Abstract
Abdominal hernias are usually located in the inguinal canals. Differential diagnosis of hernias should consider other pathologies, which typically occur at this site. The aim of this review paper is to present fat-containing lesions located in the inguinal canal based on both our own experience and literature. The first part of the paper describes the embryogenesis and differences in the structure and content of male and female inguinal canal. The canal is clearly wider in men, which results from the presence of the spermatic cord and its components. The female canal contains only the narrow round ligament of the uterus. The second part of the paper discusses the incorrect use of the term “lipoma” for retroperitoneal fat, which penetrated into the lumen of the patent processus vaginalis – the authors using this term acknowledge its incorrectness. These lesions often coexist with oblique inguinal hernia and should be excised during a surgery as they may cause inguinal pain. As for other fat-containing inguinal pathologies, we discussed lipomatosis of the spermatic cord, liposarcoma and the greater omentum. Differential diagnosis of these lesions considers their echogenicity, echostructure and vascularity. Furthermore, attention was paid to the adipose tissue surrounding the lower epigastric vessels, which may be incorrectly localized in the inguinal canal. Finally, the importance of proper diagnostic methodology and knowledge of the inguinal anatomy for the correct ultrasonographic diagnosis was emphasized.
Keywords: inguinal canal, anatomy, fat-containing lesions, differential diagnosis, ultrasonography
Introduction
There are several sites of reduced strength in the abdominal wall. Symmetrical inguinal canals, which are the most common location of hernia, are one of such sites. Furthermore, other pathological lesions that should be included in the differential diagnosis may be found here. The aim of the paper is to present fat-containing lesions located in the inguinal canal based on both our own experience and literature.
Embryogenesis and differences in the structure and content of the male and female inguinal canal
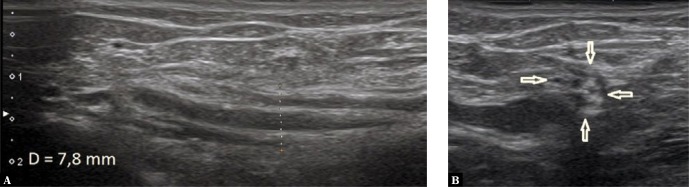
The inguinal canal is formed in the third trimester of pregnancy or, in some cases, in the first year of life. The development of this tissue tunnel is accompanied by the descent of the gonads to the pelvis, particularly the testes, which penetrate through the anterior hypogastric wall to the scrotum, pulling behind the fascia, the transverse and internal oblique muscle fibers and the parietal peritoneum. In the earlier period (about 7 weeks gestation), a gubernaculum occurs, comprised mostly of connective tissue, whose role is to pave the way for and support testicular descent. The peritoneal vaginal process develops during this period, which initially takes the form of a peritoneal recess, to later close and fuse with the spermatic cord, and finally close the inguinal canal. When this process is impaired, retroperitoneal fat or, less commonly, peritoneal viscera or fluid may penetrate into the patent vaginal process, which will clinically manifest as a (potentially painful) tissue bulge at this site. The inguinal canal is mostly made of fascia, aponeurosis and muscle fibers. The deep inguinal ring is an entrance to the canal, whereas the superficial inguinal ring is the external opening of the canal. In males, the lumen of the inguinal canal, which is 3–4 cm long, is tightly filled with the spermatic cord along with its vessels and nerves (Fig. 1 A and B). The female canal, which is narrower and shorter, contains only the round ligament of the uterus, which extends to the large pudendal lip (Fig. 2). The female canal is referred to as the “canal of Nuck” in English literature. It should be noted that the inferior portion of the inguinal canal is adjacent to the inguinal ligament, which extends between the upper anterior iliac spine and the pubic tubercle(1–6). Furthermore, the inferior epigastric vessels, which are located posteriorly to the inguinal canal and medially of the internal inguinal ring, are an important diagnostic landmark(1–6). These structures help properly apply a linear transducer of at least 7 MHz. When scanning the canal in the long axis, the transducer should be placed parallel, just above the inguinal ligament, whereas transverse scanning should be used to visualize its width. The use of Doppler option to visualize the vasculature of the spermatic cord may help ensure correct imaging site (Fig. 3). Convex transducer (3–5 MHz) may prove helpful in obese patients. Functional tests, such as the cough test and the Valsalva maneuver, as well as transducer compression and scanning in a standing position, are important elements of the assessment(4,6).
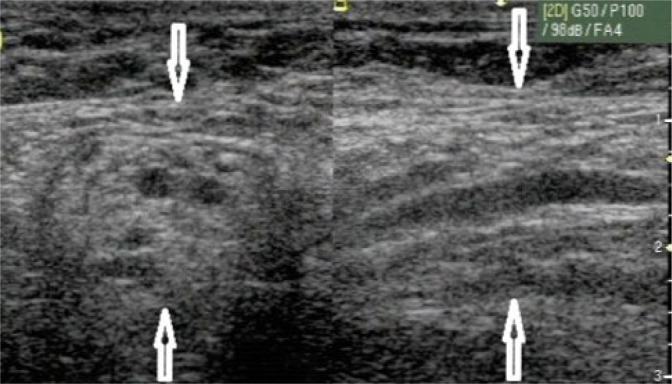
Fig. 1.
A. A longitudinal view of the inguinal canal with the spermatic cord marked with distance indicators. B. The same inguinal canal as in Fig. 1 A, but in cross-section (arrows)
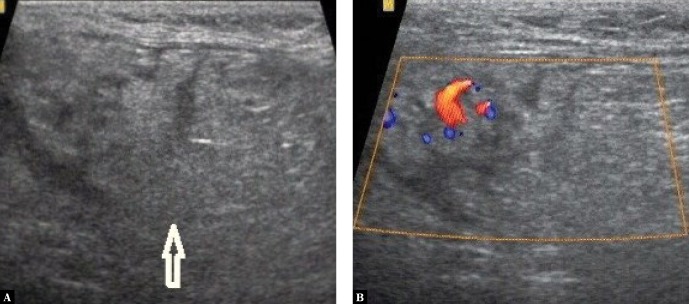
Fig. 2.
An inguinal canal in a female with hernia containing retroperitoneal fat (L). Arrows indicate the round ligament of the uterus
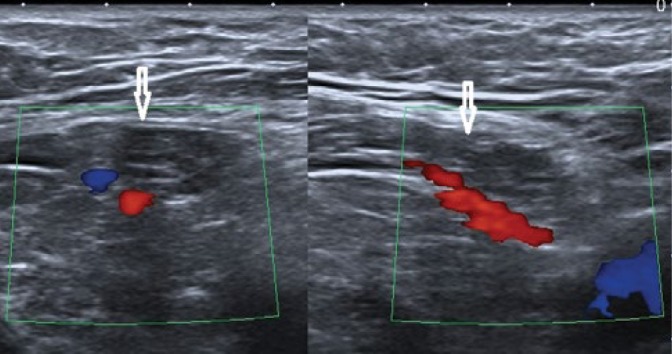
Fig. 3.
Vascularization of the spermatic cord in the inguinal canal.
Fat-containing lesions in the inguinal canal
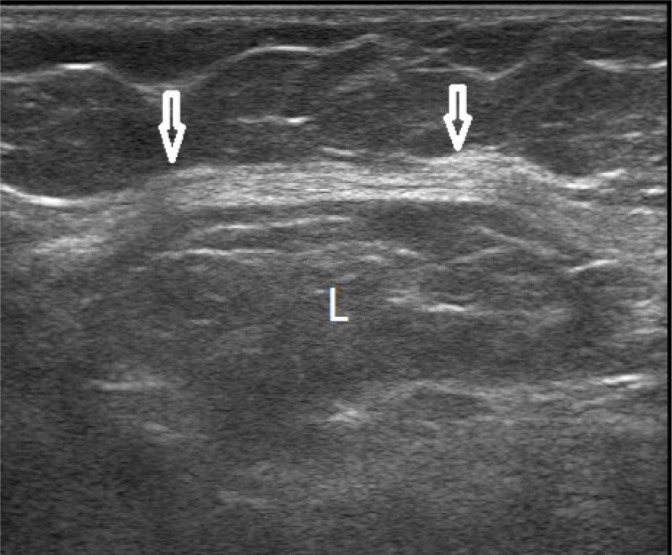
Lipomatosis of the spermatic cord
In obese men, the spermatic cord shows uniform thickening, enhanced echogenicity and a large diameter (Fig. 4). During the Valsalva maneuver, a minor sliding may be observed, which should not be misinterpreted as a movable hernia(2).
Fig. 4.
Spermatic cord with fatty deposits in the inguinal canal in two sections (arrows)
Retroperitoneal fat
In many publications, the term “spermatic cord lipoma” or “round ligament lipoma” is used to refer to retroperitoneal fat despite the fact that the authors using this term are aware of its inaccuracy(7–11). This form of fat is encountered intraoperatively in 2.3 to 72.3% of cases(7–11). As already mentioned, the peritoneal vaginal process may not close during embryogenesis, forming an open space along the long axis of the canal. This space is usually filled by different combinations of intestines, greater omentum or peritoneal fluid. Retroperitoneal fat enters the inguinal canal usually with overgrown vaginal process. Our non-published studies on inguinal hernia (n = 575) indicate that in a vast majority of cases (n = 486; 84.5%), the clinical picture of inguinal hernia was only due to the presence of retroperitoneal fat in the inguinal canal. The accumulated fat presented as structures varying in size, usually oblong, well delineated, homogeneous, slightly hypoechoic, plastic and with varying compliance to transducer compression (Fig. 5). A closer analysis of their echostructure revealed delicate hyperechoic bands corresponding to connective tissue septa. In the case of further doubts, their appearance may be compared with that of lumbar retroperitoneal fat (Fig. 6). Color Doppler shows no vascularization in the lesion.
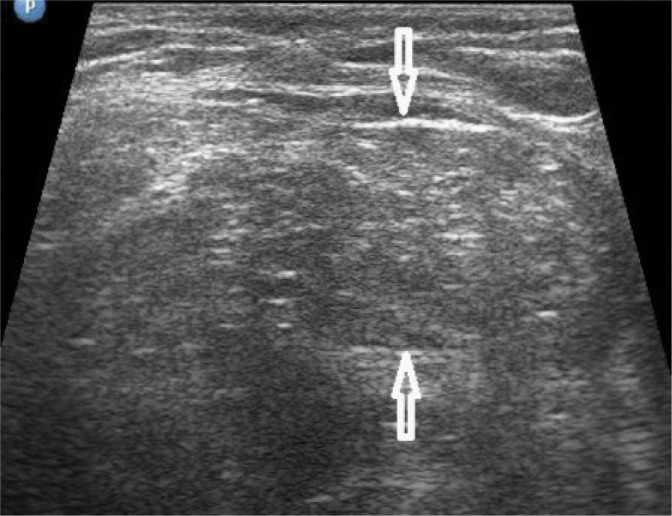
Fig. 5.

Retroperitoneal fat filling the patent processus vaginalis (arrows). Narrow echogenic bands corresponding to connective tissue septa are visible in the mass
Fig. 6.
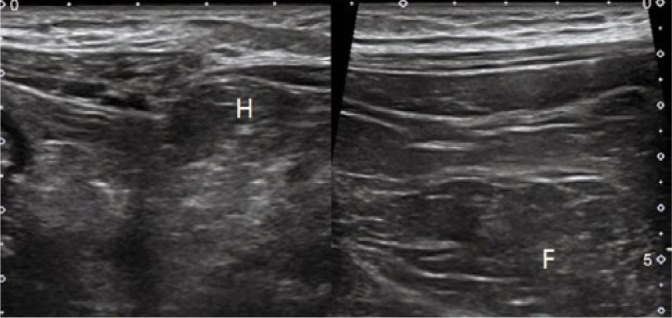
Acoustic similarity between the fat in the inguinal hernia (H) and the retroperitoneal fat (F)
The greater omentum
The greater omentum is a structure morphologically similar to preperitoneal fat. It is plastic, non-vascularized in color Doppler, with a mosaic echostructure and slightly higher echogenicity compared to the retroperitoneal fat. It connects with a mass of similar appearance located under the anterior abdominal wall rather than the fat in the lumbar region (Fig. 7). Ultrasonography enables the differentiation between the greater omentum and a pseudolipoma; however, we found no literature data to support this.
Fig. 7.
The greater omentum in the hernial sac shows mosaic echostructure (arrows)
Lipoma (true)
Lipoma is a benign encapsulated tumor, sometimes with distinct lobar structure, usually spindle-shaped and showing higher echogenicity compared to subcutaneous fat (Fig. 8). Lipomas with low stromal content may show lower echogenicity. The absence of connection with abdominal fat and the usual absence of vascularization in color Doppler are important features of this tumor. It is suggested that lipoma develops from the remnant gubernacular fat(6,12–15).
Fig. 8.

Lipoma (L) in the form of a hyperechoic mass located in the inguinal canal
A hibernoma, i.e. lipoma originating from brown fat tissue, is a rare finding. It shows thermo-energetic properties. The tumor showed mixed echogenicity in a case report presented by San Miguel et al.(16)
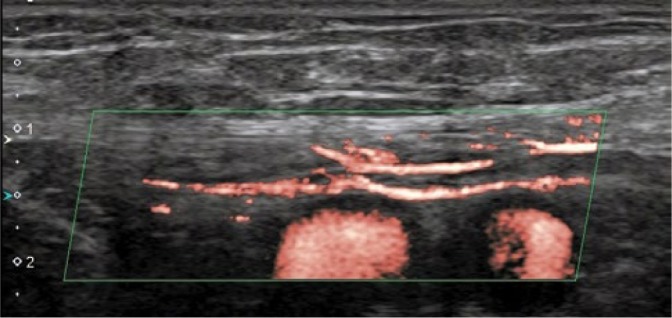
Liposarcoma
Only 5% of all sarcomas, which are classified into 50 types, are located in the genitourinary tract. Liposarcoma (37%) and leiomyosarcoma (24%) are most commonly found in the inguinal canal. Malignant histiocytic fibroma comes third (10%), whereas fibrosarcomas come fourth (5%). Liposarcomas are usually large, rapidly growing, solid and usually heterogeneous. They display chaotic vascular pattern in Doppler ultrasound (Fig. 9 A and B). Although the tumor shows locally aggressive growth pattern, lymph node involvement and blood dissemination are uncommon. Radical orchiectomy and high resection of the spermatic cord, combined with radiation therapy in some cases, is an optimal management in this pathology(6,15,17–19). In doubtful cases, computed tomography (CT) or magnetic resonance imaging (MRI) should be performed, which allow for a more accurate assessment of the ongoing inguinal pathological processes(6,15). Ultrasound-guided biopsy may be needed in some cases.
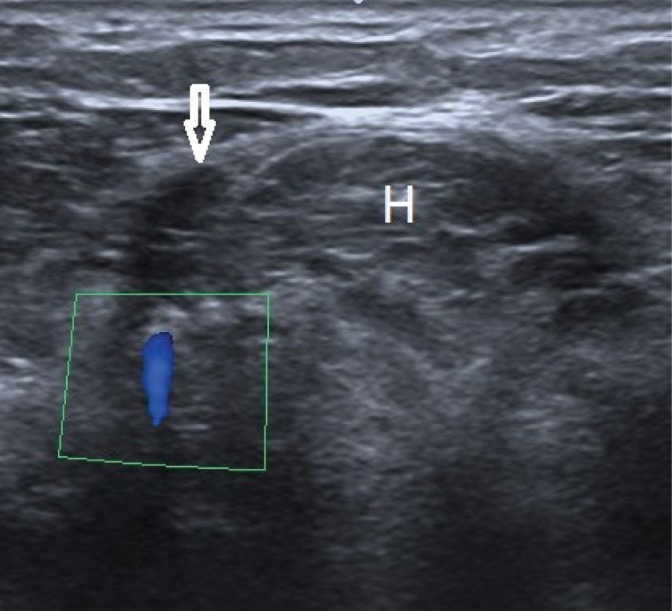
Fig. 9.
A. Liposarcoma in the inguinal canal showing heterogeneous echostructure. B. The same liposarcoma as in Fig. 9A. Pathological vascular pattern seen in color Doppler
Differential diagnosis
Differential diagnosis of the above mentioned lesions should include many pathologies that can mimic them. First of all, the fat tissue surrounding the epigastric vessels should be mentioned. Its appearance is identical to that of retroperitoneal fat filling the hernial sac (Fig. 10). The exact topography of these vessels along with the fat cuff is shown in Fig. 11.
Fig. 10.
A cross-section showing hernial fat (H) and fat surrounding the inferior epigastric vessels (arrow)
Fig. 11.
Fat surrounding the inferior epigastric vessels – two sections (arrows)
The true lipoma can be also mimicked by a lymph node affected by lipomatosis (Fig. 12); however it is located outside the inguinal canal. An undescended testicle present in the inguinal canal should be also mentioned. It usually manifests as a slightly hypoechoic lesion (Fig. 13). Therefore, the importance of a comprehensive ultrasonographic assessment in men, including the groin and the scrotum, should be emphasized. Similarly, an ovary may be found in the female inguinal canal. A precise assessment usually allows to identify the Graafian follicles (Fig. 14). Pelvic assessment to check for a potentially missing ovary is also important. An echogenic tumor may be sometimes mimicked by an intestine in the hernial sac (Fig. 15). In such cases, doubts can be resolved by repeated ultrasound after an intake of 500 mL of water by the patient. An incarcerated omentum will produce a similar ultrasound picture. The imaging conditions in this region are significantly compromised by postoperative scars, sutures and meshes. Differential diagnosis should include local primary and secondary proliferative lesions, which requires the diagnosis to be extended with CT or MRI.
Fig. 12.

A lymph node with fatty deposits (n) mimicking lipoma in the inguinal canal
Fig. 13.
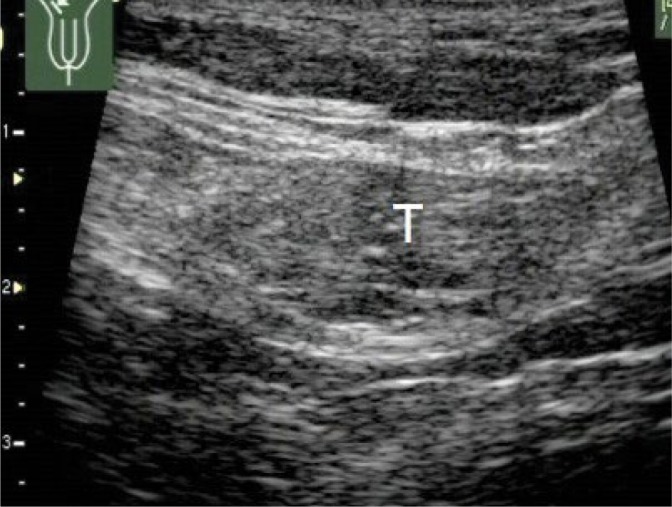
An undescended testicle (T) in the inguinal canal mimicking a pathological lesion
Fig. 14.

An ovary with 30 mm cyst is seen in the inguinal canal
Fig. 15.

An echogenic mass in the hernial sac is a compressed small intestinal loop (I). Arrows indicate the deep inguinal ring
Conclusions
Ultrasonography is a method of choice in the diagnosis of inguinal lesions provided that proper methodology and adequate anatomical knowledge are ensured. Differential diagnosis should include many clinically insignificant and significant lesions to ensure accurate diagnosis. In the case of doubts, CT or MRI and, in justified cases, ultrasound-guided biopsy, should be the next diagnostic step.
Footnotes
Conflict of interest
The authors do not report any financial or personal connections with other persons or organizations, which might negatively affect the contents of this publication and/or claim authorship rights to this publication.
References
- 1.Bochenek A, Reicher M: Anatomia człowieka. Tom 1 Wydawnictwo Lekarskie PZWL; Warszawa: 1998. [Google Scholar]
- 2.Woodward PJ, Schwab CM, Sesterhum C, Szklaruk IA: From the archives of the AFIP: Extratesticular scrotal masses: radiologic-pathologic correlation. Radiographics 2003; 23: 15–40. [DOI] [PubMed] [Google Scholar]
- 3.Khanna PC, Ponsky T, Zagol B, Lukish JR, Markle BM: Sonographic appearance of canal of Nuck hydrocele. Pediatr Radiol 2007: 37: 603–606. [DOI] [PubMed] [Google Scholar]
- 4.Garriga V, Serrano A, Marin A, Medrano S, Roson N, Pruna X: US of tunica vaginalis testis: anatomic relationships and pathologic conditions. Radiographics 2009; 29: 2017–2032. [DOI] [PubMed] [Google Scholar]
- 5.Yoong P, Duffy S, Marshall TJ: The inguinal and femoral canals: A practical step-by-step approach to accurate sonographic assessment. Indian J Radiol Imaging 2013; 23: 391–395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Revzin MV, Ersahin D, Israel GM, Kirsch JD, Mathur M, Bokhari J. et al. : US of inguinal canal: comprehensive review of pathologic processes with CT and MR imaging correlation. Radiographics 2016; 36: 2028–2048. [DOI] [PubMed] [Google Scholar]
- 7.van den Berg JC, de Valois JC, Go PM, Rosenbusch G: Detection of groin hernia with physical examination, ultrasound, and MRI compared with laparoscopic findings. Invest Radiol 1999; 34: 739–743. [DOI] [PubMed] [Google Scholar]
- 8.Lilly MC, Arreguni ME: Lipomas of the cord and round ligament. Ann Surg 2002; 235: 586–590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carilli S, Alper A, Emre A: Inguinal canal “lipoma”. Hernia 2004; 8: 252–254. [DOI] [PubMed] [Google Scholar]
- 10.Faatar S: CT of inguinal canal lipomas and fat-containing inguinal hernias. J Med Imaging Radiat Oncol 2011; 55: 485–492. [DOI] [PubMed] [Google Scholar]
- 11.Yener O, Demir M, Yigitbaşı R, Yilmaz A: Missed lipoma of the spermatic cord. Praque Med Rep 2013; 114: 5–8. [DOI] [PubMed] [Google Scholar]
- 12.Heller CA, Marucci DD, Dunn T, Barr EM, Houang M, Dos Remedios C: Inguinal canal “lipoma”. Clin Anat 2002; 15: 280–285. [DOI] [PubMed] [Google Scholar]
- 13.Gokhale S: Sonography in identification of abdominal wall lesions presenting as palpable masses. J Ultrasound Med 2006; 25: 1199–1209. [DOI] [PubMed] [Google Scholar]
- 14.Cavazzola LT, Lieberknecht M, Machado AS, Farias FR: Giant lipoma of spermatic cord. Am J Surg 2009; 198: e54–e55. [DOI] [PubMed] [Google Scholar]
- 15.Vagnoni V, Brunocilla E, Schiavina R, Borghesi M, Passaretti G, Gentile G. et al. : Inguinal canal tumors of adulthood. Anticancer Res 2013; 33: 2361–2368. [PubMed] [Google Scholar]
- 16.San Miguel P, Clemente LM, García Gonzáles R, Fernández E: Hibernoma of the spermatic cord. The second report case and literature review. Scand J Urol Nephrol 1998; 32: 53–55. [DOI] [PubMed] [Google Scholar]
- 17.Peyrí Rey E, Urban Ramón A, Martínez Fernández M, Sanmarti Da Silva B: [Dedifferentiated liposarcoma of spermatic cord: degeneration of lipoma previously resected]. Actas Urol Esp 2003; 27: 383–386. [DOI] [PubMed] [Google Scholar]
- 18.Hassan JM, Quisling SV, Melvin WV, Sharp KW: Liposarcoma of the spermatic cord masquerading as an incarcerated inguinal hernia. Am Surg 2003; 69: 163–165. [PubMed] [Google Scholar]
- 19.Kitsukawa S, Samejima T, Aizawa T, Noda K, Matsumoto T: [A case of liposarcoma of spermatic cord]. Hinyakika Kiyo 2006; 52: 227–229. [PubMed] [Google Scholar]