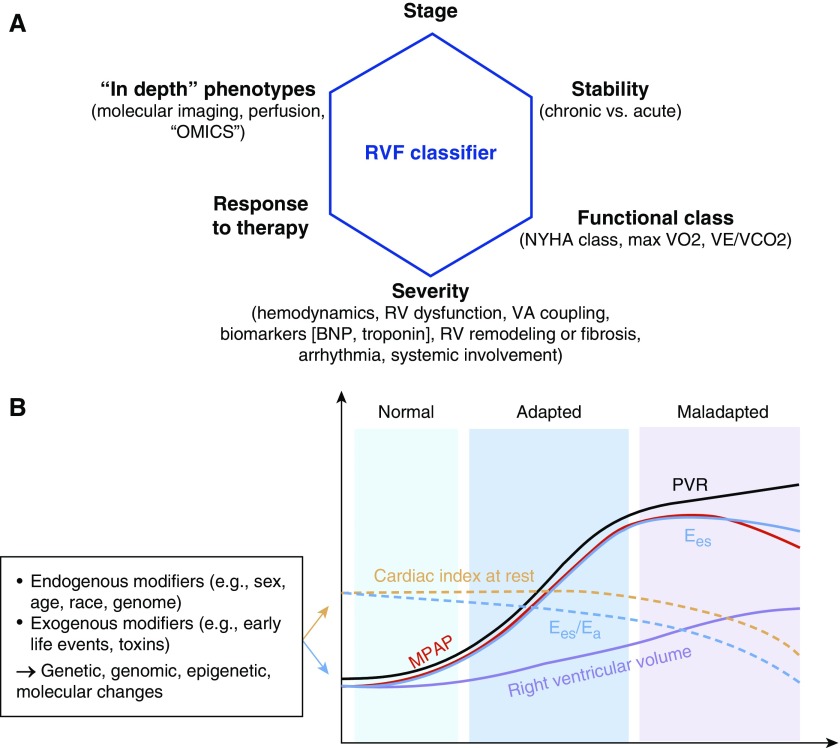
Figure 2.
Classifiers and time course of right ventricular failure (RVF). (A) RV function is described using several characteristics, such as stage and acuity, as well as functional class (either by New York Heart Association [NYHA] classification or by cardiopulmonary exercise testing) and severity (using hemodynamic characteristics, markers of RV function, ventriculoatrial [VA] coupling, imaging or plasma biomarkers indicating RV remodeling, as well as presence or absence of arrhythmias [e.g., atrial fibrillation] and presence or absence of systemic involvement [e.g., liver congestion, renal impairment]) (2, 128, 162). Response to therapy (e.g., treatment-responsive vs. refractory RVF) is frequently used for classifying RV function as well. Novel classifiers and “deep” phenotyping tools include imaging approaches aimed at assessing perfusion, metabolism, and/or fibrosis, complemented by “omics” and “big data” approaches. (B) Time course of RVF development in the setting of chronic pressure overload from pulmonary vascular disease. See Reference 128 for detailed review of the supporting literature. Note that significant molecular and temporal heterogeneity exist in RV adaptation and maladaptation to pressure overload, possibly determined by genetic, genomic, epigenetic, and molecular changes due to endogenous and exogenous factors. For example, in scleroderma-associated pulmonary arterial hypertension (PAH), end-systolic elastance (Ees) is lower than in idiopathic PAH, and Ees/arterial elastance (Ea) decreases earlier than in other disease states (170). Cardiac output/cardiac index decreases as a result of transition from adaptive to maladaptive remodeling, because of either progression of the underlying disease or an additional insult. BNP = brain natriuretic peptide; MPAP = mean pulmonary arterial pressure; PVR = pulmonary vascular resistance. (B) Modified from Reference 302.