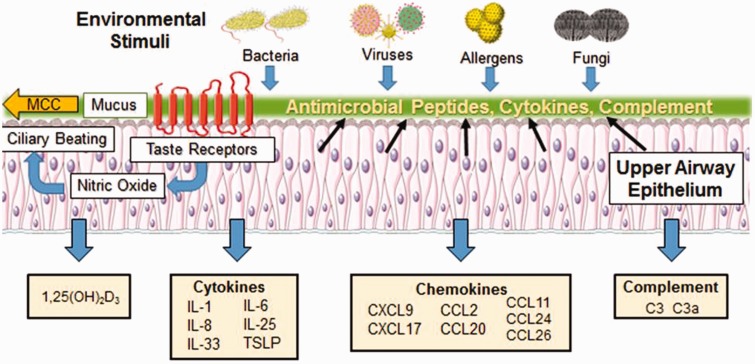
Figure 1.
Immune functions of the upper airway epithelium. The upper airway epithelium is a key player in both innate and adaptive immunity and serves as the first line of defense against allergens, pathogens, and pollutants inhaled from the external environment. The epithelium kills or neutralizes inhaled microorganisms through the release of AMPs and coordinates the clearance of inhaled irritants trapped by mucus via ciliary beating in the process of mucociliary clearance (MCC). Stimulation of taste receptors expressed on epithelial cells by bitter bacterial compounds enhances the release of AMPs and triggers the production of nitric oxide which increases ciliary beat frequency, enhancing the dispersion of AMPS and improving MCC. The pseudostratified ciliated columnar epithelial cells joined by tight junctions, adherens junctions, gap junctions, and desmosomes also serve as a physical barrier that blocks inhaled irritants from passing through to the subepithelial space below. Exposure to foreign substances triggers epithelial release of inflammatory cytokines that influence T-cell, dendritic cell (DC), and eosinophil function. The epithelium is also a rich source of numerous chemokines that modulate T-cell, DC, and eosinophil activity. In addition, the epithelium is a local source of 1,25(OH)D3 and complement proteins C3 and C3a which play critical roles in innate and adaptive immune responses. Alterations to these epithelial functions are closely intertwined with the pathogenesis of chronic rhinosinusitis with nasal polyps.