875–879. doi: 10.1017/S0022215110000769. [DOI] [PubMed] [Google Scholar]
- 10.Takenaka T., Katsura M., Shikada Y., Furuya K., Takeo S. Intrapulmonary foreign body removal under virtual bronchoscopic navigation. J. Bronchol. Interv. Pulmonol. 2012;19(2):159–161. doi: 10.1097/LBR.0b013e31824f5a99. [DOI] [PubMed] [Google Scholar]
- 11.Eberhardt R., Kahn N., Gompelmann D., Schumann M., Heussel C.P., Herth F.J. LungPoint--a new approach to peripheral lesions. J. Thorac. Oncol. : Off. Publ. Int. Assoc. Stud. Lung Canc. 2010;5(10):1559–1563. doi: 10.1097/JTO.0b013e3181e8b308. [DOI] [PubMed] [Google Scholar]
- 12.Moisan T.C. Retained endobronchial foreign body removal facilitated by steroid therapy of an obstructing, inflammatory polyp. Chest. 1991;100(1):270. doi: 10.1378/chest.100.1.270. [DOI] [PubMed] [Google Scholar]
- 13.Acharya K. Rigid bronchoscopy in airway foreign bodies: value of the clinical and radiological signs. Int. Arch. Otorhinolaryngol. 2016;20(3):196–201. doi: 10.1055/s-0036-1584293. [DOI] [PMC free article] [PubMed] [Google Scholar]