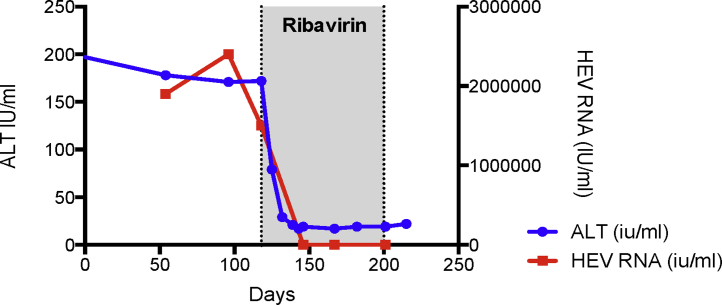
Figure 3.
HEV infection drives the rapid development of cirrhosis in patients on immunosuppressive medication. Patient who had undergone simultaneous heart and kidney transplantation in 2002 and on triple immunosuppression (mycophenolate mofetil, tacrolimus and prednisolone) was referred to liver medicine after having been noted to have deranged liver function. The first noted elevations in serum alanine aminotransferase (ALT) activity was recorded as 94IU/l which coincided with symptoms of malaise, lethargy and diarrhoeal symptoms. The referring team screened him for liver disease, stopped his statin medication and presumptively treated him for cytomegalovirus hepatitis. When his liver biochemistry failed to improve he was referred and seen in liver clinic. He had established liver cirrhosis with significant portal hypertension with median transient elastography at his index liver appointment > 20 kPa. He was subsequently found to have a HEV load of over 2.4 × 106 IU/mL with compatible serology (HEV IgM and IgG positive). Ribavirin was initiated which resulted in a virological and serum ALT response. He is now being followed up as a well-compensated cirrhotic patient by liver outpatient services. The time course from the first biochemical abnormality being detected, to the likely development of chronicity through to confirmed cirrhosis was only 16 months.