Abstract
Internalization of the thin-ideal is a risk factor for eating disorders that frequently persists into recovery and increases patient risk for relapse. Addressing thin-ideal internalization as a core element of eating disorder prevention and treatment produces significant reductions in eating pathology. However, research has not yet quantified levels of thin-ideal internalization that may signal increased versus decreased risk for disordered eating. To address this gap in the literature, receiver operating characteristic (ROC) curve analysis was used to identify a thin-ideal internalization cutoff score that signified clinically-meaningful eating disorder pathology. 787 college women (age M = 20.17, SD = 2.41; BMI M = 23.58, SD = 5.29) were classified as “healthy” (N = 717) or those with significant disordered eating (N = 70) using established clinical cutoffs for the Eating Disorder Examination-Questionnaire. ROC curve analysis was used to test the performance of the Sociocultural Attitudes Towards Appearance Questionnaire-4 (SATAQ-4) Internalization: Thin/Low Body Fat subscale in predicting disordered eating status, and to identify a cutoff score that maximized sensitivity and specificity to discriminate between healthy and disordered eating samples. Mean SATAQ-4 internalization scores were 3.29 (SD = 0.92) and 4.27 (SD = 0.62) for healthy and disordered eating participants, respectively. The SATAQ-4 internalization scores were good predictors of disordered eating status (area under the curve = 0.81, 95% CI: 0.76–0.86). The optimal cutoff of 3.78 (measured on a 1–5 Likert scale) yielded a sensitivity of 0.81 and specificity of 0.64. Overall, results provide preliminary support for the discriminant validity of SATAQ-4 thin internalization scores and suggest that even moderate levels of thin-ideal internalization may be predictive of clinically-significant eating pathology. It may be important for prevention and intervention work to actively seek to reduce internalization levels below this clinical cutoff, though future work is needed to bear this out.
Keywords: Thin-ideal internalization, Sociocultural, Risk factor, Body image, Eating disorders
Introduction
Internalization of appearance ideals is the degree to which an individual “buys into socially defined ideals of attractiveness” [1] and plays a central role in sociocultural models of disordered eating onset and maintenance [2, 3]. Among women, internalization of the thin ideal is theorized to engender body dissatisfaction and subsequent disordered eating as individuals seek to achieve an often unobtainable ideal physique. A plethora of correlational, experimental, and prospective research supports the influence of thin-ideal internalization on body image and eating disturbance [4, 5]. Indeed, thin-ideal internalization is one of the few identified risk factors with sufficient empirical evidence to support its proposed role as a causal risk factor for disordered eating [1, 6]. Further, evidence indicates that thin-ideal internalization frequently persists into eating disorder recovery and predicts heightened risk of relapse [7, 8]. Given this, interventions have targeted thin-ideal internalization to reduce risk for eating pathology.
A number of eating disorder prevention programs designed to decrease thin-ideal internalization have produced reductions in both internalization and eating disorder symptoms [9-11]. Among them, Stice’s dissonance-based intervention, the “Body Project,” has undergone the most rigorous empirical investigation, yielding consistent support for the approach in both efficacy and effectiveness trials [12]. Given the well-documented causal associations between thin-ideal internalization and eating pathology, Stice and colleagues recently adapted the successful dissonance-based prevention program into a frontline treatment approach for individuals with diagnosed eating disorders, which they refer to as “counter attitudinal therapy” [13]. Preliminary support for the treatment approach suggests that targeting thin-ideal internalization produces large reductions in both internalization and eating disorder symptoms among clinically ill individuals [13].
In sum, research suggests that thin-ideal internalization is causally related to disordered eating, and that reductions in internalization relate to reductions in eating pathology. However, research has not yet quantified specific levels of thin-ideal internalization that may signal increased versus decreased risk for disordered eating. Such information is likely to be clinically useful for identifying at-risk individuals and clarifying target levels of internalization for individuals engaged in prevention or treatment programs. The sociocultural attitudes towards appearance questionnaire-4-thin/low body fat subscale (SATAQ-4-Thin) is a well-validated and widely accessible assessment of thin-ideal internalization [14]. In the current study, receiver operating characteristic (ROC) curve analysis was used to (a) examine the utility of the SATAQ-4-Thin in distinguishing individuals with and without significant eating pathology, and (b) identify a SATAQ-4-Thin cutoff score that signified clinically meaningful eating disorder pathology. This cutoff might then be applied in clinical settings to identify individuals with clinically significant internalization, inform treatment goals, or evaluate treatment effectiveness.
Method
Participants
Participants were 787 female undergraduates attending a large Southeastern university. They ranged in age from 18 to 30, with a mean age of 20.17 (SD = 2.41). Sixty-one percent of the sample self-identified as Caucasian, 12.0% as Hispanic or Latina, 12% as Black or African American, 3.7% as Asian, 0.5% as American Indian or Alaskan Native, 0.5% as Native Hawaiian or Pacific Islander, and 9.9% as multiracial or other. The average body mass index (BMI; kg/m2) of the sample was 23.58 (SD = 5.29).
Measures
Demographic information
A demographic questionnaire asked participants to indicate their age, race/ethnicity, height, and weight. Self-reported height and weight were then used to calculate BMI.
Sociocultural Attitudes Towards Appearance Questionnaire-4 Internalization: Thin/Low Body Fat subscale
The 5-item Internalization: Thin/Low Body Fat subscale of the SATAQ-4 [14] assesses an individual’s personal desire for a thin physique (example item: “I want my body to look very thin”) and degree of cognitive energy spent thinking about achieving this physique (example item: “I think a lot about having very little body fat”). Respondents are asked to indicate their level of agreement with each item using a 5-point Likert scale ranging from 1 (definitely disagree) to 5 (definitely agree). Higher scores on the subscale indicate higher levels of thin-ideal internalization. Cronbach’s alpha in the current sample was 0.87.
Eating Disorder Examination-Questionnaire (EDE-Q)
The EDE-Q [15] is a 28-item measure assessing disordered eating attitudes and behaviors over the last 28 days (example item: “Have you been deliberately trying to limit the amount of food you eat to influence your shape or weight?”). Items are rated on a 7-point Likert-type scale ranging from 0 (no days/not at all) to 6 (everyday/markedly). The EDE-Q yields four subscale scores assessing restraint, shape concern, weight concern, and eating concern. The current study utilized the global score, representing an average of the four subscale scores. Higher global scores indicate greater levels of eating pathology. In the current sample, internal consistency for the global score was 0.95.
Procedure
Participants were recruited through the university’s undergraduate research pool. Informed consent was provided electronically and measures were completed online via secure survey software. Participants were debriefed and received extra course credit upon completion. All study procedures were approved by the university’s Institutional Review Board.
Data analyses
Established clinical cutoffs on the EDE-Q (i.e., global score of 4.0) were used to dichotomize the sample into “healthy” participants (EDE-Q < 4) and those with significant disordered eating (EDE-Q ≥ 4) [16]. As individuals with elevated disordered eating were expected to demonstrate higher SATAQ-4-Thin scores, t tests were used to examine mean differences in SATAQ-4-Thin scores between healthy and disordered eating samples. Finally, ROC curve analysis was used to test the performance of the SATAQ-4-Thin in predicting disordered eating status, and to identify a cutoff score that maximized sensitivity (i.e., ability to detect individuals with significant eating pathology) and specificity (i.e., ability to screen out individuals with nonclinical eating pathology) to discriminate between samples. The ROC curve is a graphical representation of a measure’s sensitivity plotted against its false-positive rate (i.e., 1-specificity). The area under the curve (AUC) summarizes a test’s overall accuracy, or ability to distinguish cases from non-cases, based on the average value of sensitivity for all possible values of specificity. Guidelines define AUC values as non-informative (≤ 0.50), less accurate (0.51–0.70), moderately accurate (0.71–0.90), highly accurate (0.91–0.99), and perfect (1) [17]. The optimal cutoff was defined as the SATAQ-4-Thin score that maximized sensitivity and specificity. All analyses were conducted using SPSS Statistics version 23.0.
Results
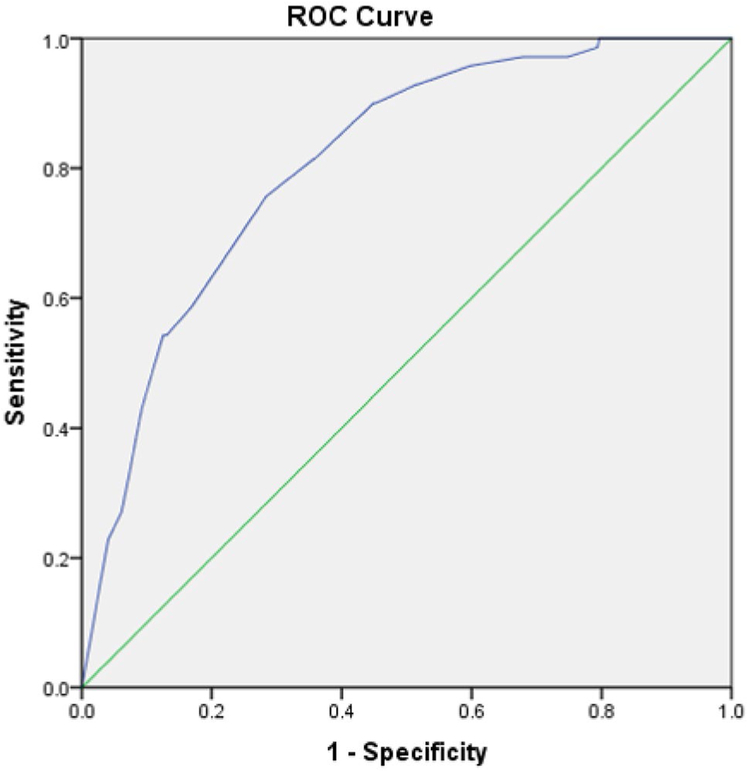
Based on established clinical cutoffs on the EDE-Q, 717 participants were classified as “healthy” (EDE-Q < 4), while 70 participants were categorized as demonstrating significant disordered eating (EDE-Q ≥ 4). T tests indicated significantly lower levels of thin-ideal internalization among healthy participants (M = 3.29, SD = 0.92) compared to those with elevated eating pathology (M = 4.27, SD = 0.62), t (785) = 8.76, p < 0.001. As shown in Fig. 1, SATAQ-4-Thin scores demonstrated moderate accuracy, AUC = 0.81, 95% CI (0.76–0.86). In other words, there is an 81% probability that a randomly selected individual with clinically significant eating pathology would obtain a higher SATAQ-4-Thin score than a randomly selected individual without clinically significant eating pathology. A cutoff score of 2.45 provided the optimal sensitivity (1.0), however, this score was associated with poor specificity (0.20). The cutoff that provided the optimal balance of sensitivity and specificity was a mean SATAQ-4-Thin score of 3.78, which had a sensitivity of 0.81 and a specificity of 0.64.
Fig. 1.
ROC curve analysis showing the area under the curve for the prediction of disordered eating status using the SATAQ-4-Thin. Area under the ROC curve = 0.81; 95% confidence interval 0.76–0.86
Discussion
The current study fills an important gap in the literature by examining the utility of a widely used measure of thin-ideal internalization in (a) identifying individuals with and without significant eating pathology, and (b) identifying an optimal cut score on the SATAQ-4 internalization: thin/low body fat subscale to distinguish those with clinically meaningful levels of internalization. T test and AUC results suggest that higher scores on the SATAQ-4-Thin relate to higher levels of disordered eating, and that the scale has acceptable accuracy in distinguishing between individuals with and without significant eating pathology. Further, results suggest that a cutoff score of 3.78 best differentiates individuals with and without clinically significant thin-ideal internalization. These results suggest that the measure may be clinically useful for identifying individuals with elevated eating disorder symptoms and dangerous levels of internalization. Although brief-eating disorder screening instruments such as the SCOFF are readily available [18], the SATAQ-4-Thin may serve as a meaningful adjunct instrument for treatment programs that target thin-ideal internalization. To adequately reduce risk for eating disorder onset or relapse, it may be important for intervention work to actively seek to reduce internalization levels below this clinical cutoff, though future work is needed to bear this out.
Limitations of the current study suggest avenues for future research. First, although the current study utilized established clinical cutoffs on a validated measure of eating pathology to identify disordered eating status, eating disorder diagnoses were not verified through a clinical diagnostic interview, which is considered to be the gold standard. Therefore, replication utilizing diagnostic interviews (e.g., Structured Clinical Interview for DSM-5 Disorders [19]) to establish eating disorder status represents an important avenue for future work. Second, as the current study examined SATAQ-4-Thin scores among individual with and without clinically significant disordered eating, the identified cutoff is best suited for identifying healthy versus actively ill individuals. Given the promise of prevention programs targeting thin-ideal internalization to ameliorate eating disorder risk, future work should seek to quantify specific levels of internalization (e.g., a SATAQ-4-Thin cutoff) that signifies increased versus decreased risk for future eating disorder onset or increase in symptoms. Such work would have important implications for identifying at-risk individuals who are likely to benefit most from these prevention approaches. Third, examination of score cutoffs among individuals in eating disorder remission or recovery also represents a valuable goal for future research as it is possible that individuals with a history of an eating disorder may be more vulnerable to relapse at lower levels of thin-ideal internalization. Fourth, the current sample is limited in terms of demographic diversity and findings may not generalize to men, younger/older populations, or more ethnically diverse populations. Therefore, future research is needed to clarify the clinical cutoffs on the SATAQ-4 internalization: thin/low body fat subscale among more diverse samples. Finally, although the current study sought to identify a cutoff that maximized both sensitivity (0.81) and specificity (0.64), it is important to note that the identified score demonstrates greater sensitivity than specificity, which is typically preferable in clinical settings. However, it may be preferable to utilize a cutoff that emphasizes specificity in other settings (e.g., research studies).
In sum, this is the first study to conduct a ROC curve analysis to identify a clinical cutoff on the SATAQ-4 internalization: thin/low body fat subscale, a widely used measure of thin-ideal internalization. Results indicate that the scale has good accuracy in identifying individuals with clinical levels of disordered eating, supporting the measure’s utility in clinical settings. Moderate levels of thin-ideal internalization (i.e., mean score of 3.78 on a 1–5 response scale) were found to signal increased risk for clinically significant eating pathology, emphasizing the potential hazard of pursuing a thin figure. Continued work is needed to replicate these findings and examine scale scores in additional populations.
Acknowledgements
This work was supported by the the National Institute of Mental Health (Grant number T32 MH082761). The opinions and assertions expressed herein are those of the authors and are not to be construed as reflecting the views of the USUHS or the U.S. Department of Defense.
Footnotes
Conflict of interest On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Informed consent Informed consent was obtained from all individual participants included in the study.
References
- 1.Thompson JK, Stice E (2001) Thin-ideal internalization: mounting evidence for a new risk factor for body-image disturbance and eating pathology. Curr Dir Psychol Sci 10:181–183. 10.1111/1467-8721.00144 [DOI] [Google Scholar]
- 2.Stice E, Nemeroff C, Shaw H (1996) A test of the dual pathway model of bulimia nervosa: evidence for restrained-eating and affect-regulation mechanisms. J Soc Clin Psychol 15:340–363. 10.1521/jscp.1996.15.3.3403 [DOI] [Google Scholar]
- 3.Thompson JK, Heinberg LJ, Altabe M, Tantleff-Dunn S (1999) Exacting beauty. American Psychological Association, Washington DC [Google Scholar]
- 4.Cafri G, Yamamiya Y, Brannick M, Thompson JK (2005) The influence of sociocultural factors on body image: a meta-analysis. Clin Psychol Sci Pract 12:421–433. 10.1093/clipsy/bpi053 [DOI] [Google Scholar]
- 5.Stice E, Gau JM, Rohde P, Shaw H (2017) Risk factors that predict future onset of each DMS-5 eating disorder: Predictive specificity in high-risk adolescent females. J Abnorm Psychol 126:38–51. 10.1037/abn0000219 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Stice E (2002) Risk and maintenance factors for eating pathology: a meta-analytic review. Psycholl Bull 128:825–848. 10.1037/0033-2909.128.5.825 [DOI] [PubMed] [Google Scholar]
- 7.Bardone-Cone AM, Harney MB, Maldonado CR, Lawson MA, Robinson DP, Smith R, Tosh A (2010) Defining recovery from an eating disorder: conceptualization, validation, and examination of psychosocial functioning and psychiatric comorbidity. Behav Res Ther 48:194–202. 10.1016/j.brat.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Heinberg LJ, Coughlin JW, Pinto AM, Haug N, Brode C, Guarda AS (2008) Validation and predictive utility of the sociocultural attitudes toward appearance questionnaire for eating disorders (SATAQ-ED): internalization of sociocultural ideals predicts weight gain. Body Image 5:279–290. 10.1016/j.bodyim.2008.02.001 [DOI] [PubMed] [Google Scholar]
- 9.Becker CB, Wilson C, Williams A, Kelly M, McDaniel L, Elmquist J (2010) Peer-facilitated cognitive dissonance versus healthy weight eating disorders prevention: a randomized comparison. Body Image 7:280–288. 10.1016/j.bodyim.2010.06.004 [DOI] [PubMed] [Google Scholar]
- 10.Bell MJ, Rodgers RF, Paxton SJ (2017) Towards successful evidence-based universal eating disorders prevention: the importance of zooming out. Eat Behav. 10.1016/j.eatbeh.2016.10.012 [DOI] [PubMed] [Google Scholar]
- 11.McVey G, Tweed S, Blackmore E (2007) Healthy schools-healthy kids: a controlled evaluation of a comprehensive universal eating disorder prevention program. Body Image 4:115–136. 10.1016/j.bodyim.2007.01.004 [DOI] [PubMed] [Google Scholar]
- 12.Becker CB, Stice E (2017) From efficacy to effectiveness to broad implementation: evolution of the body project. J Consult Clin Psych 85:767–782. 10.1037/ccp0000204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Stice E, Rohde P, Butryn M, Menke KS, Marti CN (2015) Randomized controlled pilot trial of a novel dissonance-based group treatment for eating disorders. Behav Res Ther 65:67–75. 10.1016/j.brat.2014.12.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schaefer LM et al. (2015) Development and validation of the sociocultural attitudes towards appearance questionnaire-4 (SATAQ-4). Psychol Assess 27:54–67. 10.1037/a0037917 [DOI] [PubMed] [Google Scholar]
- 15.Fairburn CG, Beglin SJ (2008) Eating Disorder examination questionnaire (EDE-Q 6.0) In: Fairburn CG (ed) Cognitive behavior therapy and eating disorders. Guilford Press, New York, pp 309–314 [Google Scholar]
- 16.Luce KH, Crowther JH, Pole M (2008) Eating disorder examination questionnaire (EDE-Q): norms for undergraduate women. Int J Eat Disord 41:273–276. 10.1002/eat.20504 [DOI] [PubMed] [Google Scholar]
- 17.Swets JA (1988) Measuring the accuracy of diagnostic systems. Science 240:1285–1293 [DOI] [PubMed] [Google Scholar]
- 18.Hill LS, Reid F, Morgan JF, Lacey JH (2010) SCOFF, the development of an eating disorder screening questionnaire. Int J Eat Disord 43:344–351. 10.1002/eat.20679 [DOI] [PubMed] [Google Scholar]
- 19.First MB, Williams JBW, Karg RS, Spitzer RL (2015) Structured clinical interview for DSM-5 disorders, research version (SCID-5-RV). American Psychiatric Association, Arlington [Google Scholar]