Figure 1.
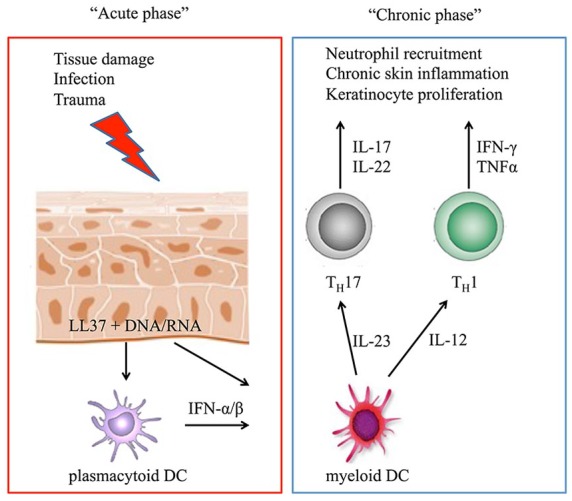
The proposed mechanisms of the immunological imbalance observed in psoriasis are summarized in the acute and chronic settings. In the acute phase of the disease, tissue damage induced, for example, by trauma or infection leads to the production of antimicrobial peptides by keratinocytes, particularly LL37. These peptides can form complexes with DNA or RNA molecules and, via toll-like receptor signaling, activate plasmacytoid dentritic cells (pDC), which produce type I interferons (IFN-α/β). Myeloid DCs are attracted and activated by IFN-α/β as well as from LL37/RNA complexes and secrete IL-12 and IL-23. They activate and induce helper T (TH) cells to develop a TH1 and TH17 phenotype, respectively, and initiate the chronic phase of the disease characterized by sustained production of the indicated proinflammatory cytokines, leading to neutrophil recruitment, chronic skin inflammation, and the formation of psoriatic plaques.
