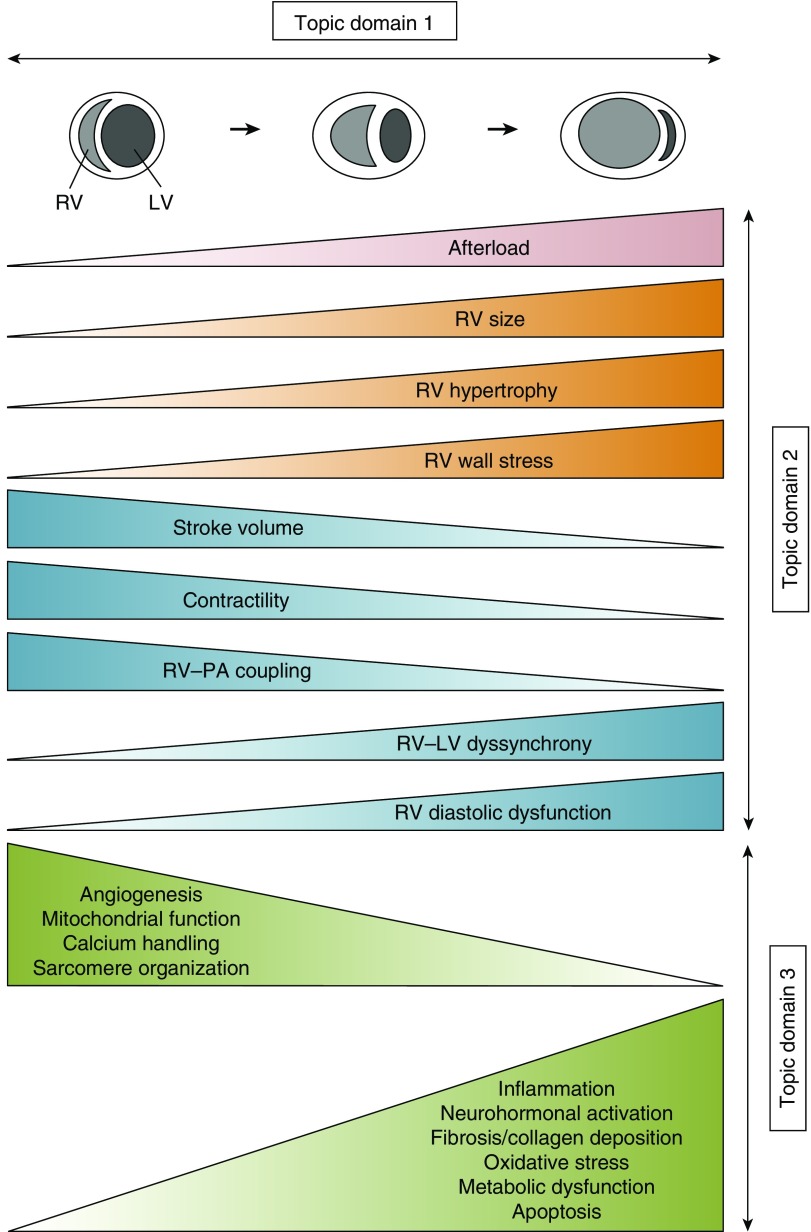
Figure 3.
Concept figure of changes in right ventricular (RV) structural, functional, and biochemical/molecular processes as the RV transitions from normal function to failure in the setting of increased afterload. Afterload increases can be acute (e.g., in cases of pulmonary embolism or acute respiratory distress syndrome) or chronic (e.g., in pulmonary arterial hypertension, pulmonary hypertension from chronic heart or lung disease, or chronic thromboembolic pulmonary hypertension). With progressive increases in RV afterload (top), RV size increases. In forms of chronic afterload increases, RV hypertrophy develops. RV stroke volume, RV contractility, and RV–pulmonary artery (PA) coupling are initially maintained (or even increased) but then progressively decrease. In parallel, RV diastolic dysfunction and RV–left ventricular (LV) dyssynchrony develop. At a molecular/biochemical level, these processes are accompanied by alterations in angiogenesis, calcium handling, mitochondrial function, and sarcomere organization, as well as progressive increases in inflammation, neurohormonal activation, fibrosis/collagen deposition, oxidative stress, metabolic dysfunction, and cardiomyocyte apoptosis. Note that for didactic purposes, long-term trajectories for all changes are shown as gradual increases or decreases, whereas in reality these changes may exhibit fluctuations and not develop in a parallel manner. Topic domain 1 of this research statement focuses on optimizing the methodology to assess RV function in acute and chronic conditions in preclinical models, human studies, and clinical trials. Structural and functional RV changes (shown in red, orange, and blue) are covered in topic domain 2; biochemical/molecular processes (in green) are discussed in topic domain 3.