Abstract
Revision quadriceps tendon repair presents a challenging problem for the treating surgeon because of associated anatomic defects such as large tendon-gap deficits and preexistent poor tissue quality. Current methods for revision quadriceps tendon repair use tendon autograft, which may predispose to additional morbidity because the repair relies only on soft tissue fixation. In this Technical Note, we describe a technique for revision of a failed quadriceps tendon repair with a large tendon gap using a trapezoidal plug Achilles tendon allograft. This technique constitutes a safe and effective approach to revising failed primary quadriceps tendon repairs, is suitable for large-gap defects, and has the ability to withstand large force transmissions.
Revision quadriceps tendon repairs present a challenging scenario for the treating surgeon. Indeed, rerupture of the quadriceps tendon often presents in conjunction with muscle atrophy, decreased bone stock, and complex tendon defects with associated retraction, which may leave a large tendon-gap deficit and increase the difficulty of the repair.1, 2 Despite the understanding of such challenges, there remains a paucity of efficacious surgical approaches that provide adequate stability and restoration of function after revision of these failures.
A case report by McCormick et al.1 in 2013 described a novel open-incision technique that used bilateral hamstring autografts through a quadriceps tendon weave and transosseous patellar repair to address a failed quadriceps tendon repair. Likewise, Rehman and Kovacs2 described a novel repair technique in which they used a hamstring autograft with a prolene mesh and platelet-rich plasma. Despite both studies reporting satisfactory outcomes at short-term follow-up, these techniques likely impart the potential for associated morbidity, as they depend on extensive harvesting of autologous tendons and the use of mesh. As such, a surgical approach that uses allograft may be an efficacious alternative with the benefit of avoiding such risks.
We describe a technique for revision of a failed quadriceps tendon repair with a large tendon gap using a trapezoidal plug Achilles tendon allograft. This technique constitutes a safe and effective approach to revising failed primary quadriceps tendon repairs, is suitable for large-gap defects, and has the ability to withstand large force transmissions.
Objective Diagnosis
Preoperative radiographs should include standing anteroposterior, lateral, long-axis weightbearing, 45° posteroanterior flexion weightbearing, and patellofemoral (sunrise) views. Additionally, preoperative magnetic resonance imaging is helpful to determine the status of the remaining tissue, retraction of the proximal stump, and associated soft tissue pathology.
Surgical Technique
Patient Positioning and Anesthesia
The patient is placed in the supine position on the operating table, and general anesthesia is used for induction. A well-padded high-thigh tourniquet is subsequently placed on the operative leg, and a bump is placed under the knee so that it rests at ∼30° flexion. The contralateral leg is secured to the table in full extension with a pneumatic compression device to help prevent deep venous thrombosis (Video 1). Table 1 outlines the step-by-step approach to performing the technique, and pearls and pitfalls of the technique are listed in Table 2.
Table 1.
Step-by-Step Technique for Quadriceps Tendon Repair With Large Tendon Defects
| 1. Patient positioning with knee in 20° flexion |
| 2. Midline approach extending from 2 cm proximal to palpable defect to distal patella |
| 3. Subcutaneous dissection and tendon exposure |
| 4. Identification of the gap, debridement of nonviable tissue |
| 5. Preparation of a trapezoidal recipient site in the native patella |
| 6. Drilling of two 2.4-mm tunnels in the patella deeper than the previously created socket; Kirschner wire passage |
| 7. Preparation of an Achilles tendon bony allograft on the back table to match the inverted trapezoidal shape created in the patella |
| 8. Allograft insertion and fixation with Kirschner wires |
| 9. Side-to-side native tendon–allograft suture |
| 10. Layered closure |
Table 2.
Pearls and Pitfalls of the Trapezoidal Achilles Tendon Allograft Plug for Revision Quadriceps Tendon Repair
| Pearls | Pitfalls |
|---|---|
| Care should be taken to place the leg holder as proximal as possible to allow for proper visualization. | Placement of the leg holder too distal can limit visualization of the entire quadriceps tendon. |
| Optimal exposure of the distal aspect of the tendon allows for a better understanding of the tissue gap within the quadricipital tendon that needs to be addressed. | Failing to identify the gaps or nonfunctional tissue can result in suboptimal postoperative outcomes. |
| The patella should be prepared first to determine a perfect match on the graft after it has been defined. A proximal bony wall of ∼2 mm should be left intact to avoid proximal migration of the graft and to improve fixation. | If the proximal bony wall fractures, fixation could be severely compromised. |
| When drilling the two 2.4-mm tunnels in the patella for Kirschner wire passage, ensure that position is centered in the socket, superficial to cartilaginous surface. | Improper orientation of the Kirschner wire anchors can lead to damage of the articular surface of the patella. |
| Before skin closure, the knee should be taken through gentle passive range of motion to determine degrees of flexion that should be allowed postoperatively. | Avoid overconstraining with the incorporation of the allografts in the quadriceps tendon reconstruction. |
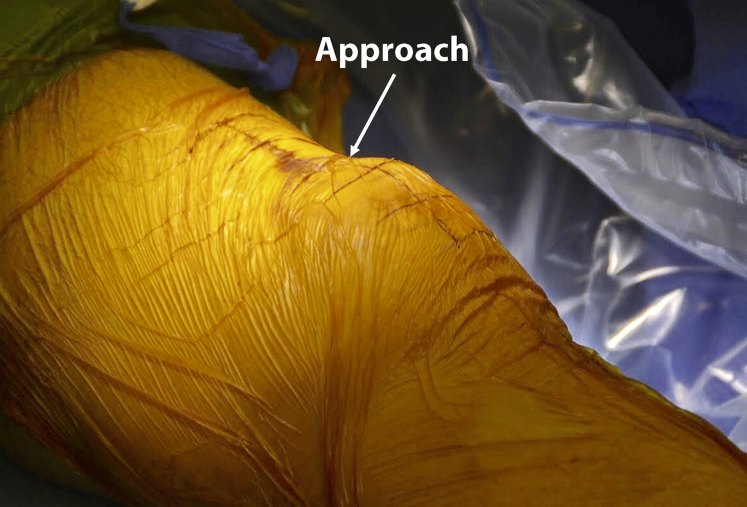
Approach
An 8-cm midline incision is created. Proximally, the incision is made 2 cm proximal to the distal aspect of the previously identified tendon stump. This incision is extended distally to the distal pole of the patella(Fig 1). Blunt dissection is performed down to the quadriceps tendon layer while performing watchful inspection to precisely identify all injured structures. At this point, the hematoma is evacuated and the joint copiously irrigated. Next, extensive debridement of the nonviable tissue is performed. All adhesions should be released, and planes should be reestablished.
Fig 1.
Markings depicting extent of midline incision on a left knee. The markings are approximated to begin 2-cm proximal to the distal aspect of the previously identified tendon gap/stump (top), and the distal end of the markings approximates the distal pole of the patella (bottom).
The superior pole of the patella should be debrided of any remaining tendon with the use of a curette, rongeur, or burr to expose cancellous bleeding bone. Next, 2 double-loaded 3.5-mm suture anchors (Arthrex, Naples, FL) are placed equidistant from the midline into the proximal patella. Sutures are passed through the full thickness of the medial and lateral aspects of the remaining quadriceps tendon using a Krackow stitch. After the anatomic reduction of the remaining tendon, usually the medial and lateral aspects, the central gap is identified.
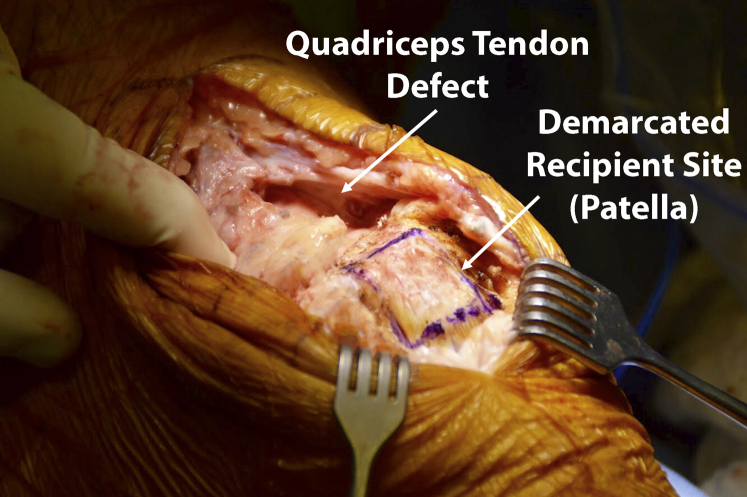
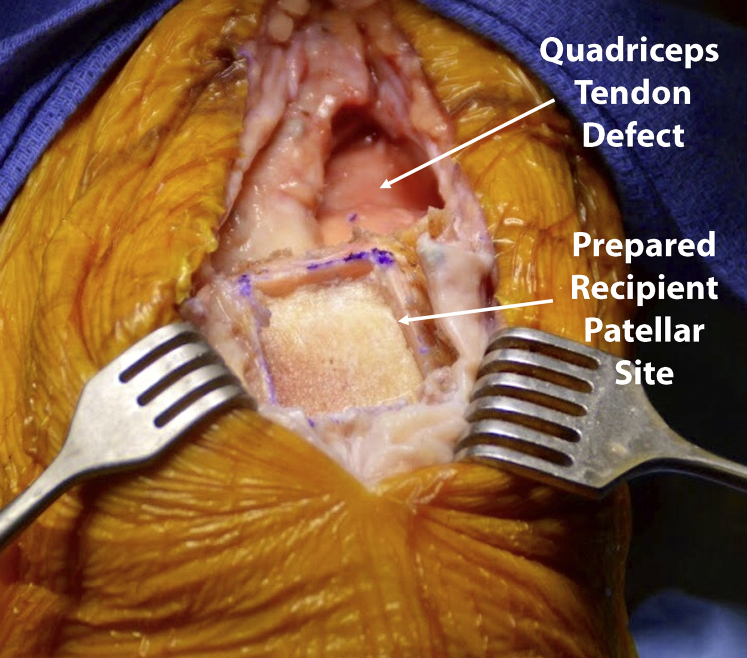
Patellar Preparation
After obtaining full visualization of the patella, an inverted trapezoidal-shaped cut is planned with a marking pen (Fig 2). The boundaries of the trapezoid are composed of a 2-mm distal segment of the proximal aspect of the patella and proximal wall and a 22-mm apex that widens to 28 mm at the base distally. An oscillating saw is used to create the previously delineated trapezoidal slot, which is shallower distally and deeper proximally. The proximal patellar wall serves as a mechanical block to prevent slippage of the graft proximally (Fig 3).
Fig 2.
Full visualization of patella after creation of the midline approach on a left knee. A marking pen has been used to plan an inverted, trapezoidal shaped cut in the patella.
Fig 3.
Intraoperative image of the proximal patellar wall (on a left knee) with two 2.4-mm tunnels drilled medially to laterally and two 18-gauge metal wires inserted transversely through the tunnels. This aspect of the patella is used to prevent slippage of the Achilles tendon graft proximally, and the wires confer additional anteroposterior fixation of the graft.
Next, two 2.4-mm tunnels are drilled medially to laterally, ensuring that the articular surface, proximal anchors, and slot are not violated. Two 18-gauge metal wires are then inserted into these holes in a transverse fashion for additional anteroposterior fixation of the graft (Fig 3).
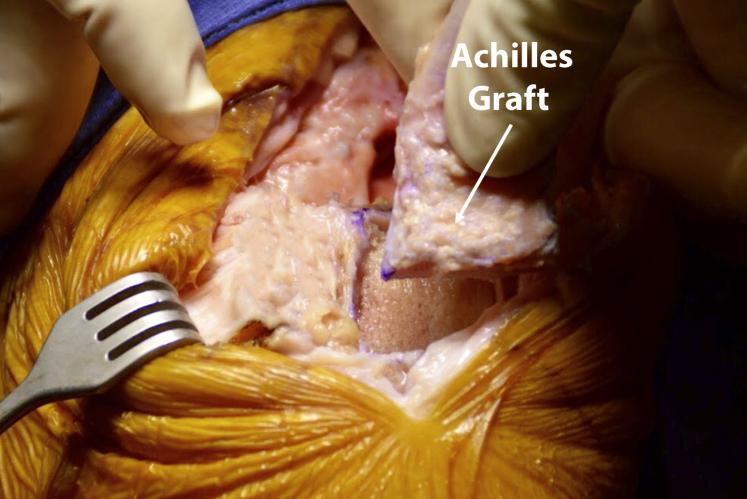
Graft Preparation and Fixation
An Achilles allograft is fashioned to the size of the recipient bone. The final product should be a trapezoidal-shaped graft 6 to 7 mm in depth proximally to 2 to 3 mm distally. The Achilles tendon can be shaped accordingly to the defect, or it can be shaped in situ if needed to avoid mismatch of the graft (Fig 4).
Fig 4.
Placement of trapezoidal Achilles graft into the recipient site (left patella). Note the matching/corresponding surfaces.
The graft is inserted into the created slot, ensuring that good congruence has been reestablished. The wires are then crossed over the graft, pulled, and twisted to improve axial compression of the graft (Fig 5). It is important to have the graft held in place for adequate reduction while tightening the wires. The graft is then trialed into the central gap defect and sutured side to side with N2 FiberWire (Arthrex) (Fig 6). The remaining proximal Achilles collagen graft can be then flipped over itself distally again if needed to cover any remaining defects. The medial and lateral retinaculum are also closed with N2 FiberWire.
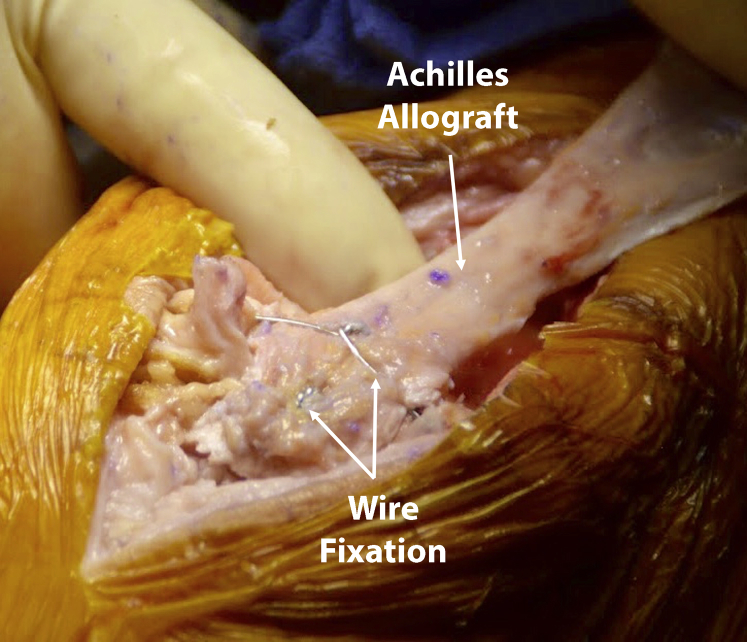
Fig 5.
Insertion of Achilles graft with wires crossed and fixed to graft to augment axial compression within the defect on a left knee.
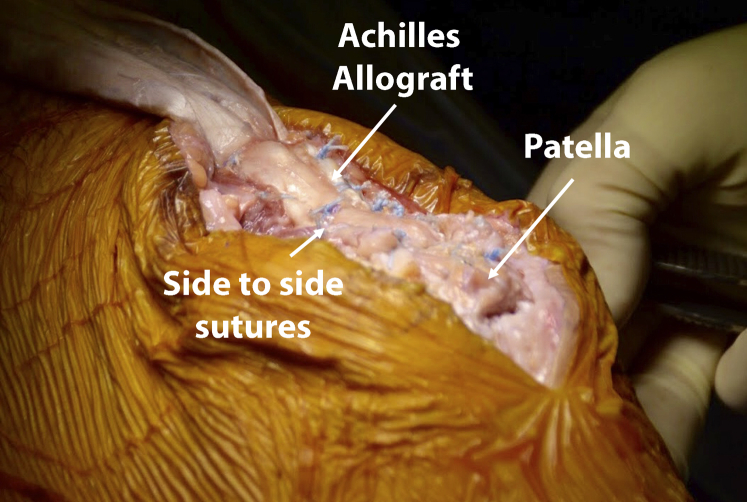
Fig 6.
Achilles graft position within gap defect after fixation with side-to-side suturing on a left knee.
Closure
Postsurgical care and appropriate parameters and limitations of activities are critical to recovery and the success of the procedure. Before complete subcutaneous closure, the knee should be flexed under direct visual inspection to assess to what degree the knee can be mobilized before repair, and graft augmentation is brought to tension. The acquisition of this information will assist in setting limitations of range of motion for the first 2 weeks postoperatively. Subcutaneous tissue and skin are closed in a layered fashion.
Rehabilitation
Postsurgical rehabilitation is divided into 4 phases (Table 3). Phases I and II are the most protected. In phase I, the patient is placed in a postsurgical hinged knee brace that is capable of both adjustable range of motion and locking. In the immediate postsurgical phase, the patient is required to use the brace at all times except when performing hygiene and during selected exercises for 2 weeks. Exercises can be performed independently and are initiated within 24 hours of surgery. Patients benefit from visual guidance on the exercises. Encouragement of restricted movement is paramount in the aversion of postsurgical stiffness, muscle atrophy, and complications of thromboembolic events. Thus, the patient is additionally placed on oral anticoagulation and restricted from air travel for 5 days.
Table 3.
Quadriceps Tendon Repair Rehabilitation Protocol
| Phase | WB | Brace | Range of Motion | Exercises |
|---|---|---|---|---|
| I, 0 to 2 wk | As tolerated with crutches and brace | Locked in full extension for sleeping and all activity; off for exercises and hygiene | 0° to 45° when non-weightbearing | Heel slides, quad sets, patellar mobs, SLRs, calf pumps |
| II, 2 to 8 wk | Full WB while in brace | 2 to 4 wk: locked in full extension day and night 4 to 6 wk: off at night; locked in full extension daytime 8 wk: discontinue brace |
2 to 3 wk: 0° to 60° 3 to 4 wk: 0° to 90° 4 to 8 wk: progress slowly as tolerated; refer to physical therapist for restrictions |
Advance phase I exercises Add side-lying hip/core/glutes Begin WB calf raises No WB with flexion >90° Progress slowly as tolerated; refer to physical therapist for restrictions |
| III, 8 to 12 wk | Full | None | Full | Progress closed-chain activities Begin hamstring work, lunges/leg press 0° to 90°, proprioception exercises, balance/core/hip/glutes Begin stationary bike when able |
SLR, straight leg raise; WB, weightbearing.
Phase II goals include increased range of motion, continued improvement in muscle recruitment, reduction of swelling, and increased tolerance of weightbearing time. Progressive mobility is achieved through incremental increases in range of motion of 15° on a weekly to biweekly basis for progressive tolerance of the repair. Avoidance of weight flexion during this phase is important to protect from incidental trauma by abrupt flexion or recruitment of avulsing muscle forces.
At phases III and IV, the patient is advanced from closed chain and proprioceptive activities at week 8 to higher-level movement such as single-leg balance, eccentric exercises, bike, and elliptical by week 12. In the last phase, IV, the patient progressively advances motor function and is typically cleared to incorporate high-impact activities such as running, jumping, and explosive maneuvers at 20 weeks postsurgery.
The capabilities of each patient may vary drastically, and thus each rehabilitation process may be modified. The patient's comorbidities and healing potential should be considered in the recovery process. This may require a longer recovery process and prolonged use of brace and crutches.
Discussion
Among knee extensor mechanism injuries, the quadriceps tendon is the most commonly disrupted segment. Rerupture of a primary quadriceps repair can be devastating to the patient, given the associated morbidity and functional deficits. Such cases require revision with grafting to restore independent movement and strength. The inherent difficulty in correcting associated large-gap deficits during revision quadriceps repairs, in addition to atrophy of the surrounding muscle and soft tissue and poor bone stock, are important considerations for the treating surgeon, and an appropriate surgical approach capable of overcoming these challenges must be used. The technique described here, which uses a trapezoidal Achilles tendon allograft plug, provides appropriate correction of such gap deficits while minimizing morbidity and restoring the extensor mechanism.
The most common cause of both partial- and full-thickness quadriceps ruptures is trauma secondary to eccentric loading of the knee extensor mechanism, although various systemic conditions such as diabetes mellitus and hyperparathyroidism have been linked to a predisposition for tendon rupture.3, 4, 5 Additionally, quadriceps ruptures may manifest from iatrogenic causes of quadriceps pathology such as a history of total knee arthroplasty (TKA), revision TKA, intra-articular corticosteroid injections, systemic steroid use, and extensile approaches used in the setting of revision or obesity.4, 6 There is limited evidence suggesting that early repair of a primary quadriceps tendon rupture may allow for good short- and mid-term outcomes,7 whereas others have reported variable postoperative improvements.8 Although no single technique has been determined as superior for repair of these defects, quadriceps tendon reconstruction with augmentation has been associated with fewer complications and better postoperative outcomes compared with simple suture repair.9 With regard to quadriceps tendon rerupture, the complexity of anatomic defects and lack of clinical and biomechanical outcomes data make it unclear as to which method provides optimal restoration of function. Therefore, there is a need for the development of surgical techniques that take into consideration the challenges inherent in revision quadriceps repairs that are not present in primary quadriceps repairs.
Traditionally, revision quadriceps tendon repairs have used methods of tendon fixation consisting of tendon lengthening and reconstruction with autologous graft; however, this may be associated with additional morbidity. Novel methods of fixation, such as allograft, synthetic mesh, and/or biologic augmentation (platelet-rich plasma or bone marrow aspirate concentrate) are now potential options for revision of quadriceps tendon rupture and may confer lower morbidity profiles while maintaining comparable knee stability. Augmentation procedures using allograft tissue, as described in this technique, have been postulated to offer a potential improvement in surgical outcomes while minimizing morbidity associated with autograft harvesting. Achilles tendon allograft (Achilles tendon-calcaneal bone block) has been previously described as an effective technique for primary reconstruction of the extensor mechanism. Wise et al.10 reported on 17 knee extensor mechanism reconstructions with Achilles tendon allograft after TKA. The 17 reconstructions consisted of 10 patellar tendons and 7 quadriceps tendon ruptures, and the entire extensor mechanism was repaired in all cases. They reported an average extensor lag and knee flexion of 8.4° and 107.9°, respectively, and only 1 rerupture. Furthermore, quadriceps strength was maintained at an average of 4 out of 5 at 2 years postoperatively.10 There are currently no studies that report on outcomes after Achilles tendon repair for isolated quadriceps deficit.
Although beyond the scope of this technical report, it is worth noting that synthetic substitutes for extensor mechanism repair have also shown promising results in return to function while presenting a cheaper alternative without the risk of disease transmission that is present with allograft tissue.11 Morrey et al.11 described the use of a Marlex mesh construct used for acute and subacute primary quadricep tendon repairs in 7 patients. At a mean follow-up of 9 years, the authors reported that no patients required reoperations or had evidence of extensor lag. Furthermore, these patients had a mean flexion of 100° at latest follow-up.11 Together, these data suggest that synthetic constructs may provide durable results with good clinical outcomes; however, further studies are required to evaluate the efficacy of a mesh in isolated quadriceps tendon deficiency in the setting of revision surgery.
Using a trapezoidal Achilles allograft bone plug for an isolated revision quadriceps tendon repair allows for some advantages (Table 4). One advantage is that the trapezoidal bone block provides a hard fixation point that keys into the patella, as opposed to relying on soft tissue adherence. Moreover, as it is an allograft, there is decreased morbidity associated with autograft harvesting. Potential risks and limitations with the use of this repair method primarily manifest from the limited available literature reporting on the clinical outcomes of allograft quadriceps repair in the setting of a previous graft failure using the current technique. Other potential disadvantages and risks with this technique include the following: 1) it is a technically challenging patellar preparation and bone plug creation method, which may limit its use; (2) there is potential for graft mismatch during allograft preparation and insertion, which may lead to graft laxity, overconstraint, or an extensor lag; and (3) there is potential for inadequate reduction within the created defect while tightening the metal wires and simultaneously attempting to stabilize the graft, which may lead to a poor outcome if not performed properly.
Table 4.
Advantages and Disadvantages of the Trapezoidal Achilles Tendon Allograft Plug for Revision Quadriceps Tendon Repair
| Advantages | Disadvantages |
|---|---|
| Minimally invasive | Technically challenging |
| Can be used when poor soft tissue adherence is a concern | Limited data on outcomes |
| Suitable for large tendon-gap defects | Potential for inadequate reduction within the created defect while tightening the metal wires and simultaneously attempting to stabilize the graft |
| Avoids additional morbidity by using allograft as opposed to autograft | Potential for graft mismatch during allograft preparation and insertion |
Conclusions
Additional research is required to determine if these promising initial findings present a solution to this difficult problem. This technique offers a suitable method for a minimally invasive, durable quadriceps tendon repair when there is a large-gap defect and concern for poor soft tissue adherence.
Footnotes
The authors report the following potential conflicts of interest or sources of funding: C.A.B-J. reports other from Cresco Lab. B.J.C. reports other from Aesculap/B.Braun, Athletico, JRF Ortho, National Institutes of Health (National Institute of Arthritis and Musculoskeletal and Skin Diseases, National Institute of Child Health and Human Development), Ossio, Regentis, Smith & Nephew; personal fees from Arthrex, Inc., Elsevier Publishing, Operative Techniques in Sports Medicine. Full ICMJE author disclosure forms are available for this article online, as supplementary material.
Supplementary Data
The quadriceps defect is evaluated preoperatively on a left knee. The vastus medialis and vastus lateralis should be interrogated, and the tendons should be intact, inserting on the patella. The stepoff is marked out to show the size of the central quadriceps defect and plan the incision. An 8-cm midline incision is performed, 2 cm proximal to the distal aspect of the previously identified tendon gap and extending distally to the distal pole of the patella. The ruptured quadriceps tendon is dissected out, taking care to respect tissue planes and preserve viable tissue. Adhesions are released. An inverted trapezoidal-shaped patellar cut is planned. The proximal edge of the cut should traverse the patella 2 mm distal to the proximal aspect of the patella and should be 22 mm in width. This widens to 28 mm at the distal aspect of the patella. A size-matched cut is planned on the surface of the Achilles allograft bone segment. The graft can be shaped in situ if needed to avoid mismatch of the graft. An oscillating saw is used to perform the cuts along the well-demarcated lines previously inscribed on the calcaneal allograft. Curved Mayo scissors are used to free the appropriately sized allograft from excess tissue. The depth of the allograft is marked before making the cut with an oscillating saw. The final product should be 6 to 7 mm deep in the proximal aspect of the graft and 2 to 3 mm deep in the distal aspect. This can be altered in situ if needed to achieve implant congruency. The patella is cut along the previously delineated trapezoidal slot using an oscillating saw. The patella is cut at a slope, with the proximal aspect cut deeper and the distal aspect cut shallower to create a mechanical block to prevent slippage of the graft proximally. Two 2.4-mm tunnels are drilled through the patella medially to laterally, taking caution not to violate the articular surface, proximal anchors, or slot. Two 18-gauge metal wires are inserted into these holes in a transverse fashion. These will serve as additional anteroposterior fixation of the graft. The size-matched Achilles graft is inserted into the recipient graft site, ensuring that good congruence has been reestablished. The wires are crossed over the graft, pulled, and twisted to improve axial compression of the graft. The graft must be held in place for adequate reduction while tightening the wires. The wires are twisted to compress the graft at the implant site. Wire cutters are used to cut the twisted ends and bury them in adjacent tissue. The graft is trialed into the central gap defect and sutured side to side with N2 FiberWire (Arthrex). The excess Achilles collagen graft can be flipped over itself distally if needed to cover any remaining defects. When there is adequate coverage of the defect, the excess graft can be resected. The medial and lateral retinaculum are closed with N2 Fiberwire. Before complete subcutaneous closure, the knee is flexed under direct visual inspection to assess to what degree the knee can be mobilized before repair, and graft augmentation is brought to tension. The skin is closed in standard fashion.
References
- 1.McCormick F., Nwachukwu B.U., Kim J., Martin S.D. Autologous hamstring tendon used for revision of quadriceps tendon tears. Orthopedics. 2013;36:e529–e532. doi: 10.3928/01477447-20130327-36. [DOI] [PubMed] [Google Scholar]
- 2.Rehman H., Kovacs P. Quadriceps tendon repair using hamstring, prolene mesh and autologous conditioned plasma augmentation. A novel technique for repair of chronic quadriceps tendon rupture. Knee. 2015;22:664–668. doi: 10.1016/j.knee.2015.04.006. [DOI] [PubMed] [Google Scholar]
- 3.Ibounig T., Simons T.A. Etiology, diagnosis and treatment of tendinous knee extensor mechanism injuries. Scand J Surg. 2016;105:67–72. doi: 10.1177/1457496915598761. [DOI] [PubMed] [Google Scholar]
- 4.Seng C., Lim Y.J., Pang H.N. Spontaneous disruption of the bilateral knee extensor mechanism: A report of two cases. J Orthop Surg (Hong Kong) 2015;23:262–266. doi: 10.1177/230949901502300233. [DOI] [PubMed] [Google Scholar]
- 5.Torkaman A., Yousof Gomrokchi A., Elahifar O., Barmayoon P., Shojaei S.F. Simultaneous bilateral rupture of patellar tendons in diabetic hemodialysis patient: A case report. Caspian J Intern Med. 2018;9:306–311. doi: 10.22088/cjim.9.3.306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Coste M., Newman J.M., Shah N.V., Eldib A.M., Grieco P.W., Maheshwari A.V. Bilateral spontaneous quadriceps tendon ruptures after staged bilateral total knee arthroplasties: A case report. J Long Term Eff Med Implants. 2018;28:63–71. doi: 10.1615/JLongTermEffMedImplants.2018025731. [DOI] [PubMed] [Google Scholar]
- 7.Chhapan J., Sankineani S.R., Chiranjeevi T., Reddy M.V., Reddy D., Gurava Reddy A.V. Early quadriceps tendon rupture after primary total knee arthroplasty. Knee. 2018;25:192–194. doi: 10.1016/j.knee.2017.12.002. [DOI] [PubMed] [Google Scholar]
- 8.Nodzo S.R., Rachala S.R. Polypropylene meshaugmentation for complete quadriceps rupture after total knee arthroplasty. Knee. 2016;23:177–180. doi: 10.1016/j.knee.2015.09.007. [DOI] [PubMed] [Google Scholar]
- 9.Black J.C., Ricci W.M., Gardner M.J. Novel augmentation technique for patellar tendon repair improves strength and decreases gap formation: A cadaveric study. Clin Orthop Relat Res. 2016;474:2611–2618. doi: 10.1007/s11999-016-5009-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wise B.T., Erens G., Pour A.E., Bradbury T.L., Roberson J.R. Long-term results of extensor mechanism reconstruction using Achilles tendon allograft after total knee arthroplasty. Int Orthop. 2018;42:2367–2373. doi: 10.1007/s00264-018-3848-4. [DOI] [PubMed] [Google Scholar]
- 11.Morrey M.C., Barlow J.D., Abdel M.P., Hanssen A.D. Synthetic mesh augmentation of acute and subacute quadriceps tendon repair. Orthopedics. 2016;39:e9–e13. doi: 10.3928/01477447-20151218-02. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The quadriceps defect is evaluated preoperatively on a left knee. The vastus medialis and vastus lateralis should be interrogated, and the tendons should be intact, inserting on the patella. The stepoff is marked out to show the size of the central quadriceps defect and plan the incision. An 8-cm midline incision is performed, 2 cm proximal to the distal aspect of the previously identified tendon gap and extending distally to the distal pole of the patella. The ruptured quadriceps tendon is dissected out, taking care to respect tissue planes and preserve viable tissue. Adhesions are released. An inverted trapezoidal-shaped patellar cut is planned. The proximal edge of the cut should traverse the patella 2 mm distal to the proximal aspect of the patella and should be 22 mm in width. This widens to 28 mm at the distal aspect of the patella. A size-matched cut is planned on the surface of the Achilles allograft bone segment. The graft can be shaped in situ if needed to avoid mismatch of the graft. An oscillating saw is used to perform the cuts along the well-demarcated lines previously inscribed on the calcaneal allograft. Curved Mayo scissors are used to free the appropriately sized allograft from excess tissue. The depth of the allograft is marked before making the cut with an oscillating saw. The final product should be 6 to 7 mm deep in the proximal aspect of the graft and 2 to 3 mm deep in the distal aspect. This can be altered in situ if needed to achieve implant congruency. The patella is cut along the previously delineated trapezoidal slot using an oscillating saw. The patella is cut at a slope, with the proximal aspect cut deeper and the distal aspect cut shallower to create a mechanical block to prevent slippage of the graft proximally. Two 2.4-mm tunnels are drilled through the patella medially to laterally, taking caution not to violate the articular surface, proximal anchors, or slot. Two 18-gauge metal wires are inserted into these holes in a transverse fashion. These will serve as additional anteroposterior fixation of the graft. The size-matched Achilles graft is inserted into the recipient graft site, ensuring that good congruence has been reestablished. The wires are crossed over the graft, pulled, and twisted to improve axial compression of the graft. The graft must be held in place for adequate reduction while tightening the wires. The wires are twisted to compress the graft at the implant site. Wire cutters are used to cut the twisted ends and bury them in adjacent tissue. The graft is trialed into the central gap defect and sutured side to side with N2 FiberWire (Arthrex). The excess Achilles collagen graft can be flipped over itself distally if needed to cover any remaining defects. When there is adequate coverage of the defect, the excess graft can be resected. The medial and lateral retinaculum are closed with N2 Fiberwire. Before complete subcutaneous closure, the knee is flexed under direct visual inspection to assess to what degree the knee can be mobilized before repair, and graft augmentation is brought to tension. The skin is closed in standard fashion.