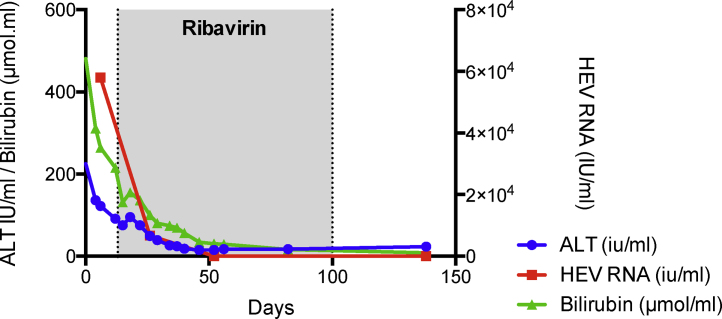
Figure 4.
HEV infection drives the development of acute on chronic liver failure in patients with established cirrhosis. A 54-year-old male who was active on the liver transplant waiting list for non-alcoholic steatohepatitis associated cirrhosis presented with a 10-day history of acute decompensation manifested by the development of jaundice and worsening ascites. His complicated medical history was significant for small bowel Crohn's disease; and he had recently been commenced on an anti-TNFa monoclonal antibody (adalimumab; Humira®) and prednisolone. Testing confirmed acute HEV G3 infection with HEV detectable in both blood and stool by PCR. In contrast to the non-cirrhotic transplant recipient mentioned above, acute HEV infection in this instance resulted in significant liver dysfunction exemplified by coagulopathy, jaundice and ascites. The patient recompensated with ribavirin and exhibited a SVR. Stool HEV PCR was negative at 3 and 6 months post treatment.