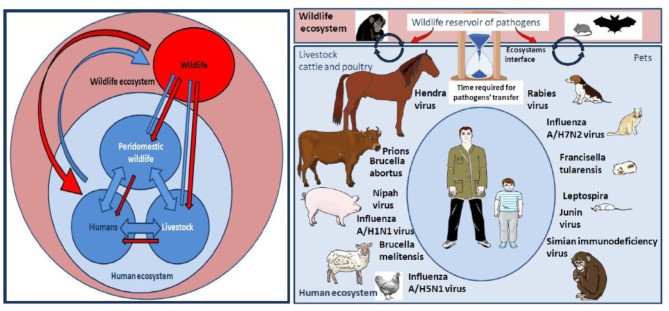
Figure 3.
Left panel: Pathogens flow at the human-livestock-wildlife interface. Many factors associated to this interaction network contribute to a trend toward the globalization of the distribution of pathogens: Ecosystems evolution, extensive agriculture, and water control projects, anarchic urbanization, migration of humans and animals, agroecology and livestock-wildlife interactions, spread of vectors, climate change, human behaviors, development of regional, and international transports. Right panel: NHP can be sometimes wildlife ecosystem actors and sometimes actors of the human ecosystem, especially when they are kept as pets. At the level of wild ecosystems, NHP are not the only source of pathogens, they are important players alongside other actors such as bats, rodents, or birds. When NHP come in close contact with humans as pets they can either directly transmit pathogens to humans or infect actors of the human ecosystem such as farm animals (livestock, cattle, poultry) or pets that can become intermediates in the transmission of pathogen to humans. Of course, most pathogens transmitted to humans by farm animals or pets do not originate from NHP. The figure summarizes examples of pathogens' transmitted from cattle, poultry, or pets to humans. The SARS-like bat CoV was transmitted to humans after evolution in the Himalayan palm-civet. The MERS-like bat CoV, originated in vespertilionid bats and evolved in dromedary prior to its transmission to human. The Hendra virus was passed from the Pteropus bat to horses, followed by transmission from horses to humans. Pteropus bats were also responsible for Nipah virus transmission to pigs which infected humans. In fact, bats are among the major reservoirs of viruses (including lyssavirus, filoviruses, coronaviruses, and paramyxoviruses), and a threat because they are adapted to flight on long distances, thus dispatching pathogens to a larger area. For the same reasons of mobility over long distance, birds are also exquisitely adapted to carry pathogens (such as influenza viruses) to farm animals before being passed on to humans. Pigs play a role in the transmission of influenza A/H1N1 to humans. Transmission of A/H7N2 to humans by cats was reported. Poultry was involved in the transmission of A/H5N1 to humans. Viruses can also be transmitted in unconventional manners such as the West Nile virus, a vector-borne pathogen maintained in a bird-mosquito cycle that infects horses and contaminated a veterinarian during the brain autopsy of a horse, or a pig found carrying a rabies virus. Investigation of wounds of humans bitten by farm animals has often shown the presence of Actinobacillus lignieresii, A. suis, Staphylococcus aureus, Prevotella melaninogenica, Escherichia coli, and Pasteurella multocida among others. In the USA, dogs cause about 1,000,000 bite cases/year (Bic/y) and cats 400,000 Bic/y for 90 million pets. Infection rates was about 15% following dog bites and 40% following cat bites and almost half of the wounds were polymicrobial with aerobic and anaerobic organism. There is a specific concern for rabies transmission. Most deaths from rabies occur in India, Africa, Latin America and Southeast Asia with a hotspot in Thailand were 10% of stray dog in Bangkok, are infected with rabies (compared to 1% in the US). Children have developed tularemia after contact with hamsters carrying Francisella tularensis. Guinea pig and rat pets could possibly spread Junin virus through their urine, feces and saliva. Cases of children bitten by rats infected by Leptospira were reported. The bites of monkeys kept as pet are also a source of concern.