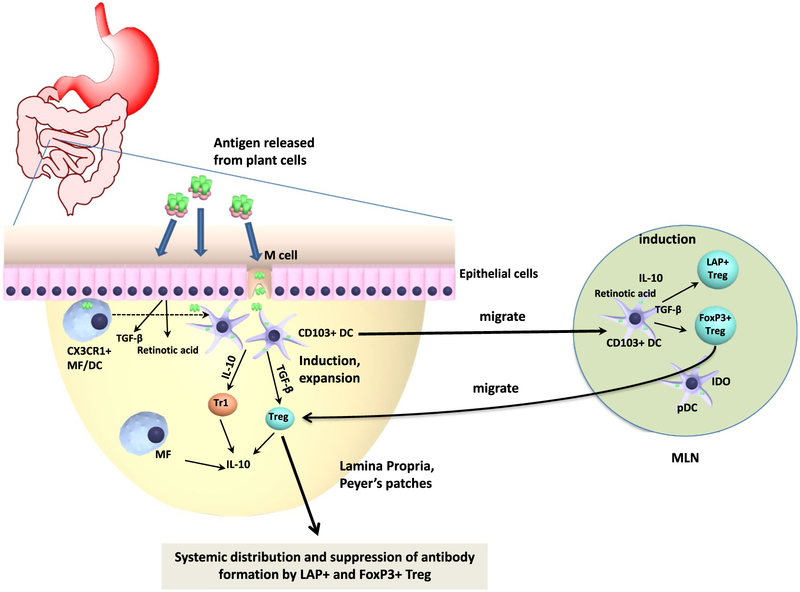
Fig. 5.
Detailed immunological mechanism of oral tolerance induction. Antigens released from plant cells in the small intestine upon oral administration are taken up by epithelial and M cells, followed by transmucosal delivery. Dendritic cells (DCs) may take up transcytosed antigen, sample antigen directly from the gut lumen, or acquire antigen initially taken up by CX3CR1+ macrophages (MF). Ultimately, antigen-loaded CD103+ DCs migrate to mesenteric lymph nodes (MLN) and present the acquired antigen to CD4+ T cells while producing TGF-β and retinoic acid, resulting in induction of Treg. Plasmacytoid DCs (pDCs) may enhance Treg induction. Upon migration back to the lamina propria, induced Treg further expand. The cytokines TGF-β and IL-10 are critical to Treg induction. Peripheral induction of FoxP3+ and of LAP+ Treg is TGF-β dependent, while IL-10 may enhance induction of Tr1 cells. IL-10 is crucial in preventing chronic inflammation in the gut and for the immune suppressive function of Treg on mucosal interfaces. Induced FoxP3+ and LAP+ Treg systemically distribute to lymphoid organs outside the gut immune system, such as the spleen, and suppress T cell responses and antibody formation.