Abstract
Objective:
Although there are currently several efficacious treatments for depressed and suicidal adolescents, less is known about predictors and moderators of adolescents’ treatment response. A growing literature has identified family functioning as a prognostic indicator of adolescents’ likelihood of benefiting from treatment. The current study tested both observational and perceived measures of family functioning as indicators of adolescents’ response to two treatment conditions.
Method:
The sample consisted of one hundred and twenty-nine depressed and suicidal adolescents (Mage = 14.96, 82.9% female, 56% black/African American) who were randomized to Attachment-Based Family Therapy (ABFT) or Family-Enhanced Non-Directive Supportive Therapy (FE-NST; Diamond et al., 2019). Baseline assessments of family functioning included ratings of parent-adolescent communication coded with the Goal-Corrected Partnership in Adolescence Coding System (GPACS; Lyons-Ruth, Hennighausen, & Holmes, 2005) and adolescent and parent reports of family conflict and cohesion from the Self-Report of Family Functioning (SRFF; Bloom, 1985).
Results:
Adolescents who engaged in more uncooperative communication with their parents during a ten-minute conflict discussion showed greater reductions in depressive symptoms in both treatments. Adolescents from traditionally underserved (non-white or lower income) families showed greater reductions in suicidal ideation in both treatments.
Conclusions:
ABFT and FE-NST were most effective for adolescents from traditionally underserved families and adolescents who engaged in less cooperative communication with their caregivers. Observational ratings of parent-adolescent communication were better prognostic indicators of treatment response than were self-reported indicators of global family functioning. Implications for generalizing these results to other treatments for depressed and suicidal adolescents are discussed.
Keywords: adolescence, depression, suicide, family functioning, treatment benefit
Public Health Significance Statement:
Identification of factors that predict treatment response for depressed and suicidal adolescents holds important implications for treatment planning. The current study extends prior literature by testing multiple measures of family functioning as well as demographic factors as predictors and moderators of depressed and suicidal adolescents’ response to Attachment-Based Family Therapy (ABFT) and Family-Enhanced Non-Directive Supportive Therapy (FE-NST). ABFT and FE-NST were particularly effective in reducing depressive symptoms in adolescents who engaged in less cooperative communication with their parent at the start of treatment and in reducing suicidal ideation in non-white adolescents and adolescents from lower income families.
Data Transparency:
The data reported in the current manuscript were collected as part of a randomized controlled trial (RCT). Findings from this RCT have been reported in separate manuscripts. Manuscript 1 (MS1; published) examines treatment differences in primary outcomes of rates of change in depressive and suicidal ideation symptoms. MS2 (published) and MS3 (published) are cross-sectional studies that use pre-treatment variables (coded suicide narratives and adolescent attachment styles in MS2 and indicators of social networks and peer deviance in MS3) to predict baseline suicide ideation intensity. MS4 (published) examines baseline emotion dysregulation and weekly assessments of negative affect, negative interpersonal events, and session insight to test spillover effects of negative events on adolescents’ insight derived from weekly therapy sessions. MS5 (published) identifies three latent classes of treatment response, which are predicted by baseline variables of non-suicidal self-injury, pessimism, Major Depressive Disorder diagnosis, and perceived burdensomeness. Parent-Teen Communication Predicts Treatment Benefit for Depressed and Suicidal Adolescents
The past several decades have witnessed the development of a number of treatments for depressed and suicidal adolescents (for reviews, see Curry, 2014; Glenn, Franklin, & Nock, 2015). Although several treatments have been identified as “probably efficacious,” there is substantial variability in adolescents’ benefit from these interventions. This variability highlights the need to identify baseline variables that help clinicians select personalized treatments for adolescents. The growing emphasis on more personalized approaches to treatment planning has called for identifying both prognostic indicators, which predict variation in treatment response across treatment conditions, and prescriptive factors, which moderate differential response between treatment modalities (Cohen & DeRubeis, 2018; DeRubeis et al., 2014). Family functioning represents one promising domain for testing prognostic and prescriptive indicators of depressed and suicidal adolescents’ response to treatment. The current study tests the impact of family functioning on adolescents’ treatment benefit from a randomized controlled trial (RCT) comparing Attachment-Based Family Therapy (ABFT) to Family-Enhanced Non-Directive Supportive Therapy (FE-NST) for depressed and suicidal adolescents (Diamond et al., 2019). In addition to family functioning, we also explore indicators of underserved status (race and income) as moderators of treatment response in a racially and economically diverse sample.
Assessing Family Functioning in Treatment Studies of Depressed and Suicidal Adolescents
The extant literature on family functioning as an indicator of depressed and suicidal adolescents’ response to treatment has relied primarily on self-report measures. These perceived measures of family conflict and lack of family cohesion predicted poorer treatment response among depressed adolescents receiving cognitive-behavioral therapy (CBT) and/or pharmacological intervention (Asarnow et al., 2009; Feeny et al., 2009; Rengasamy et al., 2013) as well as among depressed adolescents participating in CBT or a life skills control condition (Rohde, Seeley, Kaufman, Clarke, & Stice, 2006). Self-reported family conflict has also accounted for increased risk of suicidal ideation and behaviors in adolescents receiving medication and/or CBT (Brent et al., 2009). Therefore, the majority of these studies suggest that perceptions of negative family functioning reduce the likelihood that adolescents will benefit across CBT, pharmacological, and control interventions (Asarnow et al., 2009; Brent et al., 2009; Rengasamy et al., 2013; Rohde et al., 2006), with more limited evidence suggesting a moderating effect whereby CBT was less effective than medication for adolescents who perceived more negative family environments (Feeny et al., 2009).
A different pattern of results has emerged in studies that have tested self-reported family functioning as an indicator of response to interventions that specifically target adolescents’ relationship functioning. Adolescents who perceived more conflictual relationships with their mothers benefited more from interpersonal psychotherapy-adolescent skills training (IPT-AST) than from school counseling (Young, Gallop, & Mufson, 2009). These adolescents have also been shown to derive greater benefit from interpersonal psychotherapy for depressed adolescents (IPT-A) than from school-based treatment as usual (TAU; Gunlicks-Stoessel, Mufson, Jekal, & Turner, 2010). Similarly, self-harming adolescents reporting more dysfunctional family environments displayed better response to the Self-Harm Intervention: Family Therapy (SHIFT) compared to TAU (Cottrell et al., 2018). These findings suggest that adolescents who perceive more negative family environments may be more likely to benefit from relationship-focused treatments. Together, this literature highlights the importance of considering treatment modality (e.g., a focus on individual skill-building versus a focus on relationship functioning) when examining the impact of family functioning on likelihood of treatment benefit.
Studies of family functioning and adolescents’ treatment benefit have typically been limited to self-reports of either the global family environment or the dyadic parent-adolescent relationship. However, studies utilizing both global and dyadic reports suggest that these two constructs may yield differential indicators of adolescents’ treatment response (Feeny et al., 2009; Gunlicks-Stoessel et al., 2010). Observational assessment of parent-teen interactions offers an alternative measure of dyadic functioning to self-reports. Although observed parent-adolescent communication has been implicated in both externalizing and internalizing problems (Allen & Tan, 2016; Chaplin et al., 2012; Restifo & Bögels, 2009; Sheeber, Davis, Leve, Hops, & Tildesley, 2007), a central challenge is to extend accessible observational paradigms and coding systems to treatment studies of depressed and suicidal adolescents. The Goal-Corrected Partnership in Adolescence Coding System (GPACS; Lyons-Ruth, Hennighausen, & Holmes, 2005) can be coded from ten minutes of parent-adolescent conflict discussion and has been found to distinguish more secure and cooperative parent-teen dyads from more negative patterns of interaction (Obsuth, Hennighausen, Brumariu, & Lyons-Ruth, 2014). Analyses of GPACS scales have associated indicators of cooperative communication with lower levels of internalizing, externalizing, and risky problem behaviors (Kobak, Zajac, Abbott, Zisk, & Bounoua, 2017; Obsuth et al., 2014). This cooperative communication dimension holds particular promise as a prognostic and prescriptive indicator of adolescent treatment response.
Race and Income as Indicators of Treatment Response
In addition to risk associated with family functioning, there are other contextual variables that may influence adolescents’ engagement in and response to treatment. Youth from low-income and racial minority families are typically less likely to access mental health services (Coker et al., 2009) and are more likely to encounter barriers to treatment such as cost, increased distance to service providers, and stigma-related concerns (Alegria, Vallas, & Pumariega, 2010; Young & Rabiner, 2015). These disparities tend to be greater for youth with internalizing problems compared to those with externalizing symptoms (Gudiño, Lau, Yeh, McCabe, & Hough, 2009; Merikangas et al., 2011). Yet results from two of the largest treatment studies for adolescent depression are contradictory regarding the impact of family income and race on treatment benefit (Asarnow et al., 2009; Curry et al., 2006). However, treatment studies are often limited by missing family income data and racially homogenous samples (Asarnow et al., 2009), highlighting the need for studies that examine treatment benefit in more racially and economically diverse samples (Miranda, Nakamura, & Bernal, 2003).
Studies of effects of income and race on adolescents’ treatment benefit also need to examine how these variables interact with treatment condition. Youth from minority families may be especially vulnerable to disruptions in family functioning (e.g., related to weakening of traditional, family-centered values through acculturation processes; Balis & Postolache, 2008; Kuhlberg, Peña, & Zayas, 2010; Silva & Van Orden, 2018). These minority youth may be more likely to benefit from treatments that seek to improve family relationships as opposed to more individually-focused treatments (Kuhlberg et al., 2010). For instance, although both CBT and IPT were found to effectively reduce depressive symptoms in a sample of Puerto Rican adolescents, IPT was particularly efficacious in enhancing adolescents’ self-concept and social adaptation (Rosselló & Bernal, 1999). More research is needed in racially and economically diverse samples that further examines the effects of relationship-focused treatments.
The Current Study
The overall goal of the current study was to examine multiple indicators of adolescents’ family functioning and underserved status as predictors and moderators of adolescents’ response to Attachment-Based Family Therapy (ABFT; Diamond, Diamond, & Levy, 2014) and Family-Enhanced Non-Directive Supportive Therapy (FE-NST; Levy & Diamond, 2010). Both treatments shared a common goal of improving the adolescent’s ability to rely on adult support for managing suicidal and depressive symptoms. ABFT is premised on the notion that ruptures in the parent-adolescent attachment bond precipitate and maintain adolescents’ symptoms. This treatment primarily relies on joint parent-teen sessions that address the rupture and enhance the adolescent’s confidence in a parent’s availability (Diamond, Russon, & Levy, 2016; Kobak, Zajac, Herres, & Ewing, 2015). In FE-NST, the therapist provides a supportive and reflective listener (Brent & Kolko, 1991) who encourages the adolescent to explore and clarify distressing thoughts and feelings. FE-NST is supplemented by five sessions for parents that include joint parent-teen safety planning and parent psychoeducation about their adolescent’s depressive and suicidal symptoms. Analyses of the primary outcomes indicated that adolescents in both conditions showed treatment benefit in terms of significant reductions in their depressed and suicidal symptoms. The analyses revealed no significant effects of treatment condition on adolescents’ treatment benefit (Diamond et al., 2019).
The current study had two aims. First, self-reported and observed indicators of family functioning were tested as predictors and moderators of depressed and suicidal adolescents’ response to ABFT and FE-NST. Based on prior literature, we expected that the focus of enhancing the adolescent’s access to a supportive relationship with a therapist in FE-NST or a parent in ABFT would be particularly effective for adolescents from more dysfunctional families. Further, because ABFT includes multiple sessions that specifically target parent-adolescent interactions, we explored whether adolescents with more communication difficulties with a parent would be particularly likely to benefit from ABFT compared to FE-NST. Second, indicators of adolescents’ underserved status (family income and race) were considered as potential predictors and moderators of treatment benefit.
Method
Participants
Participants were recruited from emergency rooms, inpatient psychiatric hospitals, outpatient facilities, schools, and self-referrals to participate in an RCT comparing ABFT and FE-NST. A total of 253 adolescents were screened for eligibility. Inclusion criteria required severe suicidal ideation (score ≥ 31 on the Suicidal Ideation Questionnaire-Junior; SIQ-JR; Reynolds, 1988) and moderate depression (score ≥ 20 on the Beck Depression Inventory-II; BDI-II; Beck, Steer, & Brown, 1996). Participants were excluded if the adolescent demonstrated imminent risk of harm to self or others, psychotic symptoms, or severe impairment in cognitive functioning; started an anti-depressant medication within three weeks of the initial assessment; did not have a willing adult caregiver to participate; or was non-English speaking. For additional information regarding participant recruitment and screening, see Diamond et al. (2019).
One hundred and twenty-nine adolescents between the ages of 12 and 18 (M = 14.96, SD = 1.66) were enrolled, with females representing 82.9% of the sample. More than half of the adolescents identified as black/African American (56%), followed by 31% white/Caucasian, and 13% another race (American Indian or Alaskan Native, Asian, Native Hawaiian or Other Pacific Islander, or “other”). Sixteen percent of the adolescents reported Hispanic/Latino ethnicity. At enrollment, 27.1% of adolescents were taking medication to treat depressive symptoms, and 31% of families reported living below the poverty line, as indicated by an income-to-needs ratio equal to or less than 1.0. Most (79.8%) of the adolescents were accompanied to the baseline assessment by their mother, while 11.6% were accompanied by their father and 8.5% by a primary caregiver other than their mother or father (e.g., aunt, grandmother, stepmother, older sibling). We use the term “parent” to refer to the caregiver who participated in treatment with the adolescent.
Procedure
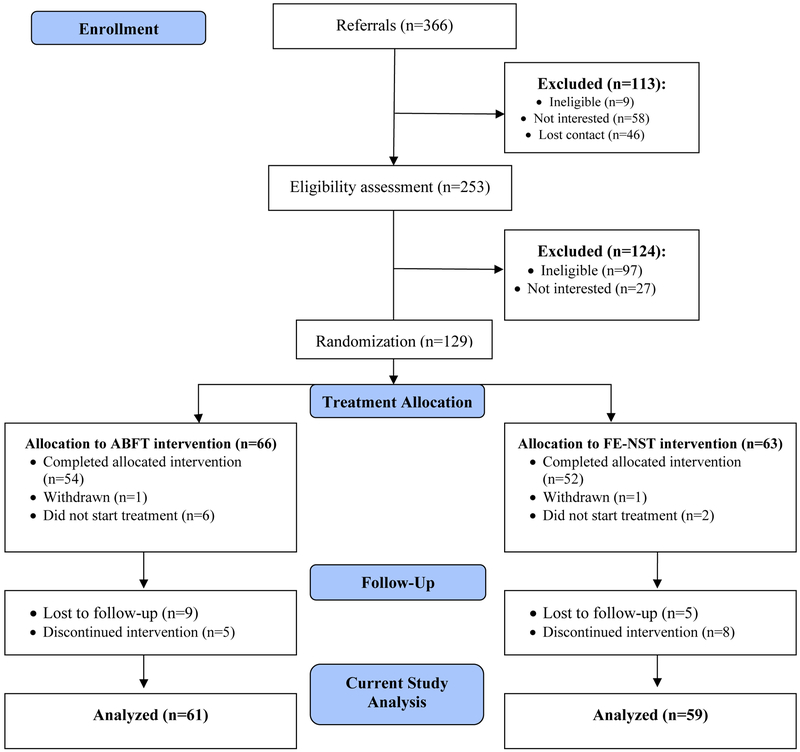
The study was approved by the Institutional Review Boards of both institutions involved in the study. Adolescents provided consent or assent, and an adult caregiver provided consent. Prior to treatment, adolescents and their parents completed a battery of interviews and self-report measures, and parent-adolescent dyads were video-recorded during a 10-minute conflict discussion. Parent and adolescents’ ratings of their areas of disagreement established the topic for the conflict discussions. Following the baseline assessment, families were randomly assigned to 16 weeks of ABFT or FE-NST. Participants were stratified based on variables including gender, history of past suicide attempts, and endorsement of family conflict (score > 13 on the Self-Report of Family Functioning [SRFF; Bloom, 1985] conflict scale). Primary outcome measures of suicidal and depressive symptoms were collected monthly through Week 16 (post-treatment) by staff blind to treatment condition. For a consort diagram of participant flow, see Figure 1.
Figure 1.
Consort diagram. Note: Version of this consort diagram for primary outcome analyses previously published in Diamond et al. (2019).
Treatments
Attachment-Based Family Therapy (ABFT).
ABFT (Diamond et al., 2014) is a 16-week manualized treatment that has demonstrated efficacy in treating suicidal and depressed adolescents (Glenn et al., 2015). ABFT purports that ruptures in the parent-adolescent relationship, such as conflict, parental abdication or abandonment, neglect, or abuse, can reduce the adolescent’s confidence in the parent’s availability. ABFT reframes the adolescent’s suicidality by linking the adolescent’s difficulty in turning to parents for help to their suicidal thoughts and feelings. The ABFT protocol consists of five tasks, which begin with a conjoint parent-adolescent reframe session, followed by individual sessions with the adolescent then parent alone, followed by a conjoint reparative task in which the therapist coaches the parent and teen through conversations about perceived attachment ruptures, and, finally, followed by conjoint sessions to consolidate improvement in the parent-adolescent relationship.
Family-Enhanced Non-Directive Supportive Therapy (FE-NST).
FE-NST (Levy & Diamond, 2010) is a 16-week manualized treatment adapted from the Supportive Relationship Treatment Manual (Brent & Kolko, 1991). This individual, supportive treatment focuses on the therapist reflectively listening, empathizing, and offering summarizing statements that may organize or bring new understandings of the adolescent’s experiences. In the current study, individual sessions were supplemented with one conjoint parent-adolescent session for safety planning and four parent-only education sessions on understanding adolescent depression, assessing suicide risk, enhancing advocacy and resource development, and increasing problem-solving.
Baseline Assessments of Family Functioning
Cooperative communication.
Raters, trained by a GPACS developer, rated the parent-adolescent conflict discussions with four 5-point scales from the GPACS coding system that indicated the overall level of cooperative communication during the discussion (Obsuth et al., 2014). Scale reliabilities presented here are based on 18.3% of the videos, which were double-coded by a study rater and a GPACS developer. All coders were blind to treatment condition and all other study measures. The first scale, collaborative communication, assesses the extent to which parents and adolescents engage in balanced and reciprocal conversation (1: one individual dominates the discussion, 5: both voice their opinions comfortably and constructively; M(SD) = 2.36(0.94), intraclass correlation (ICC) = 0.83). The warmth/valuing scale rates the extent to which parents and adolescents share positive regard and voice statements of warmth, valuing, and care (1: absence of warmth or valuing, 5: high positive regard, warmth, and valuing in the interaction; M(SD) = 2.68(0.98), ICC = 0.88). The parent validation of the adolescent scale rates the degree to which the parent is open and responsive to the adolescent’s opinions, ideas, and assertions (1: parental invalidation, 5: parent engages and appropriately seeks the adolescent’s thoughts and feelings; M(SD) = 2.50(0.94), ICC = 0.86). Finally, the adolescent respectful spontaneity scale measures the adolescent’s ability to clearly and respectfully state and support his or her opinions and attitudes during the conversation (1: adolescent is unable to provide or support a viewpoint, 5: adolescent advances an opinion in a consistent, comfortable, and natural manner; M(SD) = 2.48(1.00), ICC = 0.89). Ratings of the four scales demonstrated good internal consistency (Cronbach’s α = 0.89) and were averaged to form a dimension indexing cooperative communication (Kobak et al., 2017), with higher scores indicating more cooperative and validating interactions.
Self-reported family conflict and cohesion.
Parents and adolescents completed the SRFF, which yields two subscales. Five items assess family cohesion (e.g., “family members really help and support one another”), and five items assess family conflict (e.g., “we fight a lot in our family”). Each item is assessed on a 4-point scale (1: “never true for my family,” 4: “very true for my family”). The SRFF has demonstrated adequate validity (Bloom, 1985) and reliability (Stark, Humphrey, Crook, & Lewis, 1990), with previous studies demonstrating Cronbach’s alphas between 0.63 and 0.91. In the current study, family cohesion demonstrated adequate internal consistency for both parent (Cronbach’s α = 0.78) and adolescent (Cronbach’s α = 0.79) reports. In the current sample, parent-rated family conflict yielded a Cronbach’s alpha of 0.57. The adolescent-rated family conflict item “family members rarely criticize each other,” reverse coded, was removed to improve internal consistency. The remaining four conflict items demonstrated a Cronbach’s alpha of 0.66. To improve internal consistency, the conflict and cohesion scales were aggregated for parents and for adolescents. The parent- and adolescent-rated family functioning scales demonstrated adequate internal consistency (Cronbach’s α = 0.82 for adolescent report, Cronbach’s α = 0.76 for parent report).
Demographic Variables
Parents provided household income and size. Income-to-needs ratios were calculated by dividing family income by the poverty threshold corresponding to household size. Adolescents reported their race, which was coded 1 = white, 0 = non-white. Adolescents’ medication status (whether or not the adolescent was taking medication for depression at the start of treatment), age, and gender were included to control for possible effects on baseline symptom severity and treatment response.
Monthly Symptom Assessments
Depressive symptoms.
Depressive symptoms were assessed using the BDI-II, a 21-item self-report measure. Items are rated on a 4-point scale (0: absence of symptom, 3: most severe symptom) and inquire about a range of depressive symptoms, including sadness, irritability, loss of interest, and worthlessness. In the current sample, the BDI-II demonstrated good internal consistency (Cronbach’s α = 0.85).
Suicidal ideation.
Adolescents’ suicidal ideation was measured using the SIQ-JR, a 15-item self-report measure. Items include statements such as “I thought about killing myself” and “I thought about how I would kill myself.” Each item is rated on a 7-point scale that assesses the frequency of these suicidal thoughts (1: absence of the thought, 7: the thought has occurred almost every day for the past month). In the current sample, the SIQ-JR demonstrated good internal consistency (Cronbach’s α = 0.84).
Data Analytic Plan
An initial principal component analysis (PCA) examined the latent structure of self-reported and observed indicators of family functioning. Hierarchical linear modeling (HLM; Raudenbush & Bryk, 2002) tested the prognostic and prescriptive effects of cooperative communication, parent and adolescents’ reports of global family functioning, and indicators of underserved status on adolescents’ treatment response. Initial examination of the rates of change in SIQ-JR and BDI-II separately revealed non-linear trends in both outcomes over time. To account for this non-linearity, a log-10 transformation of the time variable was used in each model, which allowed for an accommodation of faster rates of change early in treatment (Young et al., 2016). Slopes in each model therefore represent symptom change across log-10 transformed 4-week intervals over the course of 16 weeks. To enhance interpretation, total symptom change from baseline to Week 16 will also be used as an indicator of treatment benefit. To fit the hierarchical linear models, time was analyzed as a within-subjects (Level-1) predictor of depressive and suicidal symptoms over the course of treatment, with Week 0 (baseline) coded as 0. Grand-mean centered baseline variables were then analyzed as between-subjects (Level-2) moderators of within-subject trajectories of symptom change across the 4 months of treatment. Random intercepts and random slopes were estimated. All error terms were allowed to vary, and robust standard errors were analyzed to account for non-normality and outliers in the data (Raudenbush & Bryk, 2002). Final estimation of fixed effects was estimated using robust standard errors.
Missing Data
Most (69.8%) adolescents completed all five of the baseline, 4, 8, 12, and 16 week assessments of depressive and suicidal symptoms, while 13.2% completed four of the five assessments, 7% completed two or three, and 10% completed one. The number of repeated measures completed was not significantly related to study variables. Nine adolescents did not complete the baseline conflict discussion. Therefore, the fixed effects and variance components are based on the 120 adolescents with complete Level-2 data. However, there were no significant differences on any study variables based on completion of the baseline conflict discussion. Therefore, missing data was assumed to be missing at random, and estimates were calculated in HLM based on restricted maximum likelihood estimation.
Results
PCA of Baseline Family Functioning
A PCA of the multiple indicators of family functioning used the four observed communication scales, adolescent-rated family conflict and cohesion, and parent-rated family conflict and cohesion. The GPACS scales were included to replicate the dimension of cooperative communication reported in previous studies (Kobak et al., 2017; Obsuth et al., 2014) and to evaluate potential cross-loadings with self-report measures of family functioning. The PCA, with a promax rotation, yielded two factors with eigenvalues greater than 1, which accounted for 66.9% of the variance in the eight scales. The four GPACS scales loaded on the first factor, while adolescent and parent reports of conflict and cohesion loaded on the second factor. However, previous research has typically examined parent and adolescent reports as separate variables. Therefore, a second PCA was conducted with a promax rotation that fixed the number of factors to three. This model accounted for 76.6% of the variance in the eight scales. The four GPACS scales loaded on the first factor, adolescent-rated conflict and cohesion loaded on the second factor, and parent-rated conflict and cohesion loaded on the third factor. Factor loadings are presented in Table 1. None of the scales cross-loaded on the other factors. The three-factor model of family functioning (observed cooperative communication [mean of the four GPACS codes], adolescent-rated family functioning [mean of adolescent-rated conflict and cohesion, with the conflict scale reverse coded to provide an overall indicator of positive family functioning], and parent-rated family functioning [mean of parent-rated conflict, reverse coded, and cohesion]) was used in subsequent analyses.
Table 1.
Factor loadings for indicators of family functioning
| Cooperative communication | Adolescent-rated family functioning | Parent-rated family functioning | |
|---|---|---|---|
| GPACS collaborative communication | .95 | .03 | −.08 |
| GPACS parent validation of the adolescent | .90 | −.12 | .08 |
| GPACS adolescent respectful spontaneity | .82 | .12 | −.10 |
| GPACS warmth/valuing | .81 | −.003 | .12 |
| Adolescent-rated family cohesion | .05 | .92 | −.06 |
| Adolescent-rated family conflict | .03 | −.81 | −.09 |
| Parent-rated family conflict | −.04 | .10 | −.95 |
| Parent-rated family cohesion | −.05 | .24 | .68 |
Note: Factor loadings greater than .40 are bolded.
Descriptive Analyses
Descriptive statistics and zero-order correlations are presented in Table 2. At pre-treatment, the three indicators of family functioning (cooperative communication and adolescent and parent perceptions of the family environment) were positively correlated. Higher ratings of cooperative communication were more evident among white families, higher income families, and adolescents who were receiving anti-depressant medication. Adolescents receiving anti-depressant medication at the start of treatment also reported more severe depressive and suicidal symptoms at baseline. There were several correlations between pre-treatment and post-treatment variables. Adolescents with more pre-treatment cooperative communication and adolescents who entered treatment on anti-depressant medication reported more post-treatment depressive and suicidal ideation symptoms. White adolescents and adolescents from higher income families had higher levels of post-treatment suicidal ideation. Treatment condition was not associated with any of the study variables. There were no associations between study variables and the adolescent’s relationship with the participating caregiver (e.g., mother, father, other caregiver).
Table 2.
Means, standard deviations, and zero-order correlations of study variables
| Mean | SD | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Cooperative Communication | 2.50 | 0.84 | ---- | .29** | 27** | 24** | .22* | −.05 | −.03 | .30** | −.02 | −.11 | −.01 | .26** | .20* |
| 2. Adolescent-rated family functioninga | 2.53 | 0.31 | ---- | .49*** | .26** | .03 | −.12 | .06 | .07 | −.01 | −.16+ | .03 | .01 | −.07 | |
| 3. Parent-rated family functioningb | 2.61 | 0.29 | ---- | .30** | −.06 | −.09 | .06 | .09 | −.05 | −.13 | .02 | −.01 | −.03 | ||
| 4. Income-to-needs ratio | 2.07 | 1.45 | ---- | .44*** | −.004 | −.007 | .35*** | .07 | −.10 | −.10 | .08 | .25** | |||
| 5. Racec | 0.31 | 0.46 | ---- | .13 | −.08 | .46*** | .05 | .09 | −.10 | .15 | .36*** | ||||
| 6. Age | 14.96 | 1.66 | ---- | −.04 | .10 | −.05 | .18* | .04 | .15 | .18+ | |||||
| 7. Genderd | 0.17 | 0.38 | ---- | −.09 | −.01 | −.18* | .002 | −.12 | −.003 | ||||||
| 8. Medicatione | 0.27 | 0.45 | ---- | .04 | .26** | .30** | .38*** | .37*** | |||||||
| 9. Treatment conditionf | 0.52 | 0.50 | ---- | .07 | .03 | −.01 | −.09 | ||||||||
| 10. Baseline BDI | 35.62 | 9.30 | ---- | .41*** | .46*** | .33*** | |||||||||
| 11. Baseline SIQ | 49.89 | 15.16 | ---- | .22* | .28** | ||||||||||
| 12. Week 16 BDI | 18.13 | 14.08 | ---- | .70*** | |||||||||||
| 13. Week 16 SIQ | 20.89 | 16.80 | ---- |
Note:
aggregated adolescent-rated family conflict (M = 2.18, SD = 0.67), reverse coded, and cohesion (M = 2.87, SD = 0.67);
aggregated parent-rated family conflict (M = 2.16, SD = 0.47), reverse coded, and cohesion (M = 3.06 SD = 0.61);
1 = white, 0 = non-white;
1 = male, 0 = female;
1 = currently on anti-depressant medication, 0 = not currently on anti-depressant medication;
1 = ABFT, 0 = FE-NST;
p < .10;
p < .05;
p < .01;
p < .001
Hierarchical Linear Models
Depressive symptoms.
An unconditional model examined the within-subjects and between-subjects variability in depressive symptoms over the sixteen weeks of treatment. The intraclass correlation coefficient (ICC) indicated that 47.8% of the variance in depressive symptoms was accounted for by between-subject variability, leaving 52.2% that was due to within-subject fluctuations. A within-subjects (Level-1) model estimated a fixed intercept of 35.16 (t(119) = 38.37, p < 0.001) as the average starting level of adolescent depressive symptoms. A fixed slope of −24.31 (t(119) = −13.39, p < 0.001) indicated that, on average, adolescents reported a significant decrease in depressive symptoms from the beginning to end of treatment. On average, this rate of change corresponded to a decline of 17.02 points on the BDIII between baseline and post-treatment. The random effects in both the intercept (SD = 7.81, χ2 (107) = 276.25, p < 0.001) and slope (SD = 13.51, χ2 (107) = 221.92, p < 0.001) indicated significant between-subject variability in both starting levels and rates of change in depressive symptoms.
The family functioning, demographic, and medication variables as well as treatment condition were entered as Level-2 predictors of adolescents’ trajectories of depressive symptoms during treatment. Results, presented in Table 3, indicated that cooperative communication predicted slower rates of decline in depressive symptoms (B = 5.43, t(110) = 2.49, p = 0.01). However, neither self-reported family functioning nor adolescents’ medication status was a significant predictor of reductions in depressive symptoms. As previously reported, there were no effects of treatment condition on rates of change in depression. None of the interactions between treatment condition and the indicators of family functioning or underserved status were significant.
Table 3.
Final estimation of fixed effects (with robust standard errors) for BDI-II
| Full Model | Reduced Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Fixed Effects | Coefficient | S.E. | t-ratio | p-value | Coefficient | S.E. | t-ratio | p-value |
| Intercept | ||||||||
| Intercept | 35.16*** | 0.83 | 42.53 | <0.001 | 35.16*** | 0.88 | 40.03 | <0.001 |
| Cooperative communication | −0.74 | 1.26 | −0.59 | 0.56 | −1.88 | 1.29 | −1.46 | 0.15 |
| Adolescent-rated family functioning | −2.24 | 1.83 | −1.22 | 0.22 | ||||
| Parent-rated family functioning | −0.15 | 2.03 | −0.07 | 0.94 | ||||
| Treatment conditiona | 1.85 | 1.70 | 1.08 | 0.28 | ||||
| Income-to-needs ratio | −0.79 | 0.69 | −1.14 | 0.26 | ||||
| Age | 1.15+ | 0.59 | 1.95 | 0.05 | ||||
| Genderb | −2.26 | 1.99 | −1.13 | 0.26 | ||||
| Racec | −2.08 | 1.89 | −1.10 | 0.27 | ||||
| Medicationd | 7.78*** | 2.23 | 3.49 | <0.001 | 7.64** | 1.97 | 3.87 | <0.001 |
| Slope | ||||||||
| Intercept | −24 48*** | 1.71 | −14.29 | <0.001 | −24 27*** | 1.73 | −14.02 | <0.001 |
| Cooperative communication | 5.43* | 2.18 | 2.49 | 0.01 | 6.55** | 1.98 | 3.31 | 0.001 |
| Adolescent-rated family functioning | −1.75 | 2.89 | −0.61 | 0.55 | ||||
| Parent-rated family functioning | 0.48 | 4.54 | 0.11 | 0.92 | ||||
| Treatment condition | −2.86 | 3.51 | −0.82 | 0.42 | ||||
| Income-to-needs ratio | 1.92 | 1.45 | 1.33 | 0.19 | ||||
| Age | −0.07 | 0.94 | −0.07 | 0.94 | ||||
| Gender | −2.56 | 4.12 | −0.62 | 0.54 | ||||
| Race | −1.64 | 4.23 | −0.39 | 0.70 | ||||
| Medication | 4.88 | 4.09 | 1.19 | 0.24 | ||||
Note: N = 120, df = 110 for full model, df = 117 (intercept), 118 (slope) for reduced model;
1 = ABFT, 0 = FE-NST;
1 = male, 0 = female;
1 = white, 0 = non-white;
1 = currently on anti-depressant medication, 0 = not currently on anti-depressant medication;
p < .10;
p < .05;
p < .01;
p < .001.
Unstandardized coefficients are reported. Tests of interactions between treatment condition and indicators of family functioning, adolescent race, and family income yielded non-significant results and are therefore not included in this table.
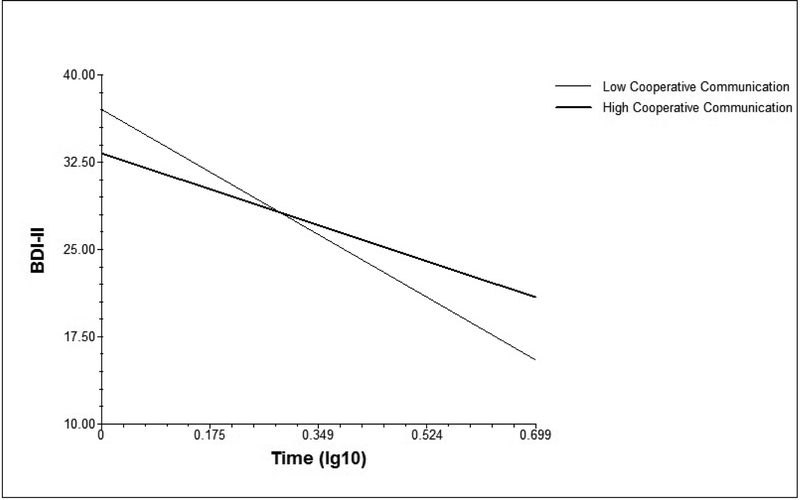
A reduced model tested cooperative communication and medication status as the only Level-2 predictors (see Table 3). Medication status continued to be associated with starting levels of depression (B = 7.64, t(117) = 3.87, p = <0.001), and cooperative communication remained a significant predictor of slower rates of decline in depressive symptoms (B = 6.55, t(118) = 3.31, p = 0.001). Two models were then estimated, one with cooperative communication zero-centered one standard deviation above the mean and another with cooperative communication zero-centered one standard deviation below the mean. The rates of change in depressive symptoms in these two models are presented in Figure 2. On average, adolescents in high cooperative dyads had slower rates of decline in depressive symptoms (B = −18.75, t(118) = −7.63, p < 0.001), with a total decline of 13.13 points on the BDI-II from baseline to post-treatment. In contrast, adolescents in low cooperative dyads had a faster rate of decline in depressive symptoms (B = −29.79, t(118) = −12.66, p < 0.001), with an estimated total decline of 20.85 points on the BDI-II.
Figure 2.
Rates of change in depressive symptoms over the course of treatment at high and low cooperative communication
Suicidal ideation.
The ICC of an unconditional model of adolescents’ suicidal symptoms over the course of treatment indicated that 35.6% of the variance in suicidal ideation was accounted for by between-subject variability, leaving 64.4% that was due to within-subject fluctuations. A within-subjects (Level-1) model estimated a fixed intercept of 48.66 (t(119) = 34.17, p < 0.001) as the average starting level of suicidal ideation symptoms. A fixed slope of - 41.80 (t(119) = −14.95, p < 0.001) indicated that, on average, adolescents reported a significant decrease in suicidal ideation from the beginning to end of treatment. On average, this rate of change corresponded to a total decline of 29.26 points on the SIQ-JR between baseline and post-treatment. Random effects in the intercept (SD = 12.23, χ2 (107) = 288.56, p < 0.001) and slope (SD = 21.24, χ2 (107) = 225.92, p < 0.001) indicated significant between-subject variability in both starting levels and rates of change in suicidal ideation.
The family functioning, demographic, and medication variables as well as treatment condition were entered as Level-2 predictors of adolescents’ trajectories of suicidal ideation during treatment. Results, presented in Table 4, indicated that adolescents’ pre-treatment reports of positive family functioning predicted faster rates of decline in suicidal ideation (B = −10.87, t(111) = −2.02, p = 0.046). White adolescents and adolescents from higher income households reported slower rates of decline in suicidal symptoms (B = 17.10, t(111) = 2.72, p = 0.008; B = 5.99, t(111) = 2.64, p = 0.01, respectively). Cooperative communication, parent-reported family functioning, and medication status were not significant predictors of reductions in suicidal ideation. As previously reported, there were no effects of treatment condition on rates of change in suicidal ideation. None of the interactions between treatment condition and the indicators of family functioning or underserved status were significant.
Table 4.
Final estimation of fixed effects (with robust standard errors) for SIQ-JR
| Full Model | Reduced Model | |||||||
|---|---|---|---|---|---|---|---|---|
| Fixed Effects | Coefficient | S.E. | t-ratio | p-value | Coefficient | S.E. | t-ratio | p-value |
| Intercept | ||||||||
| Intercept | 48.66*** | 1.28 | 37.88 | 0.001 | 48.67*** | 1.30 | 37.53 | <0.001 |
| Cooperative communication | 0.30 | 1.86 | 0.16 | 0.87 | ||||
| Adolescent-rated family functioning | 1.13 | 2.50 | 0.45 | 0.65 | 0.69 | 2.19 | 0.32 | 0.75 |
| Parent-rated family functioning | −0.94 | 3.23 | −0.29 | 0.77 | ||||
| Treatment conditiona | 2.02 | 2.55 | 0.79 | 0.43 | ||||
| Income-to-needs ratio | −0.93 | 0.99 | −0.94 | 0.35 | −0.94 | 0.96 | −0.98 | 0.33 |
| Age | 0.91 | 0.80 | 1.14 | 0.26 | ||||
| Raceb | −9.35** | 3.24 | −2.89 | 0.005 | −8.18* | 3.32 | −2.46 | 0.02 |
| Medicationc | 15.87*** | 3.62 | 4.39 | 0.001 | 14.77*** | 3.38 | 4.37 | 0.001 |
| Slope | ||||||||
| Intercept | −42 15*** | 2.51 | −16.77 | 0.001 | −42.11*** | 2.53 | −16.66 | <0.001 |
| Cooperative communication | 4.18 | 3.35 | 1.25 | 0.21 | ||||
| Adolescent-rated family functioning | −10.87* | 5.38 | −2.02 | 0.046 | −8.43+ | 4.55 | −1.85 | 0.07 |
| Parent-rated family functioning | 1.53 | 7.03 | 0.22 | 0.83 | ||||
| Treatment condition | −5.58 | 5.10 | −1.09 | 0.28 | ||||
| Income-to-needs ratio | 5.99* | 2.27 | 2.64 | 0.01 | 5.51* | 2.18 | 2.52 | 0.01 |
| Age | 0.71 | 1.32 | 0.54 | 0.59 | ||||
| Race | 17.10** | 6.28 | 2.72 | 0.008 | 16.07* | 6.10 | 2.64 | 0.01 |
| Medication | −7.87 | 5.85 | −1.35 | 0.18 | ||||
Note: N = 120, df = 111 for full model, df = 115 (intercept), 116 (slope) for reduced model;
1 = ABFT, 0 = FE-NST;
1 = white, 0 = non-white;
1 = currently on anti-depressant medication, 0 = not currently on anti-depressant medication;
p < .10;
p < .05;
p < .01;
p < .001.
Unstandardized coefficients are reported. Tests of interactions between treatment condition and indicators of family functioning, adolescent race, and family income yielded non-significant results and are therefore not included in this table.
A reduced model tested adolescent-rated family functioning, race, medication status, and the family income-to-needs ratio as the only Level-2 predictors (see Table 4). Adolescent race and medication status continued to be associated with starting levels of suicidal ideation (B = - 8.18, t(115) = −2.46, p = 0.02; B = 14.77, t(115) = 4.37, p = <0.001, respectively). White racial status and higher income-to-needs ratios remained significant predictors of slower rates of change in suicidal ideation during treatment (B = 16.07, t(116) = 2.64, p = 0.01; B = 5.51, t(116) = 2.52, p = 0.01, respectively). Adolescent-rated family functioning did not significantly predict reductions in suicidal ideation in this model.
Discussion
Observations of parent-adolescent communication as well as indicators of adolescents’ underserved status (race and household income) proved useful as prognostic predictors of adolescents’ treatment benefit in ABFT and FE-NST. The findings indicate that adolescents with more difficulties maintaining cooperative communication with their parents and adolescents who are traditionally underserved in terms of non-white or low-income status are more likely to benefit from both treatments. Adolescents with less cooperative communication showed greater reductions in depressive symptoms compared to those with better communication. Non-white adolescents and adolescents from lower income families showed greater reductions in suicidal ideation compared with white adolescents and those from higher income households. These prognostic indicators of treatment response were independent of treatment condition and were not useful in differentiating between adolescents’ response to ABFT compared with FE-NST.
Although both interventions produced significant treatment gains, different treatment elements may have been responsible for reductions in suicidal and depressive symptoms. Previous studies have often implicated lack of supportive adult relationships in risk for adolescents’ depressive symptoms (Newman, Newman, Griffen, O’Connor, & Spas, 2007; Rueger, Malecki, & Demaray, 2010). As a result, relational treatments such as ABFT and FE-NST, which aim to enhance the adolescent’s access to a supportive adult relationship, may be particularly beneficial for depressed adolescents who lack this support. The observed quality of parent-adolescent communication may be particularly useful in identifying adolescents for whom depressive symptoms are maintained by the relative absence of cooperative and validating interactions with a supportive adult. These adolescents may then experience the greatest declines in depressive symptoms while engaging in these relationship-focused treatments. Overall, these findings fit with results examining adolescents’ response to IPT-A, where improvement in family interpersonal functioning was implicated in reductions in depressive symptoms (Reyes-Portillo, McGlinchey, Yanes-Lukin, Turner, & Mufson, 2017). In contrast, reductions in adolescents’ suicidal ideation may have been accounted for by other elements of the current RCT’s protocols. Management of suicidal symptoms was an active component in both treatments, with weekly monitoring of suicidality, access to 24/7 crisis hotlines, and safety planning (Stanley & Brown, 2012). This high level of monitoring and managing suicidal symptoms may have been particularly beneficial for traditionally underserved adolescents who typically lack access to a standardized, sixteen-week treatment protocol and extensive therapist engagement to ensure participant retention, which were components prioritized in this RCT.
Indicators of communication and underserved status as predictors of treatment benefit showed different associations with depressive and suicidal symptoms. Whereas communication predicted trajectories of depressive symptoms, underserved status predicted trajectories of suicidal symptoms. This effect of parent-adolescent communication on reductions in depressive but not suicidal symptoms is consistent with prior studies indicating that difficulties in interpersonal functioning are implicated in treatment of adolescent depression, but not necessarily suicidal symptoms (Reyes-Portillo et al., 2017; Shpigel, Diamond, & Diamond, 2012). Overall, this research suggests that adolescent depressive symptoms may be particularly sensitive to treatments that are designed to enhance relational support. To the extent that our indicators of underserved status are linked to less access to prior services, treatment benefit for these adolescents should be evident in reductions of both suicidal and depressive symptoms. However, the extant literature is largely inconclusive regarding the effects of race and income on depressed adolescents’ treatment response (Asarnow et al., 2009; Curry et al., 2006). Additional research that examines income and race as predictors of reductions in both depressive and suicidal symptoms in economically and racially diverse samples is needed to further disentangle these effects.
Neither family functioning nor underserved status differentiated between adolescents’ response to the two treatment conditions. The lack of prescriptive effects occurred despite coding that indicated good adherence to the ABFT and FE-NST protocols (Diamond et al., 2019). Although some non-specific treatment elements from FE-NST were present in ABFT, there were virtually no ABFT strategies in the FE-NST condition. Common treatment elements may therefore have accounted for the present findings. Specifically, the supportive relationship provided by the therapist in FE-NST may have compensated for gains in parental support in ABFT. Other common elements such as safety planning and parent involvement may have also reduced the likelihood of finding prescriptive effects.
Parent and adolescent reports of the family environment produced relatively few and less robust predictions of adolescents’ treatment benefit. Only adolescents’ reports of a more cohesive family environment predicted greater reductions in suicidal ideation, but this effect was no longer significant in the reduced model. Our PCA indicated that parent and adolescent perceptions of the family environment and observer ratings of parent-adolescent communication yielded distinct and only modestly correlated indicators of overall family functioning. Importantly, associations between adolescent reports of the family environment and their depressive and suicidal symptoms share common method variance and are more vulnerable to individual attitudes and biases. It may be that adolescents’ reports of a more cohesive family environment reflect general positive expectancies and attitudes that contribute to better treatment engagement (Constantino & Westra, 2012).
Strengths and Limitations
The current study has several strengths. First, few papers have rigorously tested multiple measures of family functioning and contextual indicators of underserved status as predictors and moderators of depressed and suicidal adolescents’ treatment response. The current findings suggest that family functioning is an inclusive term that needs to be differentiated into multiple constructs so that the prognostic and prescriptive utility of these constructs can be evaluated. This study provides support for the utility of an observational assessment of parent-adolescent communication as a predictor of treatment response. The findings also highlight the importance of recruiting racially and economically diverse samples when examining underserved status as prognostic and prescriptive indicators of treatment response. Unfortunately, low-income and non-white families are typically underrepresented in large clinical trials and are more likely to drop out of treatment early when they are included (Nock & Ferriter, 2005).
The study has several notable limitations. First, the value of the GPACS assessment as a prognostic indicator for treatment response needs further testing and replication in other less relationally focused treatments that have been shown to be probably efficacious for depressed and suicidal adolescents. Given that inclusion criteria for this study required at least moderate depressive symptoms and severe suicidal ideation, effects may not generalize to less depressed or suicidal samples. Additionally, the study is limited by the fact that 30.2% of adolescents were missing at least one of the five monthly symptom assessments. Finally, the current sample was predominantly female. Although not unusual for depressed adolescent samples, it does limit our ability to detect gender differences.
Conclusion and Future Directions
The current findings identified prognostic predictors of adolescents’ treatment benefit in two relational treatments. Future research should replicate and extend these findings. Improved family relationships have been identified as mediators of the effect of IPT-A on depressed adolescents’ symptoms (Reyes-Portillo et al., 2017). Changes in observed parent-adolescent communication should similarly be tested as a potential mechanism for reducing suicidal and depressive symptoms. Additionally, future RCTs should directly compare relational treatments with alternative modalities (e.g., ABFT vs. CBT). Although the results indicate that depressed and suicidal adolescents from more dysfunctional or underserved families may be particularly likely to benefit from relationship-focused treatments, additional studies that allow for direct comparisons with alternative or more skills-based treatment modalities are essential. Ultimately, this work can inform more personalized decisions for treating adolescents with depressive and suicidal symptoms. Continued development of prognostic and prescriptive assessment tools may significantly assist in this endeavor.
Acknowledgments:
This work was supported by funding from the National Institute of Mental Health (NIMH) under Grant R01MH091059. The clinical trial, Attachment Based Family Therapy for Suicidal Adolescents, is registered at http://clinicaltrials.gov ().
References
- Alegria M, Vallas M, & Pumariega A (2010). Racial and ethnic disparities in pediatric mental health. Child and Adolescent Psychiatric Clinics of North America, 19(4), 759–774. doi: 10.1016/j.chc.2010.07.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen JP, & Tan JS (2016). The multiple facets of attachment in adolescence In Cassidy J & Shaver PR (Eds.), Handbook of attachment: Theory, research, and clinical applications (3rd ed., pp. 399–415). New York, NY: Guilford Press. [Google Scholar]
- Asarnow JR, Emslie G, Clarke G, Wagner KD, Spirito A, Vitiello B, … Brent D (2009). Treatment of selective serotonin reuptake inhibitor-resistant depression in adolescents: Predictors and moderators of treatment response. Journal of the American Academy of Child & Adolescent Psychiatry, 48(3), 330–339. doi: 10.1097/CHI.Ob013e3181977476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balis T, & Postolache TT (2008). Ethnic differences in adolescent suicide in the United States. International Journal of Child Health and Human Development, 1(3), 281–296. [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Beck Depression Inventory manual (2nd ed). San Antonio, TX: Psychological Corporation. [Google Scholar]
- Bloom BL (1985). A factor analysis of self-report measures of family functioning. Family Process, 24(2), 225–239. doi: 10.1111/j.1545-5300.1985.00225.x [DOI] [PubMed] [Google Scholar]
- Brent DA, Emslie GJ, Clarke GN, Asarnow J, Spirito A, Ritz L, … Keller MB (2009). Predictors of spontaneous and systematically assessed suicidal adverse events in the Treatment of SSRI-Resistant Depression in Adolescents (TORDIA) study. The American Journal of Psychiatry, 166(4), 418–426. doi: 10.1176/appi.ajp.2008.08070976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brent DA, & Kolko DJ (1991). Supportive relationship treatment manual Pittsburgh, PA: University of Pittsburgh. Unpublished manuscript. [Google Scholar]
- Chaplin TM, Sinha R, Simmons JA, Healy SM, Mayes LC, Hommer RE, & Crowley MJ (2012). Parent-adolescent conflict interactions and adolescent alcohol use. Addictive Behaviors, 37, 605–612. doi: 10.1016/j.addbeh.2012.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen ZD, & DeRubeis RJ (2018). Treatment selection in depression. Annual Review of Clinical Psychology, 14, 209–236. doi: 10.1146/annurev-clinpsy-050817-084746 [DOI] [PubMed] [Google Scholar]
- Coker TR, Elliott MN, Kataoka S, Schwebel DC, Mrug S, Grunbaum JA, … Schuster MA (2009). Racial/ethnic disparities in the mental health care utilization of fifth grade children. Academic Pediatrics, 9(2), 89–96. doi: 10.1016/j.acap.2008.11.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Constantino MJ, & Westra HA (2012). An expectancy-based approach to facilitating corrective experiences in psychotherapy In Castonguay LG & Hill CE (Eds.), Transformation in psychotherapy: Corrective experiences across cognitive behavioral, humanistic, and psychodynamic approaches (pp. 121–139). Washington, DC: American Psychological Association. [Google Scholar]
- Cottrell DJ, Wright-Hughes A, Collinson M, Boston P, Eisler I, Fortune S, … Farrin AJ (2018). Effectiveness of systemic family therapy versus treatment as usual for young people after self-harm: A pragmatic, phase 3, multicentre, randomised controlled trial. The Lancet Psychiatry, 5(3), 203–216. doi: 10.1016/S2215-0366(18)30058-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Curry JF (2014). Future directions in research on psychotherapy for adolescent depression. Journal of Clinical Child & Adolescent Psychology, 43(3), 510–526. doi: 10.1080/15374416.2014.904233 [DOI] [PubMed] [Google Scholar]
- Curry J, Rohde P, Simons A, Silva S, Vitiello B, Kratochvil C, … March J (2006). Predictors and moderators of acute outcome in the Treatment for Adolescents with Depression Study (TADS). Journal of the American Academy of Child and Adolescent Psychiatry, 45(12), 1427–1439. doi: 10.1097/01.chi.0000240838.78984.e2 [DOI] [PubMed] [Google Scholar]
- DeRubeis RJ, Cohen ZD, Forand NR, Fournier JC, Gelfand LA, & Lorenzo-Luaces L (2014). The personalized advantage index: Translating research on prediction into individualized treatment recommendations. A demonstration. PLoS ONE, 9(1), e83875. doi: 10.1371/journal.pone.0083875 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond GS, Diamond GM, & Levy SA (2014). Attachment-based family therapy for depressed adolescents. Washington, DC: American Psychological Association. [Google Scholar]
- Diamond GS, Kobak RR, Ewing ESK, Levy SA, Herres JL, Russon JM, & Gallop RJ (2019). A randomized controlled trial: Attachment-based family and non-directive supportive treatments for youth who are suicidal. Journal of the American Academy of Child and Adolescent Psychiatry, 58(7), 721–731. doi: 10.1016/j.jaac.2018.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond G, Russon J, & Levy S (2016). Attachment-based family therapy: A review of the empirical support. Family Process, 55(3), 595–610. doi: 10.1111/famp.12241 [DOI] [PubMed] [Google Scholar]
- Feeny NC, Silva SG, Reinecke MA, McNulty S, Findling RL, Rohde P, … March JS (2009). An exploratory analysis of the impact of family functioning on treatment for depression in adolescents. Journal of Clinical Child & Adolescent Psychology, 38(6), 814–825. doi: 10.1080/15374410903297148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glenn CR, Franklin JC, & Nock MK (2015). Evidence-based psychosocial treatments for self-injurious thoughts and behaviors in youth. Journal of Clinical Child & Adolescent Psychology, 44(1), 1–29. doi: 10.1080/15374416.2014.945211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gudiño OG, Lau AS, Yeh M, McCabe KM, & Hough RL (2009). Understanding racial/ethnic disparities in youth mental health services. Journal of Emotional and Behavioral Disorders, 17(1), 3–16. doi: 10.1177/1063426608317710 [DOI] [Google Scholar]
- Gunlicks-Stoessel M, Mufson L, Jekal A, & Turner JB (2010). The impact of perceived interpersonal functioning on treatment for adolescent depression: IPT-A versus treatment as usual in school-based health clinics. Journal of Consulting and Clinical Psychology, 78(2), 260–267. doi: 10.1037/a0018935 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak R, Zajac K, Abbott C, Zisk A, & Bounoua N (2017). Atypical dimensions of caregiver-adolescent interaction in an economically disadvantaged sample. Development and Psychopathology, 29, 405–416. doi: 10.1017/S0954579417000074 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobak R, Zajac K, Herres J, & Ewing ESK (2015). Attachment based treatments for adolescents: The secure cycle as a framework for assessment, treatment, and evaluation. Attachment & Human Development, 17(2), 220–239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhlberg JA, Peña JB, & Zayas LH (2010). Familism, parent-adolescent conflict, self-esteem, internalizing behaviors and suicide attempts among adolescent Latinas. Child Psychiatry and Human Development, 41(4), 425–440. doi: 10.1007/s10578-010-0179 [DOI] [PubMed] [Google Scholar]
- Levy SA, & Diamond GS (2010). Family-enhanced non-directive supportive therapy manual. Philadelphia, PA: Unpublished manuscript. [Google Scholar]
- Lyons-Ruth K, Hennighausen K, & Holmes B (2005). Goal-corrected partnership in adolescence coding system (GPACS): Coding manual. Cambridge, MA: Department of Psychiatry, Harvard Medical School; Unpublished manuscript. [Google Scholar]
- Merikangas KR, He J, Burstein ME, Swendsen J, Avenevoli S, Case B, … Olfson M (2011). Service utilization for lifetime mental disorders in U.S. adolescents: Results of the National Comorbidity Survey Adolescent Supplement (NCS-A). Journal of the American Academy of Child and Adolescent Psychiatry, 50(1), 32–45. doi: 10.1016/j.jaac.2010.10.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda J, Nakamura R, & Bernal G (2003). Including ethnic minorities in mental health intervention research: A practical approach to a long-standing problem. Culture, Medicine and Psychiatry, 27(4), 467–486. [DOI] [PubMed] [Google Scholar]
- Newman BM, Newman PR, Griffen S, O’Connor K, & Spas J (2007). The relationship of social support to depressive symptoms during the transition to high school. Journal of Adolescence, 42(167), 441–459. [PubMed] [Google Scholar]
- Nock MK, & Ferriter C (2005). Parent management of attendance and adherence in child and adolescent therapy: A conceptual and empirical review. Clinical Child and Family Psychology Review, 8(2), 149–166. doi: 10.1007/s10567-005-4753-0 [DOI] [PubMed] [Google Scholar]
- Obsuth I, Hennighausen K, Brumariu LE, & Lyons-Ruth K (2014). Disorganized behavior in adolescent-parent interaction: Relations to attachment state of mind, partner abuse, and psychopathology. Child Development, 85(1), 370–387. doi: 10.1111/cdev.12113 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Raudenbush SW, & Bryk AS (2002). Hierarchical linear models: Applications and data analysis methods. Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Rengasamy M, Mansoor BM, Hilton R, Porta G, He J, Emslie GJ, … Brent DA (2013). The bi-directional relationship between parent-child conflict and treatment outcome in treatment-resistant adolescent depression. Journal of the American Academy of Child & Adolescent Psychiatry, 52(4), 370–377. doi: 10.1016/j.jaac.2013.01.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Restifo K, & Bögels S (2009). Family processes in the development of youth depression: Translating the evidence to treatment. Clinical Psychology Review, 29(4), 294–316. doi: 10.1016/j.cpr.2009.02.005 [DOI] [PubMed] [Google Scholar]
- Reyes-Portillo JA, McGlinchey EL, Yanes-Lukin PK, Turner JB, & Mufson L (2017). Mediators of interpersonal psychotherapy for depressed adolescents on outcomes in Latinos: The role of peer and family interpersonal functioning. Journal of Latina/o Psychology, 5(4), 248–260. doi: 10.1037/lat0000096 [DOI] [Google Scholar]
- Reynolds W (1988). SIQ professional manual. Odessa, FL: Psychological Assessment Resources. [Google Scholar]
- Rohde P, Seeley JR, Kaufman NK, Clarke GN, & Stice E (2006). Predicting time to recovery among depressed adolescents treated in two psychosocial group interventions. Journal of Consulting and Clinical Psychology, 74(1), 80–88. doi: 10.1037/0022-006X.74.1.80 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosselló J, & Bernal G (1999). The efficacy of cognitive-behavioral and interpersonal treatments for depression in Puerto Rican adolescents. Journal of Consulting and Clinical Psychology, 67(5), 734–745. [DOI] [PubMed] [Google Scholar]
- Rueger SY, Malecki CK, & Demaray MK (2010). Relationship between multiple sources of perceived social support and psychological and academic adjustment in early adolescence: Comparisons across gender. Journal of Youth and Adolescence, 39, 47–61. doi: 10.1007/s10964-008-9368-6 [DOI] [PubMed] [Google Scholar]
- Sheeber LB, Davis B, Leve C, Hops H, & Tildesley E (2007). Adolescents’ relationships with their mothers and fathers: Associations with depressive disorder and subdiagnostic symptomatology. Journal of Abnormal Psychology, 116(1), 144–154. doi: 10.1037/0021-843X.116.1.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shpigel MS, Diamond GM, & Diamond GS (2012). Changes in parenting behaviors, attachment, depressive symptoms, and suicidal ideation in attachment-based family therapy for depressive and suicidal adolescents. Journal of Marital & Family Therapy, 38(s1), 271–283. doi: 10.1111/j.1752-0606.2012.00295.x [DOI] [PubMed] [Google Scholar]
- Silva C, & Van Orden KA (2018). Suicide among Hispanics in the United States. Current Opinion in Psychology, 22, 44–49. doi: 10.1016/j.copsyc.2017.07.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stanley B, & Brown GK (2012). Safety planning intervention: A brief intervention to mitigate suicide risk. Cognitive and Behavioral Practice, 19(2), 256–264. doi: 10.1016/j.cbpra.2011.01.001 [DOI] [Google Scholar]
- Stark KD, Humphrey LL, Crook K, & Lewis K (1990). Perceived family environments of depressed and anxious children: Child’s and maternal figure’s perspectives. Journal of Abnormal Child Psychology, 18(5), 527–547. [DOI] [PubMed] [Google Scholar]
- Young JF, Benas JS, Schueler CM, Gallop R, Gillham JE, & Mufson L (2016). A randomized depression prevention trial comparing interpersonal psychotherapy-adolescent skills training to group counseling in schools. Prevention Science, 17(3), 314–324. doi: 10.1007/s11121-015-0620-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young JF, Gallop R, & Mufson L (2009). Mother-child conflict and its moderating effects on depression outcomes in a preventive intervention for adolescent depression. Journal of Clinical Child & Adolescent Psychology, 38(5), 696–704. doi: 10.1080/15374410903103577 [DOI] [PubMed] [Google Scholar]
- Young AS, & Rabiner D (2015). Racial/ethnic differences in parent-reported barriers to accessing children’s health services. Psychological Services, 12(3), 267–273. doi: 10.1037/a0038701 [DOI] [PMC free article] [PubMed] [Google Scholar]