Abstract
Background:
In response to the opioid overdose epidemic, scalable interventions that instruct at-risk populations how to prevent and respond to overdose scenarios are needed.
Method:
The following groups of at-risk individuals were recruited online: (1) Acute Pain patients with an opioid prescription, (2) Chronic Pain patients with an opioid prescription, and (3) persons without pain who use Illicit Opioids. Participants were tested on their opioid overdose knowledge using the Brief Opioid Overdose Knowledge (BOOK) questionnaire and randomized to one of two web-based interventions that contained 25 educational content slides. One intervention consisted of embedded questions with corrective feedback (Presentation + Mastery, n = 58), the other did not (Presentation, n = 61). Participants completed the BOOK again at the end of the intervention and 30 days later. Overdose risk behaviors were assessed at baseline and 30-days.
Results:
Relative to baseline, both Presentation and Presentation + Mastery interventions increased total BOOK scores immediately and 30 days later. There was a significant effect of Group on BOOK Knowledge, whereby those with Acute Pain had lower scores across time, regardless of intervention, relative to those with Chronic Pain and Illicit Opioid Use. Compared to baseline, all three groups reported fewer instances of using opioids alone or concurrently with alcohol at the 30-day follow-up.
Conclusions:
A web-based intervention increased opioid overdose knowledge and decreased overdose risk behavior immediately and at a one-month follow-up, suggesting that this brief, practical, and scalable program could have utility in several populations who are at-risk of opioid overdose.
1. Introduction
The United States has experienced a 500% increase in opioid overdose (OD) deaths in the past 20 years (Hedegaard, Minino, & Warner, 2018). Interventions that instruct at-risk populations on how to prevent and appropriately respond to OD scenarios are needed. Given the unprecedented scope of the current opioid epidemic, interventions that are cost-effective, easily administered, and effective in multiple opioid-using populations will confer maximum public health impact.
Although the majority of existing OD interventions have been implemented among illicit opioid using groups (Dunn, Yepez-Laubach, et al., 2017; Jones, Roux, Stancliff, Matthews, & Comer, 2014), overdose from prescribed opioids for pain has also increased over the past decade (Hedegaard et al., 2018). Research suggests that individuals who take opioids for pain management have lower baseline knowledge of opioids, opioid overdose, and opioid overdose responses (Dunn, Barrett, Fingerhood, & Bigelow, 2017; Dunn et al., 2016). Developing self-paced and internet-based brief educational interventions that effectively increase OD knowledge and retention may be especially important for individuals who are prescribed opioids without ongoing medical support. Opioid naïve patients who are prescribed opioids at hospital discharge for acute or post operative pain might be at particular risk for opioid misuse, and may benefit substantially from these interventions (Brat et al., 2018; Calcaterra et al., 2016).
Web-based interventions have been shown to produce significant increases on the Brief Opioid Overdose Knowledge Questionnaire (BOOK), a validated questionnaire for assessing OD knowledge, in persons with opioid use disorder (Dunn et al., 2016; Dunn, Yepez-Laubach, et al., 2017) or receiving opioids for chronic pain (Huhn, Garcia-Romeu, & Dunn, 2018). Web-based interventions have been evaluated in both a clinical setting and remotely via the crowdsourcing platform Amazon Mechanical Turk (mTurk), which was able to recruit individuals who are not yet in treatment for a confidential web-based intervention. mTurk participants were free to opt into the intervention and complete it using their own personal computers at their own pace without any intervention administrator. Two intervention versions have been compared. The first (“Presentation”) contained 25 educational slides with texts, pictures, and videos and reviewed general opioid knowledge, opioid-OD knowledge, and opioid-OD response knowledge. The second (“Presentation + Mastery”) was identical aside from questions embedded throughout the presentation that required participants to correctly answer ≥80% of questions in each batch. Two previous studies (Dunn et al., 2017; Huhn et al., 2018) have found both interventions (Presentation, Presentation + Mastery) to produce comparable knowledge gains. One of these studies that assessed knowledge retention among persons with opioid use disorder at 30 and 90-days and reported knowledge gains were sustained(Dunn, Yepez-Laubach, et al., 2017). Participants were also less likely to report using opioids by themselves at follow-up.
The current study replicates and extends these studies by comparing knowledge as rated by the BOOK following the Presentation and Presentation + Mastery interventions (Dunn et al., 2016) and assessing 30-day knowledge retention following web-based delivery through mTurk This is also the first study to compare participants with acute or chronic pain who had a current prescription for an opioid analgesic, or participants with no pain who endorsed current illicit opioid use. This study was conducted to address concerns that previous Presentation and Presentation + Mastery interventions produced comparable gains in immediate knowledge (Huhn et al., 2018), but might not have captured intervention-based differences in long-term retention, based on evidence that Presentation + Mastery interventions are generally more effective at increasing knowledge relative to Presentation interventions (Krebs, Prochaska, & Rossi, 2010). Therefore, it was hypothesized that both Presentation and Presentation + Mastery web-based interventions would increase post-intervention BOOK total scores, but the Presentation + Mastery intervention would lead to greater BOOK scores at the 30-day follow-up. It was also postulated that all three populations would show significant gains in BOOK scores.
2. Method
2.1. Study Design
2.1.1. Screening and Participant Eligibility
Participants were recruited between July 2018 and August 2018 from Amazon Mechanical Turk (MTurk). The study recruited MTurk “workers” to respond to Human Intelligence Task (HIT) advertisement for a survey on “health behaviors” (Buhrmester, Kwang, & Gosling, 2011; Dworkin, Hessel, Gliske, & Rudi, 2016). Although mTurk workers tend to be young, educated, and report poorer health quality and higher rates of depression (Mortensen, Alcala, French, & Hu, 2018; Walters, Christakis, & Wright, 2018), empirical comparisons have found mTurk outcomes to be comparable to those collected in field and laboratory experiments (Chandler & Shapiro, 2016; Strickland & Stoops, 2019). The current study blinded the intervention target during screening to prevent falsification of responses and equal numbers of participants from each pain group (e.g., acute pain, chronic pain, no pain) were enrolled. Eligibility was assessed with a brief screening for which participants were compensated $0.10. Eligible participants had an ≥ 80% approval rate from completion of previous HITs, were ≥18 years old, reported currently using an opioid (either licitly or illicitly, with several examples given), and resided in the United States. The Johns Hopkins University Internal Review Board reviewed this study and categorized it as not constituting human subject’s research because data were both confidential and anonymous.
2.1.2. Interventions
Following completion of the BOOK knowledge pre-test, participants were randomly assigned to the Presentation or Presentation + Mastery intervention. Randomization was conducted within each pain group (acute, chronic, no pain) to ensure equal representation between the interventions. Interventions were administered using the online survey manager Qualtrics (Provo, UT, USA). The Presentation intervention contained 25 educational content slides with text, pictures, and/or videos that discussed general opioid knowledge, opioid OD knowledge, and opioid OD response knowledge (Dunn et al., 2016; Huhn et al., 2018). The Presentation + Mastery intervention was identical to the Presentation intervention but embedded questions with corrective feedback throughout the slides. Embedded questions differed from the BOOK Questionnaire items, and required participants to achieve ≥ 80% accuracy to advance the intervention. If ≥80% accuracy was not achieved, the module repeated to provide participants another opportunity to answer questions correctly. Participants that failed 3 times were automatically advanced to the next module. After completing the intervention, participants answered questions about past 30-day risk behaviors (see below) and their familiarity with and comfort using naloxone (Narcan) and were compensated $5.
2.1.3. Follow-up
Researchers sent participants a message through an Amazon mTurk platform containing a link to a follow-up survey using their MTurk worker ID 30-days after intervention completion. Participants accessed the survey by clicking on the link and typing in their MTurk worker ID; only participants who completed the initial survey were authorized to access the link. The follow-up survey included the BOOK Questionnaire and questions about past 30-day behaviors that increased the risk of an OD. Participants earned $2 for completing the follow-up questions within 5 days of receiving the email.
2.3. Study Measures
2.3.1. Measures to Characterize the Sample.
Participants provided information about sex, age, education, and employment status, as well as current opioid use (both licit and illicit) and past year drug use. Current pain (acute, chronic, or no pain) was determined using question 1 on the Brief Pain Index (Cleeland & Ryan, 1994; Poquet & Lin, 2016), which defines acute and chronic pain as “pain other than everyday kinds of pain (e.g., minor headaches, sprains, toothaches) for <3 months or ≥3 months”, respectively.
2.3.2. OD Measures
The primary outcome measure in this study was the BOOK total score, which was collected pre and post intervention, and at the 30-day follow-up (Dunn et al., 2016; Huhn et al., 2018). The BOOK is comprised of 12 items that correspond to three domains: general opioid knowledge, opioid OD knowledge, and opioid OD response knowledge. Response options were “True”, “False”, or “I Don’t Know”. Correct responses were summed to generate three subscale scores (range: 0–4) and one total score (range: 0–12).
Participants also indicated whether they had used prescription opioids or heroin by themself, used pain pills or heroin at the same time as alcohol, or used methadone that was not prescribed to them as measures of risk behavior.
2.3.3. Acceptance Measures.
Immediately after the intervention participants rated intervention acceptability on a number of domains. These included general acceptability, rated on a scale from 1 (strongly agree) to 5 (strongly disagree),whether they believed the intervention would help prevent them from overdosing in the future, whether it would change the way they would help other people who are overdosing and whether they would recommend the intervention to a family member or friend (yes/no).
2.4. Statistical Analysis
Sample size was based on the number of cases needed to detect within (pre, post, and follow-up) x between (Presentation, Presentation + Mastery) interactions on the BOOK total score across the three time points and between two intervention types. A power analysis conducted with G Power indicated that a total sample size of 120 (40 per pain group) would provide 95% power to detect a small effect size. Participants were over-sampled (N = 185) to ensure adequate enrollment, based on previously reported drop-out rates for mTurk studies (Johnson & Jiang, 2017). Since pain groups were expected to enter the intervention with different baseline knowledge, analyses did not covary for group differences and instead evaluated knowledge gains and retention within each pain group independently. All analyses were restricted to participants who completed the 30-day follow-up (N=119) so that differences in knowledge retention across the three time points could be assessed.
Demographics, time to complete the intervention, and prior OD and naloxone experiences were compared across interventions using 3×2 Factorial ANOVAs for continuous variables and chi-squared analyses for categorical variables. To characterize differences in participants who were and were not retained at the various stages, demographics were compared across participants who did not complete the entire intervention, did not complete the 30 day follow up, or who completed all assessments, using ANOVAs and chi-squared analyses as appropriate. To test the primary question of how well the two intervention types improved BOOK scores across time, main effects and interactions were examined using repeated measures analyses of variance (RM ANOVA) for the BOOK total and three subscores. RM ANOVAs then tested the main effects and interactions of each pain group, intervention type, and timepoint on BOOK total and three subscores. Finally, RM ANOVA tested differences in total BOOK scores at pre-and post-intervention across participants who did and did not completed the 30-day follow-up. Bonferroni corrected post-hoc analyses probed significant effects of Time and Pain Group.
Past 30-day OD risk behaviors (using opioids alone, using opioids and alcohol concurrently, taking methadone that was not prescribed) were dichotomized into yes/no values for the baseline and 30-day follow-up visits and compared across intervention type and pain groups as a function of time using chi-squared tests.
Consistent with previous studies, acceptability questions that were scored on a 5-point Likert scale were rescored such that “Strongly Agree” and “Agree” were coded as “Yes” and “Neutral”, “Disagree” and “Strongly Disagree” were coded as “No” (Huhn et al., 2018). Responses were then compared across intervention type and pain group using chi-squared tests. Finally, the rate of attrition, defined as failure to complete the intervention after consenting, was compared across pain groups as another proxy measure of intervention acceptability using chi-squared tests.
With the exception of the attrition-related analyses (N=258), all analyses were restricted to the subset of participants who completed the entire study through the 30-day follow-up (N = 119).
Alpha levels for significant findings were set at p < .05 and analyses were conducted using SPSS version 25.0.
3. Results
3.1. Participants
A total of 1,642 mTurk workers were screened for eligibility, 258 (15.7% of screened sample) were eligible and initiated the study intervention, 185 (11.2%) completed the intervention, and 119 (64.3% of intervention completers; Presentation N=61 and Presentation + Mastery N=58) completed the 30-day follow-up (Figure 1). Of the 58 who completed all 11 embedded quizzes Presentation + Mastery intervention, there were 22 instances where a participant failed three times. Compared to study completers, participants who did not complete the intervention or did not complete the 30-day follow-up were less likely to be employed full-time, p’s < .05; no additional differences were observed.
Figure 1.
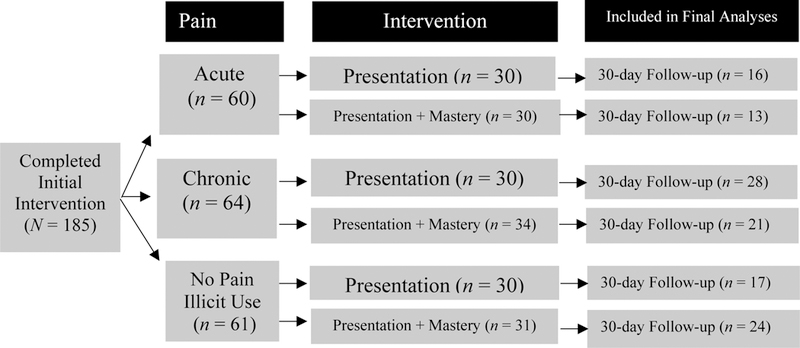
Number of participants within each Pain Group and Intervention.
Demographics did not differ across participants randomized to the Presentation and Presentation + Mastery groups (Table 1). Participants spent significantly more minutes completing the Mastery + Presentation intervention (M = 36.4 minutes, SD = 22.3) than the Presentation intervention (M = 27.4, SD = 15.8), F(1, 119) = 8.5, p = .004.
Table 1.
Participant Characteristics by Population and Randomized Intervention
| Total N = 119 |
Acute Pain n = 29 |
Chronic Pain n = 49 |
No Pain, Illicit Use n = 41 |
|||||
|---|---|---|---|---|---|---|---|---|
| Presentation (N=61) |
Presentation + Mastery (N=58) |
Presentation (N=16) |
Presentation + Mastery (N=13) |
Presentation (N=28) |
Presentation + Mastery (N=21) |
Presentation (N=17) |
Presentation + Mastery (N=24) |
|
| % Male | 57 | 56 | 67 | 39 | 47 | 41 | 69* | 77* |
| Age (M ± SD) | 34.7 ± 11.4 | 35.0 ± 10.8 | 35.8 ± 15.5 | 36.7 ± 15.7 | 36.0 ± 9.0 | 38.1 ± 10.7 | 30.9 ± 8.2 | 31.6 ± 8.7 |
| Education (% Highest Degree Earned) | ||||||||
| High School | 34 | 44 | 38 | 31 | 26 | 50 | 47 | 46 |
| 2-year degree | 22 | 15 | 19 | 31 | 32 | 17 | 19 | 4 |
| 4-year college degree | 30 | 31 | 38 | 23 | 26 | 17 | 30 | 46 |
| Master’s degree/Terminal degree/ | 14 | 11 | 6 | 15 | 16 | 17 | 17 | 4 |
| % Employed full time | 75 | 64 | 80 | 62 | 69 | 71 | 81 | 59 |
| % Uninsured | 16 | 10 | 13 | 0 | 13 | 6 | 27 | 18 |
| % Used Drug Last 30 Days | ||||||||
| Alcohol | 60 | 65 | 54 | 74 | 41 | 47 | 88* | 87* |
| Benzodiazepines | 29 | 19 | 13 | 7 | 9 | 12 | 44* | 55* |
| Cannabis | 56 | 58 | 46 | 67 | 30 | 41 | 75* | 86* |
| MDMA | 12 | 8 | 8 | 7 | 0 | 0 | 23* | 25* |
| Prescription Stimulants | 21 | 11 | 0 | 0 | 12 | 6 | 41* | 31* |
| BPI Pain Severity Score (1–10) (M ± SD) |
3.1 ± 3.2 | 3.5 ± 3.0 | 1.7 ± 2.4 | 1.3 ± 2.0 | 4.2 ± 2.4# | 3.8 ± 2.9# | 2.5 ± 2.2 | 1.8 ± 2.2 |
| BPI Pain Interference Score (1–10) (M ± SD) |
2.8 ± 2.8 | 2.8 ± 2.5 | 2.0 ± 2.8 | 1.4 ± 1.9 | 3.6 ± 2.6# | 4.2 ± 2.6# | 2.6 ± 2.2 | 1.8 ± 2.8 |
| % Heard of naloxone (Narcan) | 86 | 90 | 77 | 80 | 90 | 94 | 81 | 96 |
| % Ever OD | 16 | 14 | 13 | 15 | 9 | 12 | 18* | 14* |
| % Ever Witnessed OD | 51 | 40 | 33 | 40 | 50 | 35 | 69* | 46* |
| Minutes to complete intervention (M+SD) † | 27.4 ± 15.8 | 36.4 ± 22.3 | 19.4 ± 8.0 | 38.2 ± 20.6 | 32.1 ± 18.1 | 34.9 ± 15.4 | 26.3 ± 14.3 | 36.4 ± 27.7 |
Note:
Asterisks indicate that the no pain group significantly differed from acute and chronic pain groups.
Hashtags indicate that chronic pain groups significantly differed from acute pain and no pain groups. BPI=Brief Pain Inventory, M= mean, SD= standard deviation, OD=overdose,
indicates a significant difference between Presentation and Presentation + Mastery interventions
As expected, the pain groups differed in a few baseline characteristics. Specifically, the no pain/illicit use group was more likely to be male, report past 30-day alcohol, cannabis, benzodiazepine, MDMA and prescription stimulant use, and have both witnessed and experienced an OD in their lifetime, relative to the acute and chronic pain groups (Table 1). Chronic pain participants also reported significantly higher pain severity and interference, as measured by the Brief Pain Inventory, compared to acute and no pain participants.
3.2. BOOK Score Outcomes
RM ANOVA indicated a significant main effect of Time on BOOK total scores, F(1.8, 212.2) = 79.6, p < .001, general opioid subscores, F(1.8, 206.2) = 36.7, p < .001, OD subscores, F(1.8, 207.8) = 28.1, p < .001, and OD response subscores, F(1.9, 220.3) = 210.9, p < .001, such that scores significantly increased from pre-to post-intervention and 30-day follow-up (Figure 2, Table 2). There were small significant decreases in all scores and subscores (except opioid OD response knowledge) between post-intervention and 30-day follow-up, p’s < .05 (Table 2). There was no significant effect of Intervention nor Time x Intervention on BOOK scores, p’s > .05
Figure 2.
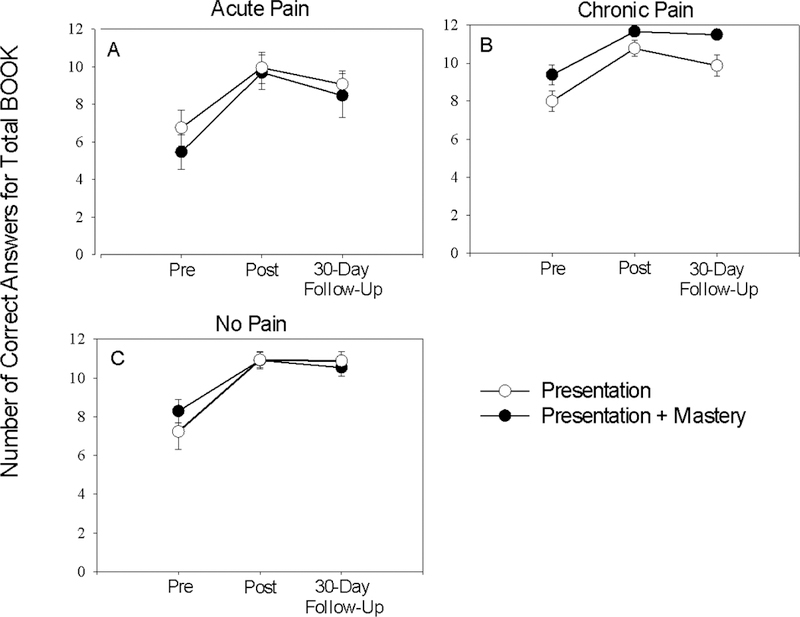
Brief Opioid Overdose Knowledge (BOOK) Total Scores (Mean ± Standard Error; total possible range 0–12) Across Time Points among Individuals with Prescription Opioid Use and Acute Pain (A), Prescription Opioid Use and Chronic Pain (B), and Illicit Opioid Use with No Pain (C).
Table 2.
Scores and Subscores (M ± SD) from the BOOK Questionnaire by Pain Group and Intervention
| Total N = 119 |
Acute Pain n = 29 |
Chronic Pain n = 49 |
No Pain, Illicit Use n = 41 |
|||||
|---|---|---|---|---|---|---|---|---|
| Presentation (N=61) |
Presentation + Mastery (N=58) |
Presentation (n=16) |
Presentation + Mastery (n=13) |
Presentation (N=28) |
Presentation + Mastery (N=21) |
Presentation (N=17) |
Presentation + Mastery (N=24) |
|
| Total BOOK (Score range 0–12)1 | ||||||||
| Pre | 7.5 ± 3.4a | 8.0 ± 3.1a | 6.8 ± 3.81 | 5.5 ± 3.31 | 8.0 ± 3.0 | 9.4 ± 2.2 | 7.2 ± 3.9 | 8.3 ±3.0 |
| Post | 10.6 ± 2.5b | 10.9 ± 2.2b | 9.9 ± 3.31 | 9.7 ± 3.3 | 10.8 ± 2.3 | 11.7 ± 0.4 | 10.9 ± 1.7 | 10.9 ± 2.1 |
| 30-Day Follow-Up | 9.9 ± 2.8c | 10.3 ± 2.7c | 9.0 ± 2.91 | 8.5 ± 4.2 | 9.8 ± 3.1 | 11.5 ± 0.7 | 10.9 ± 2.0 | 10.5 ± 2.2 |
| General Opioid Knowledge (Score range 0–4)2 | ||||||||
| Pre | 2.7 ± 1.2a | 2.9 ± 1.3a | 2.5 ± 1.4 | 2.0 ± 1.4 | 2.8 ± 1.0 | 3.5 ± 0.8 | 3.0 ± 1.2 | 2.7 ± 1.4 |
| Post | 3.6 ± 0.8b | 3.7 ± 0.8b | 3.6 ± 0.7 | 3.0 ± 1.2 | 3.5 ± 0.7 | 3.9 ± 0.3 | 3.8 ± 0.3 | 3.8 ± 0.5 |
| 30-Day Follow-Up | 3.4 ± 1.0c | 3.4 ± 1.0c | 3.0 ± 1.2 | 2.7 ± 1.4 | 3.4 ± 0.9 | 3.8 ± 0.4 | 3.8 ± 0.3 | 3.5 ± 0.9 |
| Opioid Overdose Knowledge (Score range 0–4)2 | ||||||||
| Pre | 2.8 ± 1.3a | 2.9 ± 1.2a | 2.4 ± 1.5 | 2.1 ± 1.3 | 3.0 ± 1.2 | 3.1 ± 1.4 | 2.6 ± 1.4 | 3.1 ± 1.0 |
| Post | 3.5 ± 1.1b | 3.7 ± 0.7b | 3.4 ± 1.1 | 3.2 ± 1.4 | 3.6 ± 0.9 | 4.0 ± 0.0 | 3.5 ± 1.2 | 3.7 ± 0.7 |
| 30-Day Follow-Up | 3.3 ± 1.2c | 3.5 ± 1.0c | 2.9 ± 1.6 | 3.0 ± 1.4 | 3.3 ± 1.1 | 3.7 ± 0.6 | 3.6 ± 0.8 | 3.6 ± 0.9 |
| Opioid OD Response Knowledge (Score range 0–4)1 | ||||||||
| Pre | 2.0 ± 1.4a | 2.2 ± 1.4a | 1.8 ± 1.4 | 1.4 ± 1.4 | 2.8 ± 1.2 | 2.1 ± 1.2 | 1.9 ± 1.5 | 2.2 ± 1.4 |
| Post | 3.5 ± 1.0b | 3.5 ± 1.0b | 3.2 ± 1.4 | 3.2 ± 1.5 | 3.7 ± 0.5 | 3.6 ± 0.8 | 3.6 ± 0.9 | 3.5 ±1.0 |
| 30-Day Follow-Up | 3.3 ± 1.3b | 3.5 ± 1.0b | 3.0 ± 1.6 | 2.8 ± 1.6 | 4.0 ± 0.0 | 3.2 ± 1.4 | 3.5 ± 1.0 | 3.4 ± 0.9 |
Note. Superscript letters represent results from post-hoc analyses following a significant effect of Time, respectively; time points with letters in common are not significantly different from one another.
Superscript numbers on Total and subscale titles refer to a significant main effect of pain groups across the three time points. “1” denotes a significant difference between Acute Pain and Chronic Pain groups, “2” denotes a significant difference between Acute Pain and Chronic Pain and No Pain groups
There was a significant main effect of pain group on BOOK total scores, F(2, 113) = 7.0, p = .001, such that individuals with acute pain displayed significantly lower scores compared to the chronic pain participants across all time points (Figure 2). For the subscores, acute pain participants had lower general opioid and OD overdose knowledge subscores than the chronic and no pain groups, (Table 2) F(2, 113) = 8.0, p < .01, F(2, 113) = 10.6, p < .05, and lower scores relative to the chronic pain group on the OD response subscale, F(2, 113) = 3.5, p < .05 (Table 2). No Intervention x Pain group interactions were observed for the BOOK total or subscores (p’s > .05).
Total BOOK scores at pre-and post-intervention were significantly lower among participants who did not complete the 30-day follow-up (M= 7.7, SEM = 0.3) compared to those who did (M = 9.2, SEM = 0.2; F(1, 183) = 186.0, p < .05)
3.3. Changes in Risky Opioid Use
Chi-squared analyses indicated, regardless of intervention or pain group, significantly fewer participants reported using opioids alone in the 30 days after the intervention (37.8%) compared to the 30 days before the intervention (51.3%), χ2 (1) = 4.4, p = .03 (Figure 3). Likewise, chi-squared analyses indicated significantly fewer participants reported using alcohol concurrently with opioids 30 days after the intervention (20%) compared to the 30 days before the intervention (35%), χ2 (1) =6.1, p = .01. These results also did not vary as a function of intervention χ2 (1) = 1.4, p = .24. However, individuals with acute pain were less likely to use alcohol with opioids when compared to individuals with no pain and illicit opioid use (27.6% v. 39.0%), but were more likely to use alcohol with opioids compared to individuals with chronic pain (27.6% v. 17.3%) χ2 (2) = 10.6, p = .005 (Figure 3). There was no significant change in the frequency of individuals who used non-prescribed methadone in the 30 days after the intervention (5%) compared to the 30 days before the intervention (6%), χ2 (1) =0.1, p = .78.
Figure 3.
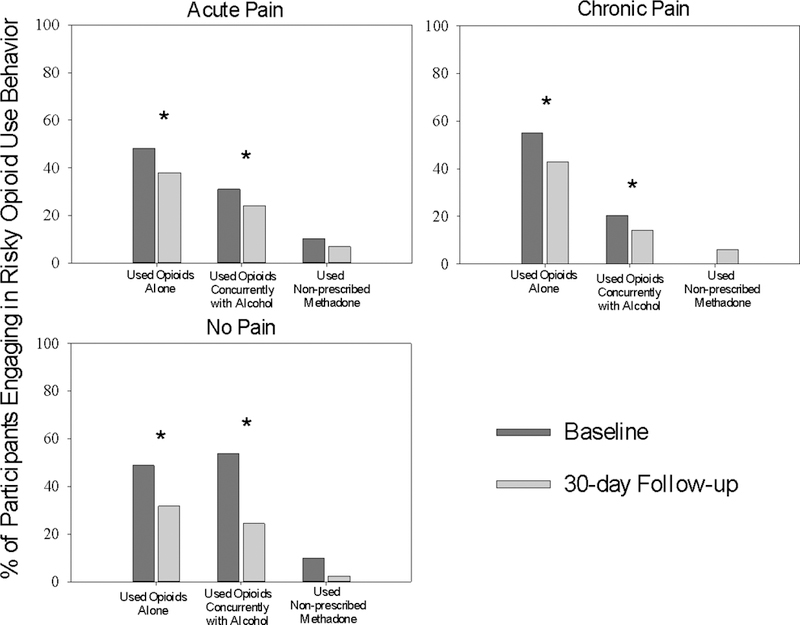
Percentage of participants in each Pain Group reporting risky opioid use behaviors in the 30 days prior to the intervention (Baseline) and in the 30 days after the intervention (30-day follow-up). Asterisks (*) indicate a significant change in the percentage of participants reporting risky opioid use behavior between the two time points, p < .05.
3.4. Acceptability
No significant differences in intervention acceptability were observed across any of the items between the Presentation and Presentation + Mastery groups (Table 3). Significantly more participants dropped out after initiating the Presentation + Mastery (37.2%) versus Presentation (16.8%) intervention, χ2 (1) =13.1, p < .001.
Table 3.
Acceptability of Intervention, % participants answering in the affirmative as a function of pain group
| Acute Pain n = 29 |
Chronic Pain n = 49 |
No Pain n = 41 |
p | |
|---|---|---|---|---|
| The educational intervention was helpful. | 90 | 96 | 93 | .56 |
| The educational intervention taught me information that I did not know before. | 83 | 88 | 90 | .65 |
| The educational intervention was easy to understand. | 79 | 100 | 95 | < .01 |
| The educational intervention was fun. | 41 | 63 | 56 | .16 |
| The educational intervention took too long. | 21 | 12 | 22 | .43 |
| The educational intervention was interesting. | 76 | 92 | 81 | .13 |
| I would recommend this educational intervention to someone else. | 66 | 90 | 81 | .03 |
| I believe that more people should receive this educational intervention. | 73 | 92 | 88 | .05 |
| I do NOT think the educational intervention was useful. | 10 | 2 | 5 | .27 |
| The educational intervention was confusing. | 7 | 4 | 5 | .86 |
| The educational intervention will help prevent you from overdosing. | 100 | 100 | 100 | - |
| The educational intervention will change the way you help other people who are overdosing. | 100 | 100 | 100 | - |
| I would recommend this intervention to a family member or friend. | 100 | 100 | 100 | - |
Note: p-values correspond to chi-squared tests that compared the proportion of affirmative responses to each statement across Pain Group. Intervention and Intervention X Pain Group effects did not have a significant impact on acceptability scores. Results were collapsed across Presentation and Presentation + Mastery conditions because no significant differences were observed between those groups.
Participants with acute pain were more likely to indicate that the interventions were not “Easy to Understand” (20.7%) compared to chronic pain (0.0%) and no pain groups (4.9%), χ2 (2) =12.8, p < .001. Acute pain participants were also more likely to indicate that they would not “recommend this educational intervention to someone else” (34.5%) compared to chronic pain (10.2%) and no pain (12.5%) participants. These acceptability responses, however, did not differ across intervention type within either population, p’s > .05. Dropout rates after initiating intervention did not differ across Pain Group, χ2 (2) = 2.1, p > .05.
4. Discussion
Interventions that mitigate morbidity and mortality are urgently needed to address the ongoing opioid crisis. Both two versions of the web-based intervention compared here immediately increased opioid OD knowledge and produced sustained knowledge gains 30-days later within three unique opioid-using populations. In addition, significantly fewer participants reported engaging in risky opioid-use related behaviors after completing either intervention. These findings support the use of remote, self-paced, web-based interventions for enhancing efforts to decrease opioid OD risk.
There were a few findings which should inform future applications of these computer-based interventions. First, participants who endorsed acute pain had markedly lower baseline opioid OD knowledge relative to other opioid-using populations across all tested time points. These findings are consistent with previous studies documenting lower baseline knowledge about opioid overdose among pain populations (Dunn et al., 2016; Dunn et al., 2017). Their unfamiliarity with all three opioid OD knowledge domains, paired with their comparable rates of risky opioid use behavior, suggests that individuals with acute pain who have opioid prescriptions may especially benefit from efforts to improve their opioid OD knowledge and might require supplemental educational resources to close the gap in opioid OD knowledge.
Second, despite both interventions being ranked favorably, attrition from the Presentation + Mastery condition was higher than from the Presentation condition. Since attrition was unrelated to demographics, it is likely that the additional burden imposed on participants by the Presentation + Mastery intervention (e.g., longer completion time, additional effort for embedded testing) may have contributed to greater dropout rates. The fact that the Presentation + Mastery version was associated with higher drop-out and took significantly longer for participants to complete but did not yield additional gains in knowledge suggests the Presentation version of this intervention appears to be the more practical option for dissemination.
To our knowledge, these web-based interventions are the first to demonstrate meaningful and sustained increases in opioid OD knowledge and to simultaneously target three unique populations of persons exposed to opioids who may be at heightened risk of OD. Other web-based interventions that successfully informed participants about OD did not assess knowledge at baseline, making the extent to which knowledge increased from those interventions unclear (Roe & Banta-Green, 2016; Simmons, Rajan, Goldsamt, & Elliott, 2016). In addition to knowledge, both interventions tested here were associated with decreases in self-reported risky opioid use behaviors. The fact that knowledge gains were retained and self-reported engagement in risk behaviors decreased by the 30-day follow-up increases confidence that the intervention may be an effective way of informing individuals about OD risks. Ideally, these interventions could complement other efforts to stem opioid overdose risk, including clinic-based screenings to identify participants at high risk for opioid misuse (Albert et al., 2011; Green et al., 2015; Strand, Eukel, & Burck, 2018) and the distribution of naloxone (Albert et al., 2011; Oliva et al., 2017; Walley et al., 2013). Importantly, unlike clinic-based screening or naloxone distribution, these interventions can be delivered with little burden on patients and providers and these initial data suggesting they may be associated with reductions in the frequency of high opioid overdose risk behavior suggests interventions such as this could be impactful.
This study has some limitations. First, although steps were taken to prevent, identify, and eliminate falsified responses, the online nature of the data collection prevents firm verification of participant characteristics and opioid use behaviors of the participants so results should be interpreted cautiously. Second, while the BOOK questionnaire is a brief measure of knowledge that covers important information related to opioid-overdose, it may not completely capture the full extent of knowledge deficits and/or gains either at baseline or from either version of the intervention; therefore, we can only conclude that our interventions perform equally according to the BOOK questionnaire. Third, the online nature of this study prevents us from objectively confirming risk behaviors or assessing whether participants can accurately respond to an OD using the techniques taught in the intervention. Furthermore, the unique demographics of online mTurk workers may limit the generalizability of these findings. Fourth, the scope of risky behaviors assessed in our study was somewhat limited. Therefore, future studies should include questions that assess other risky opioid use behaviors (e.g., using without access to naloxone, using in combination with other sedating drugs, using opioids while by themself) that could be influenced by these brief interventions. Fifth, future iterations should recruit enough participants to be adequately powered to detect differences across testing time points and populations. Our results suggests there are disparities in BOOK knowledge across groups which should be replicated and further characterized. Finally, it is unclear whether our overdose education materials where unique in their ability to reduce self-reported risk behaviors because both conditions were exposed to the same 25 slides. Future studies comparing the 25-slide manual to other overdose education materials would demonstrate the specific efficacy of our materials for reducing these behaviors. These limitations provide future research directions for the development and implementation of these web-based interventions.
In conclusion, this study demonstrated that a remote web-based intervention effectively increased opioid OD knowledge and decreased some OD-risk behaviors in three opioid-using populations who have unique risks for experiencing an opioid OD. This study extends upon previous studies (Dunn et al., 2017; Huhn et al., 2018) and suggests the Presentation version of this intervention may be of particularly value because it is a brief, user-friendly, well-accepted and recommended by participants, low burden, and scalable approach that could have significant public health impact by reducing opioid OD risk in persons who are managing their acute or chronic pain with an opioid prescription and have no pain and are using opioids illicitly.
5. References
- Albert S, Brason FW 2nd, Sanford CK., Dasgupta N, Graham J., & Lovette B. (2011). Project Lazarus: community-based overdose prevention in rural North Carolina. Pain Med, 12 Suppl 2, S77–85. doi: 10.1111/j.1526-4637.2011.01128.x [DOI] [PubMed] [Google Scholar]
- Brat GA, Agniel D, Beam A, Yorkgitis B, Bicket M, Homer M, … Kohane I. (2018). Postsurgical prescriptions for opioid naive patients and association with overdose and misuse: retrospective cohort study. Bmj, 360, j5790. doi: 10.1136/bmj.j5790 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buhrmester M, Kwang T, & Gosling SD (2011). Amazon’s Mechanical Turk: A New Source of Inexpensive, Yet High-Quality, Data? Perspect Psychol Sci, 6(1), 3–5. doi: 10.1177/1745691610393980 [DOI] [PubMed] [Google Scholar]
- Calcaterra SL, Yamashita TE, Min SJ, Keniston A, Frank JW, & Binswanger IA (2016). Opioid Prescribing at Hospital Discharge Contributes to Chronic Opioid Use. J Gen Intern Med, 31(5), 478–485. doi: 10.1007/s11606-015-3539-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler J, & Shapiro D (2016). Conducting Clinical Research Using Crowdsourced Convenience Samples. Annu Rev Clin Psychol, 12, 53–81. doi: 10.1146/annurev-clinpsy-021815-093623 [DOI] [PubMed] [Google Scholar]
- Cleeland CS, & Ryan KM (1994). Pain assessment: global use of the Brief Pain Inventory. Ann Acad Med Singapore, 23(2), 129–138. [PubMed] [Google Scholar]
- Dunn KE, Barrett FS, Fingerhood M, & Bigelow GE (2017). Opioid Overdose History, Risk Behaviors, and Knowledge in Patients Taking Prescribed Opioids for Chronic Pain. Pain Med, 18(8), 1505–1515. doi: 10.1093/pm/pnw228 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn KE, Barrett FS, Yepez-Laubach C, Meyer AC, Hruska BJ, Sigmon SC, … Bigelow GE. (2016). Brief Opioid Overdose Knowledge (BOOK): A Questionnaire to Assess Overdose Knowledge in Individuals Who Use Illicit or Prescribed Opioids. J Addict Med, 10(5), 314–323. doi: 10.1097/adm.0000000000000235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dunn KE, Yepez-Laubach C, Nuzzo PA, Fingerhood M, Kelly A, Berman S, & Bigelow GE (2017). Randomized controlled trial of a computerized opioid overdose education intervention. Drug Alcohol Depend, 173 Suppl 1, S39–s47. doi: 10.1016/j.drugalcdep.2016.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dworkin J, Hessel H, Gliske K, & Rudi JH (2016). A Comparison of Three Online Recruitment Strategies for Engaging Parents. Fam Relat, 65(4), 550–561. doi: 10.1111/fare.12206 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Green TC, Bowman S, Davis C, Los C, McHugh K, & Friedmann PD (2015). Discrepancies in addressing overdose prevention through prescription monitoring programs. Drug Alcohol Depend, 153, 355–358. doi: 10.1016/j.drugalcdep.2015.05.009 [DOI] [PubMed] [Google Scholar]
- Hedegaard H, Minino AM, & Warner M (2018). Drug Overdose Deaths in the United States, 1999–2017. NCHS Data Brief(329), 1–8. [PubMed] [Google Scholar]
- Huhn AS, Garcia-Romeu AP, & Dunn KE (2018). Opioid Overdose Education for Individuals Prescribed Opioids for Pain Management: Randomized Comparison of Two Computer-Based Interventions. Front Psychiatry, 9, 34. doi: 10.3389/fpsyt.2018.00034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson MJ, & Jiang L (2017). Reaping the benefits of meaningful work: The mediating versus moderating role of work engagement. Stress Health, 33(3), 288–297. doi: 10.1002/smi.2710 [DOI] [PubMed] [Google Scholar]
- Jones JD, Roux P, Stancliff S, Matthews W, & Comer SD (2014). Brief overdose education can significantly increase accurate recognition of opioid overdose among heroin users. Int J Drug Policy, 25(1), 166–170. doi: 10.1016/j.drugpo.2013.05.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krebs P, Prochaska JO, & Rossi JS (2010). A meta-analysis of computer-tailored interventions for health behavior change. Prev Med, 51(3–4), 214–221. doi: 10.1016/j.ypmed.2010.06.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mortensen K, Alcala MG, French MT, & Hu T (2018). Self-reported Health Status Differs for Amazon’s Mechanical Turk Respondents Compared With Nationally Representative Surveys. Med Care, 56(3), 211–215. doi: 10.1097/mlr.0000000000000871 [DOI] [PubMed] [Google Scholar]
- Oliva EM, Christopher MLD, Wells D, Bounthavong M, Harvey M, Himstreet J, … Trafton JA (2017). Opioid overdose education and naloxone distribution: Development of the Veterans Health Administration’s national program. J Am Pharm Assoc (2003), 57(2s), S168–S179.e164. doi: 10.1016/j.japh.2017.01.022 [DOI] [PubMed] [Google Scholar]
- Poquet N, & Lin C (2016). The Brief Pain Inventory (BPI). J Physiother, 62(1), 52. doi: 10.1016/j.jphys.2015.07.001 [DOI] [PubMed] [Google Scholar]
- Roe SS, & Banta-Green CJ (2016). An Initial Evaluation of Web-Based Opioid Overdose Education. Subst Use Misuse, 51(2), 268–275. doi: 10.3109/10826084.2015.1092986 [DOI] [PubMed] [Google Scholar]
- Simmons J, Rajan S, Goldsamt L, & Elliott L (2016). Implementation of online opioid overdose prevention, recognition and response trainings for professional first responders: Year 1 survey results. Drug Alcohol Depend, 169, 1–4. doi: 10.1016/j.drugalcdep.2016.10.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strand MA, Eukel H, & Burck S (2018). Moving opioid misuse prevention upstream: A pilot study of community pharmacists screening for opioid misuse risk. Res Social Adm Pharm. doi: 10.1016/j.sapharm.2018.07.011 [DOI] [PubMed] [Google Scholar]
- Strickland JC, & Stoops WW (2019). The use of crowdsourcing in addiction science research: Amazon Mechanical Turk. Exp Clin Psychopharmacol, 27(1), 1–18. doi: 10.1037/pha0000235 [DOI] [PubMed] [Google Scholar]
- Walley AY, Xuan Z, Hackman HH, Quinn E, Doe-Simkins M, Sorensen-Alawad A, … Ozonoff A (2013). Opioid overdose rates and implementation of overdose education and nasal naloxone distribution in Massachusetts: interrupted time series analysis. Bmj, 346, f174. doi: 10.1136/bmj.f174 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walters K, Christakis DA, & Wright DR (2018). Are Mechanical Turk worker samples representative of health status and health behaviors in the U.S.? PLoS One, 13(6), e0198835. doi: 10.1371/journal.pone.0198835 [DOI] [PMC free article] [PubMed] [Google Scholar]


