Abstract
Antiresorptive drugs (ARDs), such as bisphosphonates or denosumab, that prevent bone resorption are widely used in patients with osteoporosis or with cancer that has metastasized to the bones. Although osteonecrosis of the jaw (ONJ) is a well-documented complication of ARD use, the benefits ARDs outweigh the complication. Thus, research has focused on finding ways to prevent or reduce the risk of developing ONJ. Dentists, as part of a multi-professional team, have a critical role in preventing ONJ. However, many dentists tend to hesitate to provide dental care to patients with ONJ, or tend to think that it is a problem to be dealt with by oral surgeons. This review gives an overview of ARD-related ONJ and provides the guidelines for dental care in patients taking ARDs to lower the risk of developing ONJ.
Keywords: Antiresorptive drugs, Bisphosphonate, Denosumab, Dental care, Osteonecrosis
INTRODUCTION
Bisphosphonates (BPs) are the most widely used antiresorptive drugs (ARDs) for the treatment of osteoporosis. Besides osteoporosis, BPs are also important therapeutic drugs for management of skeletal diseases in neoplasia, hypercalcemia of malignancy, Paget's disease, osteogenesis imperfecta, and fibrous dysplasia [1]. In dentistry, BPs became well-known because of its side effect, BP-related osteonecrosis of the jaw (BRONJ). Since first reported in 2003, several observational studies reported that surgical procedures are major risk factors for the development of BRONJ [2,3,4]. Therefore, dentists, especially oral surgeons, are aware of the link between the complications of ARDs, including BPs, and dental surgery.
Osteonecrosis of the jaw (ONJ) does not respond well to treatment once it has occurred. Therefore, the focus has been on the prevention of ONJ, i.e., avoiding surgical procedures. When the advanced lesion is found, the patient is usually referred to the oral surgeon. However, all dentists could play an important role in the detection of intraoral changes in patients using ARD, thus, helping in preventing complications such as ONJ. When dentists do not have clear guidelines on managing patients using ARD, they might hesitate to provide dental care, or even miss providing necessary treatment. Therefore, this review summarizes our current understanding of ARD-related ONJ based on a literature search. It also suggests guidelines to general dentists when providing dental care to patients using ARD.
REVIEW
Overview of antiresorptive-drugs related osteonecrosis of the jaw (ARONJ)
1. ARDs
ARDs include various types of injections and oral medications (Table 1) [5]. Among them, BPs are a representative ARD most commonly prescribed to treat osteoporosis since the initial launch of alendronates by Merck & Co. [6]. When orally administered, BPs are approved for the treatment of non-malignant bone disorders such as osteoporosis and osteopenia [7,8]. Intravenously administered BPs have also been shown to improve management and prevention of metastatic bone disease, implying that BPs are important adjuvants for cancer treatment, especially breast and prostate cancers [9,10,11]. BPs have a strong affinity for bone and, thus, become embedded in the bone mineral, resulting in the retention of measurable amounts for several years [12].
Table 1. List of antiresorptive drugs.
| Generic name | Brand name | Manufacture | Dosage (application) | Indication | |
|---|---|---|---|---|---|
| Bisphosphonate | |||||
| Zoledronic acid | Zometa | Novartis pharmaceuticals (Novartis Korea) | 4 mg/100 mL (IV) | Hypercalcemia of malignancy, bone complication due to multiple myeloma and bone metastases from solid tumors | |
| Reclat/Aclasta | 5 mg/100 mL (IV) | Osteoporosis, Paget's disease | |||
| Alendronate sodium | Fosamax | Merck & Co. (MSD Korea) | 1, 10, 35, 40, 70 mg (PO) | Osteoporosis, Paget's disease | |
| Fosamax Plus D | 70 mg (PO) | Osteoporosis | |||
| Ibandronate sodium | Boniva/Bonviva | Genentech/Roche (Roche Korea) | 150 mg (PO) | Osteoporosis | |
| 3 mg (IV) | Osteoporosis | ||||
| Bonviva plus | (Alvogen Korea) | 150 mg (PO) | Osteoporosis | ||
| Risedronate sodium | Actonel | Warner Chilcott (Handok) | 5, 35, 75, 150 mg (PO) | Osteoporosis, Paget's disease | |
| Clodronate disodium | Bonefos | Bayer | 400, 800 mg (PO) | Osteoporosis, hypercalcemia and osteolysis due to malignancy | |
| Paget's disease, hypercalcemia due to metastatic bone disease, multiple myeloma | |||||
| Tiludronate disodium | Skelid | Sanofi-Aventis | 240 mg (PO) | Paget's disease | |
| Pamidronate disodium | Aredia | Novatis Pharmaceuticals (Novartis Korea) | 30, 60, 90 mg (IV) | Hypercalcemia with malignancy, bone metastases, Paget's disease | |
| Denosumab | Prolia | Amgen (Amgen Korea) | 60 mg (SC) | Osteoporosis | |
| Xgeva | 120 mg (SC) | Skeletal related event with bone metastases | |||
IV, intravenous injection; PO, per os; SC, subcutaneous injection.
In 2011, denosumab (Dmab), a high-affinity and highly-specific monoclonal antibody for human receptor activator of nuclear factor-kB ligand (RANKL), was Food and Drug Administration-approved for the similar clinical use as an ARD [13]. Dmab is the newest ARD, with a novel mechanism of action. While BPs mainly affect osteoclast function through inhibition of differentiation and maturation and induction of apoptosis [14], Dmab inhibits osteoclastic formation, function, and survival [15,16]. Furthermore, Dmab does not become embedded within bone tissue and has a short half-life of 12.5 days when compared with BPs, which have a half-life of 10–12 years [17].
A different ARD, odanacatib (ODN), an orally active, potent, and selective cathepsin K inhibitor was developed for the treatment of postmenopausal osteoporosis. ODN is known to reduce bone resorption by selectively inhibiting cathepsin K-induced matrix proteolysis without affecting other osteoclastic functions or osteoclast viability [18]. However, its use has been discontinued since 2016 because of an increased risk for cardiovascular events [19].
2. ARONJ
In 2003, ONJ was reported as a major side effect of BP treatment [2]. ONJ was also reported as one of the adverse effects of Dmab use [20]. Therefore, ARONJ has been suggested as a comprehensive term encompassing both BRONJ and Dmab-related ONJ (DRONJ) [5]. Other antiresorptive agents including cathepsin K inhibitors and antiangiogenic inhibitors could also be proven to be associated with ONJ. Therefore, the American Association of Oral and Maxillofacial Surgeons (AAOMS) has proposed the term “medication-related osteonecrosis of the jaw” involving antiangiogenic therapies as relating factors, although global consensus has not yet been established [3,21]. In this review, the term ‘ARONJ’ will be used in order to focus on ARDs.
3. Incidence of ARONJ
The incidence of ONJ is related to dose and duration of exposure to ARD. While the incidence of ONJ in patients with osteoporosis is very low, i.e., from 0.001% to 0.01%, the incidence in the oncology patient population is much higher (0.5% to 4.6%) [22,23]. According to Khan et al. [24], greater than 90% of cases of ARONJ occur in cancer patients receiving high intravenous (IV) doses of BPs (i.e., 3 mg every 3–4 weeks) or subcutaneous Dmab (i.e., 120 mg every 4 weeks). Considering that the doses used for cancer-related cases are 12–25 times higher than those used for treating osteoporosis, it is not surprising that ONJ is reported more frequently in cancer patients than in patients with osteoporosis [25,26,27,28]. Moreover, several clinical studies have reported that the incidences of ONJ in cancer patients in year 1, 2, and 3 were 0.5%–1.1%, 1.2%–3.7%, and 1.4%–4.6%, respectively, highlighting the increased risk for ONJ associated with more prolonged treatment [23,29,30].
4. Diagnosis and clinical manifestations of ARONJ
Patients are considered to have ARONJ if all the following characteristics are present [3]: 1) Current or previous treatment with ARDs, 2) Exposed bone or bone that can be probed through an intraoral or extraoral sinus tract in the maxillofacial region that has persisted for longer than 8 weeks, 3) No history of radiation therapy to the jaws or obvious metastatic disease to the jaw.
Most clinical presentation of ARONJ includes inflammation and an unhealed wound. According to the clinical symptoms and radiographic findings, ARONJ has been categorized into four stages [21]. Stages 1–3 include exposed/necrotic bone, while stage 0 includes patients with no clinical evidence of necrotic bone but with nonspecific clinical findings, radiographic changes, and symptoms. When the stage 0 category was added in 2009, the risk of a patient in this category was unknown. However, Fedele et al. [31] reported that this stage accounted for 25%–30% of ONJ, and half of the non-exposed BRONJ subsequently progressed to frank bone exposed ONJ. Regardless of the risk for over-diagnosing ONJ, stage 0 should still be diagnosed and treated as pre-ONJ, and dentists have a pivotal role in the early diagnosis of ONJ. Bone pain and radiographic features of osteosclerosis may present as stage 0 ONJ [22]. In such circumstances, it is necessary to exclude other possibilities that can cause odontalgia and implement a careful radiographic evaluation.
5. Potential risk factors for ARONJ
Several known risk factors are associated with ARONJ development. Among them, invasive dental treatments such as tooth extraction, dental implant, or apical/periodontal surgery are definitive local risk factors [3]. Tooth extraction is considered as the intervention most responsible for ARONJ, ranging from 69% to 86% of cases [32,33]. A retrospective study from Australia reported an 8-fold increased risk for both IV and oral administration of ARDs [34]. In a longitudinal cohort study with cancer patients exposed to IV BPs, tooth extraction was associated with a maximum 33-fold increased risk for ONJ [28].
Another risk factor is a concomitant local infection such as periodontal/periapical inflammation. Saad et al. [27] analyzed oncology patients with ONJ and reported that a tooth extraction is a precipitant in approximately two-thirds of the patients, while a coincident oral infection is found in about half of the patients. Several recent studies have reported that a local infection is the main trigger for ONJ development [35,36,37,38,39,40]. Otto et al. [35] investigated the outcome of tooth extractions in patients receiving BP therapy. They reported that many cases already had osteomyelitis or osteonecrotic structural bone changes at the time of tooth extraction, a very important consideration when understanding the pathogenesis of ONJ. Given the reason for tooth extraction, preexisting infection/inflammation around a tooth could cause these bony changes even before tooth extraction. In addition, the use of antiangiogenic agents and tyrosine kinase inhibitors, which are essentially administered as adjuvants in cancer patients, was associated with an increased risk for ONJ [22,41].
Suggested dental care to lower the risk of developing ARONJ
All patients taking ARDs do not have ONJ. Even though surgical intervention has been shown to be a local risk factor for ONJ development, some studies have shown that the incidence of ARONJ can be reduced with preventive dental interventions [5,42,43]. Karna et al. [44] assess the effectiveness of dental interventions in preventing or reducing the incidence of ARONJ in cancer patients taking ARDs. They showed a 77.3% reduction in the incidence of ARONJ in the dental intervention group when compared with the group without any dental intervention. Preventive dental intervention includes any dental management, i.e., completion of dental treatment before commencing ARDs, use of antibiotics before and after a surgical procedure, and maintenance of good oral health [44,45,46,47,48]. In this respect, dentists play a critical role in optimizing the prevention and reduction of ARONJ development.
Many studies have proposed practical guidelines for dental care for preventing ONJ in patients taking ARDs [3,5,21,35,49]. Generally, it is important to educate patients on the importance of maintaining oral hygiene. Furthermore, the causes of infection such as caries, dental plaque, periodontitis, and apical periodontitis need to be treated with conservative procedures. Lastly, if possible, invasive dental procedures should be avoided. To provide proper dental care, dentists need to evaluate the medical history specifically and assess the risk of ARONJ during an examination. The dentist should confirm whether ARD treatment is scheduled or has already started. If treatment has started, the dose of BPs or Dmab the patient is receiving, the treatment duration, and whether any other medication likely to increase the risk of ARONJ is being used should be determined. Based on this information, patients can be categorized as being at low or high risk for developing ARONJ (Table 2) [23]. Patients who have received a low dose of an ARD for less than 4 years with no additional risk factors are regarded to have low risk. Otherwise, all other patients taking an ARD are considered to be at high risk [3,50,51,52].
Table 2. Evaluation factors for the patients at low or high risk of ARONJ.
| ARONJ risk | ARD dose | Treatment duration | Additional risk factors‡ | |||
|---|---|---|---|---|---|---|
| Low dose* | High dose† | ≤ 4 years | > 4 years | None | At least one | |
| At low risk | ○ | - | ○ | - | ○ | - |
| At high risk | ○ | - | ○ | - | - | ○ |
| ○ | - | - | ○ | - | - | |
| - | ○ | - | - | - | - | |
ARONJ, antiresorptive agent-related osteonecrosis of the jaw; ARD, antiresorptive drug; BP, bisphosphonate; Dmab, denosumab; IV, intravenous injection.
*Low dose: low dose of BPs (oral uptake), Dmab (60 mg every 6 months); †High dose: high dose of BPs (IV injection), Dmab (120 mg every 4 weeks); ‡Additional risk factors: Prior use of BPs or Dmab, Use of corticosteroids, chemotherapy, or angiogenesis inhibitors, radiotherapy to head and neck, poor oral hygiene, periodontitis, ill-fitting dentures, smoking, comorbidities (e.g. cancer, hematological disease, immunological disorders, diabetes mellitus, anemia).
1. Patients at low risk for ARONJ of the Jaw
1) Prior to ARD treatment
Taking into account the European Society for Medical Oncology and the British National Osteoporosis Guidance Group, there is a consensus across the guidelines that, in order to prevent the occurrence of ONJ, a comprehensive oral evaluation is recommended prior to initiating ARDs [3,23,53,54]. Especially prior to commencing IV BPs or Dmab in cancer patients, it is necessary to instruct screening visits. In addition, invasive dental procedures and subsequent healing should be completed if the clinical condition permits. However, for patients at low risk for developing ONJ, a routine screening visit is not required [23]. The usual recommendations on preventive dental care, such as periodic recall check-ups, effective plaque control, dietary advice, and antibacterial and/or fluoride mouthwash, applicable to the general population are enough for such low-risk individuals. If a low-risk patient has not complied with these recommendations, a preventive dental visit should be advised.
2) Under ARD treatment
For patients at low risk of developing ONJ, no alteration or delay in the planned dental treatment is necessary. All conservative treatments, including restorative treatment, nonsurgical endodontic treatment, and prosthodontic/orthodontic therapy, are safe. Only a few cases of ONJ have been reported after nonsurgical endodontic procedures. However, when analyzed in detail, these cases are controversial because a spontaneous osteonecrotic process may be present before root canal therapy and may possibly cause painful symptoms that could be misdiagnosed as apical periodontitis together with non-specific radiographic feature [55]. With invasive dental procedures, elective dentoalveolar surgery is not contraindicated. Simple extractions and surgeries that do not involve osteotomy can be carried out [23]. If a dental implant needs to be placed, informed consent should be provided for the risks for possible long-term implant failure and the low risk for developing ONJ [56]. To minimize the risk for ONJ, clinicians should recommend the use of an antimicrobial mouthwash and systemic antibiotics before/after the procedure [32,35].
2. Patients at high risk for ARONJ
1) Prior to ARD treatment
Prophylactic dental treatment should be carried on all high-risk patients. With this recognition, the American Society of Clinical Oncology and Cancer Care Ontario group made the following recommendation: “A dental assessment is recommended, where feasible, before the commencement of BPs, and any pending dental or oral health problems should be dealt with before starting treatment” [57]. The evaluation and management of patients who are to receive ARD treatment are similar to those scheduled to initiate head and neck radiation therapy [3]. This evaluation should include a thorough oral examination and a radiographic evaluation to identify acute infections and potential infections that could be exacerbated [3]. Treatment should include conservative endodontic and prosthodontic therapies with good prognosis and periodontal treatment for teeth with good dental hygiene [3,23]. However, for teeth with poor hygiene or poor prognosis, extraction is preferred. All necessary oral surgery should be completed before starting ARDs. Ideally, the ARD treatment should be initiated after mucosa epithelialization, and adequate bone remodeling have occurred, which usually takes 2 to 4 weeks after dental treatment [21,22,23]. It is recommended to maintain good oral hygiene and ensure optimal periodontal health and well-fitted dentures, not needing further dental procedures.
2) Under ARD treatment
For patients on ARD treatment, dentists need to consider that these patients are potentially at increased risk for developing ONJ even in the absence of any signs and symptoms. Therefore, clinical and radiographic evaluations should be carried out. Periapical radiographs of all teeth and panoramic radiographs are recommended to identify potential infection/inflammation [21]. For patients suspected of having ONJ, conventional computed tomography (CT) and cone-beam CT help detect early changes in the cortical and trabecular architecture of the jaw as well as involved teeth [58,59].
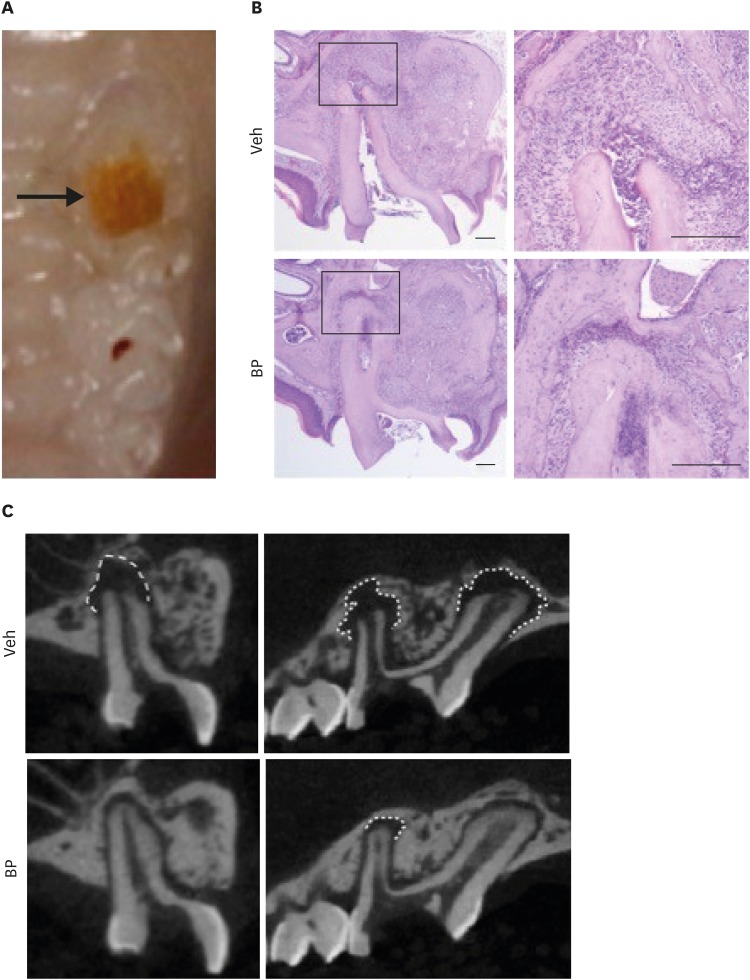
It is recommended to evaluate and interpret radiographs taken in patients using ARDs with caution. The radiographic changes seen in mice models taking BPs have been evaluated in some studies [39,60]. Kang et al. [60] demonstrated that radiographic features in these mice showed thickening of the lamina dura, periosteal bone deposition, and increased trabecular density despite induced periapical inflammation. Moreover, no periapical radiolucency was detected despite prominent periapical inflammation, as confirmed by histologic analysis, indicating that periapical radiolucency may not always be a good indicator for root canal therapy in BP users (Figure 1) [39]. This is the reason why dental treatment should be planned more aggressively in patients taking ARDs.
Figure 1. Bisphosphonates (BPs) prevent bone resorption at the apex of the pulp-exposed tooth despite the presence of inflammatory cells. Mice were intravenously administered with BPs twice a week throughout the study. One week after the initial administration, pulp was exposed and left open for 3 weeks (A), and maxillae were harvested. (B) Histologic examination revealed that there is intense infiltration of inflammatory cells at the apex in both Veh- and BP-treated mice. (C) Micro-computed tomography (µCT) scans of a pulp-exposed tooth showed marked bone resorption around the apex of the tooth in Veh-treated mice. However, BP-treated mice did not show evident bone resorption in µCT scan. Images modified from Song et al. [39].
Generally, conservative dental treatment such as removal of dental caries and nonsurgical endodontic treatment can be performed. Considering that nonsurgical endodontic treatment aims to control and prevent the spread of infection to the periapical tissue, it should be performed actively and could be recommended as an alternative to extraction in order to reduce the risk of developing ONJ. Some authors reported the association of nonsurgical endodontic treatment with ONJ development. They proposed that soft tissue damage caused by rubber dam clamp and extrusion of microorganisms during root canal instrumentation could be a local factor for initiating ONJ development [61,62,63]. More evidence is required to support this; however, it is recommended to reduce the likelihood of ONJ. Some recommendations during nonsurgical endodontic treatment include [63,64]: 1) Use of an antimicrobial mouthwash is recommended to minimize the possibility of bacteremia, 2) Avoid using anesthetic agents containing vasoconstrictors in order to reduce the risk of inadequate vascularization [55], 3) To avoid any damage to the gingival tissues, using wedges may be considered as an alternative to rubber dam clamp, 4) To reduce the possibility of apical extrusion during instrumentation, apical patency could be avoided, 5) The use of systemic antibiotics before/after the procedure should be considered. Denture wearing is also acceptable; however, it should be examined for excessive pressure or friction and be given a soft reline if needed [65].
Invasive dental procedures should be avoided in high-risk patients. As reported in several studies, tooth extraction is a major local factor contributing to the increasing incidence of ONJ in patients taking ARDs [28,33,34,35,66]. Therefore, it is recommended to treat severely damaged teeth using a conservative endodontic approach with remaining tooth structure instead of extraction [67]. Root canal treatment and decoronation are better than a tooth extraction. Similarly, teeth that demonstrate 1 or 2 mobility should be splinted rather than extracted [65]. The use of orthodontic elastics has also been proposed to promote atraumatic extraction [67].
According to Otto et al. [35], prevailing infectious conditions, not tooth extraction, might be a key risk factor for the development of ONJ. Therefore, tooth extraction can be performed in a safe and predictable way, even in high-risk patients, when performed according to established guidelines [35]. Their findings are consistent with previous findings by Saia et al. [68], who showed that prevailing infectious conditions might be a key risk factor in the development of ONJ. Considering that the main reason for tooth extraction is the eradication of a local infection that cannot be cured by conservative measures, surgical procedures should not necessarily be avoided in patients receiving ARDs [35]. Instead, the use of antimicrobial mouthwash and systemic antibiotics before/after surgery should be implemented under all efforts.
3) Considerations to lower ONJ incidence before surgical procedures
Even though all attempts should be made to avoid surgical procedures, however, surgery is sometimes inevitable. Several considerations can lower the incidence of ONJ. This includes the use of serum C-terminal telopeptide (sCTX) levels as a predictor, drug holiday/discontinuation, and extensive infection control prior to a surgical procedure.
First, the serum sCTX level, a marker of bone resorption, can be considered as a predictor of ONJ development. It was used to assess osteoclast and osteoblast activities. Thus some investigators suggested that it could be used as a marker for ONJ development. For example, Marx and their colleagues suggested that if the patient has a fasting sCTX value of at least 150 pg/mL, the clinician can schedule the surgical procedure because the patient has a minimal risk; if the value is equal to or less than 100 pg/mL, the clinician should consider the patient to have a high risk of developing ONJ [50]. Recently, however, many studies reported that there is no significant relation between sCTX and the development of ONJ [69,70,71,72]. Many variables affect sCTX measurement, and these include age, alcohol habit, smoking, ovulation, sex, exercise, circadian rhythms, drugs such as corticosteroids, diseases such as diabetes, and laboratory testing variability [69]. Low sCTX levels simply imply a reflection of the pharmacological effects of antiresorptive therapy and cannot be used as a predictor for the risk of ONJ.
Drug holiday/discontinuation could be considered before invasive dental treatment to prevent the development of ONJ. However, there is considerable controversy on the use of BPs. The advisory board of the US FDA, AAOMS, and other groups including the Korean Society for Bone and Mineral Research and the Korean Association of Oral and Maxillofacial Surgeons suggested drug discontinuation (drug holiday) for at least 2 months before any surgical procedure, for patients who have taken an oral BPs and are at high risk for developing ONJ, as long as systemic conditions permit [3,73]. On the contrary, a recent study from Japan found that drug holidays before tooth extraction did not reduce the risk of ONJ in patients receiving oral BPs [74]. BPs have long-term skeletal retention, and so cessation for weeks or months may not impact bone remodeling significantly. Meanwhile, Dmab is considered to act reversibly. A recent preclinical study reported that ONJ spontaneously resolved after discontinuation of (OPG)-Fc use, a molecule that has the same RANKL inhibitory action similar to Dmab [75]. They suggested that for patients receiving high-dose ARDs for the management of cancer, Dmab discontinuation would offer a faster and more complete resolution of ONJ when compared with BPs. Another case report also noted that the healing of DRONJ occurred in colon cancer patients with bone metastases after discontinuation of Dmab [76]. For patients taking Dmab, drug holiday could be an option before a surgical procedure is considered.
Several recent studies have reported that an infection is an essential event for the development of ONJ, and extensive infection control before any invasive dental treatment reduces the risk of ONJ [35,77,78]. Kim et al. [40] provided experimental evidence that a pre-existing pathologic periapical/periodontal inflammatory condition exacerbates ARONJ development after tooth extraction in mice [39]. Using a periodontal inflammation mouse model, they also showed that the removal of pre-existing inflammatory conditions before tooth extraction ameliorates the ONJ-like lesion. Therefore, it is suggested that any kind of inflammation/infection should be controlled before performing a tooth extraction in individuals taking ARDs to reduce the risk of developing ONJ. Therefore, even though a tooth extraction may have been scheduled for any patient taking ARDs, it is recommended to control any pre-existing inflammation by performing proactive treatments such as root canal therapy before performing tooth extraction [39].
4) After dental treatment
After an invasive dental procedure, temporary discontinuation of ARDs may be considered as a means to promote the healing of surgical wounds. Temporal discontinuation of ARDs is not associated with ONJ but wound healing, especially epithelialization [79]. BPs may increase the risk of local infection and, possibly, contribute to impaired healing of the oral mucosa [80,81,82,83,84,85]. It could also induce impaired osseous wound healing of the jaw and the maintenance of inflammation in connective tissues [84]. Therefore, if systemic conditions permit, resumption of antiresorptive treatment is recommended approximately 2 months after the invasive dental procedure. However, if systemic conditions get worse during drug discontinuation, the earliest time to resume ARD treatment should be 2 weeks after an invasive dental treatment when the epithelization of the surgical site is complete [21].
Relating issues with taking ARDs
1. External cervical root resorption (ECR)
The etiology and pathogenesis of ECR are not well understood, and several predisposing factors have been reported to potentially contribute to the initiation of ECR; trauma, orthodontic therapy, benign and malignant neoplasms, chronic periodontal or periapical infections, and Paget's disease of the bone. A few case reports suggested a possible relationship between the use of BPs and ECR [86,87]. BPs are believed to suppress osteoclastic activity. Therefore, they are thought to prevent the initiation or progression of ECR [86]. However, amino-containing BPs such as alendronic acid have proinflammatory properties that can cause an acute-phase response, which could be associated with the initiation of ECR [88,89,90]. Recently, tooth resorption has been reported in 11 cases treated with Dmab [86,91]. They questioned whether the administration and subsequent discontinuation of Dmab were related to the initiation and subsequent extensive and rapid progression of generalized ECR. Upon discontinuation of Dmab, bone turnover and osteoclast activity transiently increased to levels above the starting range before eventually returning to pretreatment levels [92]. This potential osteoclastic rebound effect could contribute to rapid ECR progression after the discontinuation of Dmab [91]. Even though more evidence is required, a possible relationship between ARD therapy and ECR has been uncovered. Thorough dental assessments before, during, and after ARD therapy should be performed, and detection of ECR lesions at the early stages is recommended to facilitate their conservative management [87].
2. Clinical outcome of root canal treatment
There is a concern about the healing outcome of root canal treatment in patients taking ARDs. Hsiao et al. [93] found that the healing rate of periapical lesions in patients taking oral BPs was 73.5%, which was not significantly different from patients without taking oral BPs (81.6%). Meanwhile, a recent study involving patients taking IV BPs revealed a strong relationship between the duration of BPs treatment and the success of root canal treatment [94]. They showed that the success rate increased in patients with shorter BP treatment durations (i.e., less than 1 year). The main limitation of these studies is the small sample size; therefore, further clinical studies are required to clarify the relationship between endodontic treatment and BPs or Dmab use.
CONCLUSIONS
More than 24 million prescriptions for BP were issued in the United States, and more than 190 million internationally. Recently developed Dmab has also seen increased use. The World Health Organization predicts that people older than 65 years will comprise 20% of the world population by 2030 [95]. Considering that osteoporosis is increasingly prevalent among the aging and in those with breast or prostate cancer, the most common cancers in women and men, respectively, the benefit provided by ARDs cannot be ignored and their use outweighs the risk for developing ONJ.
ARONJ is rare but potentially intractable; therefore, the importance of preventing ONJ development should be well-known to physicians and dentists. Dentists have a critical role in preventing and reducing the incidence of ONJ. Fortunately, there is a consensus to avoid surgical procedures to prevent ONJ development in patients taking ARDs. Furthermore, to provide proper dental care, a good understanding of ARDs treatment and ARONJ is important. A poor understanding of ARDs therapy could lead to hesitation or even refusal on the part of dentists to provide essential dental treatment for maintaining quality of life in patients with skeletal-related events or cancers. Dentists should be aware that they could play an important role in preventing ARONJ as well as help patients taking ARDs to maintain appropriate oral health.
Footnotes
Funding: The present research was supported by the research fund of Dankook University in 2018
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
- 1.Ruggiero SL, Drew SJ. Osteonecrosis of the jaws and bisphosphonate therapy. J Dent Res. 2007;86:1013–1021. doi: 10.1177/154405910708601101. [DOI] [PubMed] [Google Scholar]
- 2.Marx RE. Pamidronate (Aredia) and zoledronate (Zometa) induced avascular necrosis of the jaws: a growing epidemic. J Oral Maxillofac Surg. 2003;61:1115–1117. doi: 10.1016/s0278-2391(03)00720-1. [DOI] [PubMed] [Google Scholar]
- 3.Ruggiero SL, Dodson TB, Fantasia J, Goodday R, Aghaloo T, Mehrotra B, O'Ryan F American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on medication-related osteonecrosis of the jaw--2014 update. J Oral Maxillofac Surg. 2014;72:1938–1956. doi: 10.1016/j.joms.2014.04.031. [DOI] [PubMed] [Google Scholar]
- 4.Ruggiero SL, Dodson TB, Assael LA, Landesberg R, Marx RE, Mehrotra B American Association of Oral and Maxillofacial Surgeons. American Association of Oral and Maxillofacial Surgeons position paper on bisphosphonate-related osteonecrosis of the jaws--2009 update. J Oral Maxillofac Surg. 2009;67:2–12. doi: 10.1016/j.joms.2009.01.009. [DOI] [PubMed] [Google Scholar]
- 5.Hellstein JW, Adler RA, Edwards B, Jacobsen PL, Kalmar JR, Koka S, Migliorati CA, Ristic H American Dental Association Council on Scientific Affairs Expert Panel on Antiresorptive Agents. Managing the care of patients receiving antiresorptive therapy for prevention and treatment of osteoporosis: executive summary of recommendations from the American Dental Association Council on Scientific Affairs. J Am Dent Assoc. 2011;142:1243–1251. doi: 10.14219/jada.archive.2011.0108. [DOI] [PubMed] [Google Scholar]
- 6.Fleisch H. Development of bisphosphonates. Breast Cancer Res. 2002;4:30–34. doi: 10.1186/bcr414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Letocha AD, Cintas HL, Troendle JF, Reynolds JC, Cann CE, Chernoff EJ, Hill SC, Gerber LH, Marini JC. Controlled trial of pamidronate in children with types III and IV osteogenesis imperfecta confirms vertebral gains but not short-term functional improvement. J Bone Miner Res. 2005;20:977–986. doi: 10.1359/JBMR.050109. [DOI] [PubMed] [Google Scholar]
- 8.Delmas PD. The use of bisphosphonates in the treatment of osteoporosis. Curr Opin Rheumatol. 2005;17:462–466. doi: 10.1097/01.bor.0000163448.51661.87. [DOI] [PubMed] [Google Scholar]
- 9.Brufsky AM. Zoledronic acid for cancer therapy--induced and postmenopausal bone loss. Expert Opin Pharmacother. 2008;9:1013–1028. doi: 10.1517/14656566.9.6.1013. [DOI] [PubMed] [Google Scholar]
- 10.Berenson JR, Hillner BE, Kyle RA, Anderson K, Lipton A, Yee GC, Biermann JS American Society of Clinical Oncology Bisphosphonates Expert Panel. American Society of Clinical Oncology clinical practice guidelines: the role of bisphosphonates in multiple myeloma. J Clin Oncol. 2002;20:3719–3736. doi: 10.1200/JCO.2002.06.037. [DOI] [PubMed] [Google Scholar]
- 11.Rosen LS, Gordon D, Tchekmedyian NS, Yanagihara R, Hirsh V, Krzakowski M, Pawlicki M, De Souza P, Zheng M, Urbanowitz G, Reitsma D, Seaman J Zoledronic Acid Lung Cancer and Other Solid Tumors Study Group. Long-term efficacy and safety of zoledronic acid in the treatment of skeletal metastases in patients with nonsmall cell lung carcinoma and other solid tumors: a randomized, Phase III, double-blind, placebo-controlled trial. Cancer. 2004;100:2613–2621. doi: 10.1002/cncr.20308. [DOI] [PubMed] [Google Scholar]
- 12.Russell RG, Rogers MJ. Bisphosphonates: from the laboratory to the clinic and back again. Bone. 1999;25:97–106. doi: 10.1016/s8756-3282(99)00116-7. [DOI] [PubMed] [Google Scholar]
- 13.Bogado CE, Zanchetta MB, Boailchuk JA, Massari FE, Zanchetta JR. Denosumab: what's new? Curr Osteoporos Rep. 2011;9:12–19. doi: 10.1007/s11914-010-0040-1. [DOI] [PubMed] [Google Scholar]
- 14.Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev. 1998;19:80–100. doi: 10.1210/edrv.19.1.0325. [DOI] [PubMed] [Google Scholar]
- 15.Romas E. Clinical applications of RANK-ligand inhibition. Intern Med J. 2009;39:110–116. doi: 10.1111/j.1445-5994.2008.01732.x. [DOI] [PubMed] [Google Scholar]
- 16.Geusens P. Emerging treatments for postmenopausal osteoporosis - focus on denosumab. Clin Interv Aging. 2009;4:241–250. doi: 10.2147/cia.s3333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Uyanne J, Calhoun CC, Le AD. Antiresorptive drug-related osteonecrosis of the jaw. Dent Clin North Am. 2014;58:369–384. doi: 10.1016/j.cden.2013.12.006. [DOI] [PubMed] [Google Scholar]
- 18.Hao L, Chen W, McConnell M, Zhu Z, Li S, Reddy M, Eleazer PD, Wang M, Li YP. A small molecule, odanacatib, inhibits inflammation and bone loss caused by endodontic disease. Infect Immun. 2015;83:1235–1245. doi: 10.1128/IAI.01713-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mullard A. Merck &Co. drops osteoporosis drug odanacatib. Nat Rev Drug Discov. 2016;15:669. doi: 10.1038/nrd.2016.207. [DOI] [PubMed] [Google Scholar]
- 20.Boquete-Castro A, Gómez-Moreno G, Calvo-Guirado JL, Aguilar-Salvatierra A, Delgado-Ruiz RA. Denosumab and osteonecrosis of the jaw. A systematic analysis of events reported in clinical trials. Clin Oral Implants Res. 2016;27:367–375. doi: 10.1111/clr.12556. [DOI] [PubMed] [Google Scholar]
- 21.Yoneda T, Hagino H, Sugimoto T, Ohta H, Takahashi S, Soen S, Taguchi A, Nagata T, Urade M, Shibahara T, Toyosawa S Japanese Allied Committee on Osteonecrosis of the Jaw. Antiresorptive agent-related osteonecrosis of the jaw: position paper 2017 of the Japanese Allied Committee on Osteonecrosis of the Jaw. J Bone Miner Metab. 2017;35:6–19. doi: 10.1007/s00774-016-0810-7. [DOI] [PubMed] [Google Scholar]
- 22.Khan AA, Morrison A, Kendler DL, Rizzoli R, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB, Brandi ML, Peters E, Guise T, Eastell R, Cheung AM, Morin SN, Masri B, Cooper C, Morgan SL, Obermayer-Pietsch B, Langdahl BL, Dabagh RA, Davison KS, Sándor GK, Josse RG, Bhandari M, El Rabbany M, Pierroz DD, Sulimani R, Saunders DP, Brown JP, Compston J International Task Force on Osteonecrosis of the Jaw. Case-based review of osteonecrosis of the jaw (ONJ) and application of the international recommendations for management from the International Task Force on ONJ. J Clin Densitom. 2017;20:8–24. doi: 10.1016/j.jocd.2016.09.005. [DOI] [PubMed] [Google Scholar]
- 23.Nicolatou-Galitis O, Schiødt M, Mendes RA, Ripamonti C, Hope S, Drudge-Coates L, Niepel D, Van den Wyngaert T. Medication-related osteonecrosis of the jaw: definition and best practice for prevention, diagnosis, and treatment. Oral Surg Oral Med Oral Pathol Oral Radiol. 2019;127:117–135. doi: 10.1016/j.oooo.2018.09.008. [DOI] [PubMed] [Google Scholar]
- 24.Khan A, Morrison A, Cheung A, Hashem W, Compston J. Osteonecrosis of the jaw (ONJ): diagnosis and management in 2015. Osteoporos Int. 2016;27:853–859. doi: 10.1007/s00198-015-3335-3. [DOI] [PubMed] [Google Scholar]
- 25.Durie BG, Katz M, Crowley J. Osteonecrosis of the jaw and bisphosphonates. N Engl J Med. 2005;353:99–102. doi: 10.1056/NEJM200507073530120. [DOI] [PubMed] [Google Scholar]
- 26.Jadu F, Lee L, Pharoah M, Reece D, Wang L. A retrospective study assessing the incidence, risk factors and comorbidities of pamidronate-related necrosis of the jaws in multiple myeloma patients. Ann Oncol. 2007;18:2015–2019. doi: 10.1093/annonc/mdm370. [DOI] [PubMed] [Google Scholar]
- 27.Saad F, Brown JE, Van Poznak C, Ibrahim T, Stemmer SM, Stopeck AT, Diel IJ, Takahashi S, Shore N, Henry DH, Barrios CH, Facon T, Senecal F, Fizazi K, Zhou L, Daniels A, Carrière P, Dansey R. Incidence, risk factors, and outcomes of osteonecrosis of the jaw: integrated analysis from three blinded active-controlled phase III trials in cancer patients with bone metastases. Ann Oncol. 2012;23:1341–1347. doi: 10.1093/annonc/mdr435. [DOI] [PubMed] [Google Scholar]
- 28.Vahtsevanos K, Kyrgidis A, Verrou E, Katodritou E, Triaridis S, Andreadis CG, Boukovinas I, Koloutsos GE, Teleioudis Z, Kitikidou K, Paraskevopoulos P, Zervas K, Antoniades K. Longitudinal cohort study of risk factors in cancer patients of bisphosphonate-related osteonecrosis of the jaw. J Clin Oncol. 2009;27:5356–5362. doi: 10.1200/JCO.2009.21.9584. [DOI] [PubMed] [Google Scholar]
- 29.Stopeck AT, Lipton A, Body JJ, Steger GG, Tonkin K, de Boer RH, Lichinitser M, Fujiwara Y, Yardley DA, Viniegra M, Fan M, Jiang Q, Dansey R, Jun S, Braun A. Denosumab compared with zoledronic acid for the treatment of bone metastases in patients with advanced breast cancer: a randomized, double-blind study. J Clin Oncol. 2010;28:5132–5139. doi: 10.1200/JCO.2010.29.7101. [DOI] [PubMed] [Google Scholar]
- 30.Stopeck AT, Fizazi K, Body JJ, Brown JE, Carducci M, Diel I, Fujiwara Y, Martín M, Paterson A, Tonkin K, Shore N, Sieber P, Kueppers F, Karsh L, Yardley D, Wang H, Maniar T, Arellano J, Braun A. Safety of long-term denosumab therapy: results from the open label extension phase of two phase 3 studies in patients with metastatic breast and prostate cancer. Support Care Cancer. 2016;24:447–455. doi: 10.1007/s00520-015-2904-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Fedele S, Porter SR, D'Aiuto F, Aljohani S, Vescovi P, Manfredi M, Arduino PG, Broccoletti R, Musciotto A, Di Fede O, Lazarovici TS, Campisi G, Yarom N. Nonexposed variant of bisphosphonate-associated osteonecrosis of the jaw: a case series. Am J Med. 2010;123:1060–1064. doi: 10.1016/j.amjmed.2010.04.033. [DOI] [PubMed] [Google Scholar]
- 32.Lodi G, Sardella A, Salis A, Demarosi F, Tarozzi M, Carrassi A. Tooth extraction in patients taking intravenous bisphosphonates: a preventive protocol and case series. J Oral Maxillofac Surg. 2010;68:107–110. doi: 10.1016/j.joms.2009.07.068. [DOI] [PubMed] [Google Scholar]
- 33.Mozzati M, Arata V, Gallesio G. Tooth extraction in patients on zoledronic acid therapy. Oral Oncol. 2012;48:817–821. doi: 10.1016/j.oraloncology.2012.03.009. [DOI] [PubMed] [Google Scholar]
- 34.Mavrokokki T, Cheng A, Stein B, Goss A. Nature and frequency of bisphosphonate-associated osteonecrosis of the jaws in Australia. J Oral Maxillofac Surg. 2007;65:415–423. doi: 10.1016/j.joms.2006.10.061. [DOI] [PubMed] [Google Scholar]
- 35.Otto S, Tröltzsch M, Jambrovic V, Panya S, Probst F, Ristow O, Ehrenfeld M, Pautke C. Tooth extraction in patients receiving oral or intravenous bisphosphonate administration: a trigger for BRONJ development? J Craniomaxillofac Surg. 2015;43:847–854. doi: 10.1016/j.jcms.2015.03.039. [DOI] [PubMed] [Google Scholar]
- 36.Otto S, Hafner S, Mast G, Tischer T, Volkmer E, Schieker M, Stürzenbaum SR, von Tresckow E, Kolk A, Ehrenfeld M, Pautke C. Bisphosphonate-related osteonecrosis of the jaw: is pH the missing part in the pathogenesis puzzle? J Oral Maxillofac Surg. 2010;68:1158–1161. doi: 10.1016/j.joms.2009.07.079. [DOI] [PubMed] [Google Scholar]
- 37.Otto S, Pautke C, Opelz C, Westphal I, Drosse I, Schwager J, Bauss F, Ehrenfeld M, Schieker M. Osteonecrosis of the jaw: effect of bisphosphonate type, local concentration, and acidic milieu on the pathomechanism. J Oral Maxillofac Surg. 2010;68:2837–2845. doi: 10.1016/j.joms.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 38.Aguirre JI, Akhter MP, Kimmel DB, Pingel JE, Williams A, Jorgensen M, Kesavalu L, Wronski TJ. Oncologic doses of zoledronic acid induce osteonecrosis of the jaw-like lesions in rice rats (Oryzomys palustris) with periodontitis. J Bone Miner Res. 2012;27:2130–2143. doi: 10.1002/jbmr.1669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Song M, Alshaikh A, Kim T, Kim S, Dang M, Mehrazarin S, Shin KH, Kang M, Park NH, Kim RH. Preexisting periapical inflammatory condition exacerbates tooth extraction–induced bisphosphonate-related osteonecrosis of the jaw lesions in mice. J Endod. 2016;42:1641–1646. doi: 10.1016/j.joen.2016.07.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kim T, Kim S, Song M, Lee C, Yagita H, Williams DW, Sung EC, Hong C, Shin KH, Kang MK, Park NH, Kim RH. Removal of pre-existing periodontal inflammatory condition before tooth extraction ameliorates medication-related osteonecrosis of the jaw-like lesion in mice. Am J Pathol. 2018;188:2318–2327. doi: 10.1016/j.ajpath.2018.06.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ramírez L, López-Pintor RM, Casañas E, Arriba L, Hernández G. New non-bisphosphonate drugs that produce osteonecrosis of the jaws. Oral Health Prev Dent. 2015;13:385–393. doi: 10.3290/j.ohpd.a34055. [DOI] [PubMed] [Google Scholar]
- 42.Khan AA, Morrison A, Hanley DA, Felsenberg D, McCauley LK, O'Ryan F, Reid IR, Ruggiero SL, Taguchi A, Tetradis S, Watts NB, Brandi ML, Peters E, Guise T, Eastell R, Cheung AM, Morin SN, Masri B, Cooper C, Morgan SL, Obermayer-Pietsch B, Langdahl BL, Al Dabagh R, Davison KS, Kendler DL, Sándor GK, Josse RG, Bhandari M, El Rabbany M, Pierroz DD, Sulimani R, Saunders DP, Brown JP, Compston J International Task Force on Osteonecrosis of the Jaw. Diagnosis and management of osteonecrosis of the jaw: a systematic review and international consensus. J Bone Miner Res. 2015;30:3–23. doi: 10.1002/jbmr.2405. [DOI] [PubMed] [Google Scholar]
- 43.Rosella D, Papi P, Giardino R, Cicalini E, Piccoli L, Pompa G. Medication-related osteonecrosis of the jaw: clinical and practical guidelines. J Int Soc Prev Community Dent. 2016;6:97–104. doi: 10.4103/2231-0762.178742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Karna H, Gonzalez J, Radia HS, Sedghizadeh PP, Enciso R. Risk-reductive dental strategies for medication related osteonecrosis of the jaw among cancer patients: a systematic review with meta-analyses. Oral Oncol. 2018;85:15–23. doi: 10.1016/j.oraloncology.2018.08.003. [DOI] [PubMed] [Google Scholar]
- 45.Dimopoulos MA, Kastritis E, Bamia C, Melakopoulos I, Gika D, Roussou M, Migkou M, Eleftherakis-Papaiakovou E, Christoulas D, Terpos E, Bamias A. Reduction of osteonecrosis of the jaw (ONJ) after implementation of preventive measures in patients with multiple myeloma treated with zoledronic acid. Ann Oncol. 2009;20:117–120. doi: 10.1093/annonc/mdn554. [DOI] [PubMed] [Google Scholar]
- 46.Mücke T, Deppe H, Hein J, Wolff KD, Mitchell DA, Kesting MR, Retz M, Gschwend JE, Thalgott M. Prevention of bisphosphonate-related osteonecrosis of the jaws in patients with prostate cancer treated with zoledronic acid - A prospective study over 6 years. J Craniomaxillofac Surg. 2016;44:1689–1693. doi: 10.1016/j.jcms.2016.07.026. [DOI] [PubMed] [Google Scholar]
- 47.Vandone AM, Donadio M, Mozzati M, Ardine M, Polimeni MA, Beatrice S, Ciuffreda L, Scoletta M. Impact of dental care in the prevention of bisphosphonate-associated osteonecrosis of the jaw: a single-center clinical experience. Ann Oncol. 2012;23:193–200. doi: 10.1093/annonc/mdr039. [DOI] [PubMed] [Google Scholar]
- 48.Bramati A, Girelli S, Farina G, Dazzani MC, Torri V, Moretti A, Piva S, Dimaiuta M, La Verde N. Prospective, mono-institutional study of the impact of a systematic prevention program on incidence and outcome of osteonecrosis of the jaw in patients treated with bisphosphonates for bone metastases. J Bone Miner Metab. 2015;33:119–124. doi: 10.1007/s00774-014-0566-x. [DOI] [PubMed] [Google Scholar]
- 49.Campisi G, Fedele S, Fusco V, Pizzo G, Di Fede O, Bedogni A. Epidemiology, clinical manifestations, risk reduction and treatment strategies of jaw osteonecrosis in cancer patients exposed to antiresorptive agents. Future Oncol. 2014;10:257–275. doi: 10.2217/fon.13.211. [DOI] [PubMed] [Google Scholar]
- 50.Marx RE, Cillo JE, Jr, Ulloa JJ. Oral bisphosphonate-induced osteonecrosis: risk factors, prediction of risk using serum CTX testing, prevention, and treatment. J Oral Maxillofac Surg. 2007;65:2397–2410. doi: 10.1016/j.joms.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 51.Chiu WY, Chien JY, Yang WS, Juang JM, Lee JJ, Tsai KS. The risk of osteonecrosis of the jaws in Taiwanese osteoporotic patients treated with oral alendronate or raloxifene. J Clin Endocrinol Metab. 2014;99:2729–2735. doi: 10.1210/jc.2013-4119. [DOI] [PubMed] [Google Scholar]
- 52.Barasch A, Cunha-Cruz J, Curro FA, Hujoel P, Sung AH, Vena D, Voinea-Griffin AE CONDOR Collaborative Group. Beadnell S, Craig RG, DeRouen T, Desaranayake A, Gilbert A, Gilbert GH, Goldberg K, Hauley R, Hashimoto M, Holmes J, Latzke B, Leroux B, Lindblad A, Richman J, Safford M, Ship J, Thompson VP, Williams OD, Yin W. Risk factors for osteonecrosis of the jaws: a case-control study from the CONDOR dental PBRN. J Dent Res. 2011;90:439–444. doi: 10.1177/0022034510397196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Coleman R, Body JJ, Aapro M, Hadji P, Herrstedt J ESMO Guidelines Working Group. Bone health in cancer patients: ESMO clinical practice guidelines. Ann Oncol. 2014;25(Supplement 3):iii124–iii137. doi: 10.1093/annonc/mdu103. [DOI] [PubMed] [Google Scholar]
- 54.McCloskey EV, Johansson H, Harvey NC, Compston J, Kanis JA. Access to fracture risk assessment by FRAX and linked National Osteoporosis Guideline Group (NOGG) guidance in the UK-an analysis of anonymous website activity. Osteoporos Int. 2017;28:71–76. doi: 10.1007/s00198-016-3696-2. [DOI] [PubMed] [Google Scholar]
- 55.Fedele S, Kumar N, Davies R, Fiske J, Greening S, Porter S. Dental management of patients at risk of osteochemonecrosis of the jaws: a critical review. Oral Dis. 2009;15:527–537. doi: 10.1111/j.1601-0825.2009.01581.x. [DOI] [PubMed] [Google Scholar]
- 56.Kim I, Ki H, Lee W, Kim H, Park JB. The effect of systemically administered bisphosphonates on bony healing after tooth extraction and osseointegration of dental implants in the rabbit maxilla. Int J Oral Maxillofac Implants. 2013;28:1194–1200. doi: 10.11607/jomi.2685. [DOI] [PubMed] [Google Scholar]
- 57.Dhesy-Thind S, Fletcher GG, Blanchette PS, Clemons MJ, Dillmon MS, Frank ES, Gandhi S, Gupta R, Mates M, Moy B, Vandenberg T, Van Poznak CH. Use of adjuvant bisphosphonates and other bone-modifying agents in breast cancer: a Cancer Care Ontario and American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 2017;35:2062–2081. doi: 10.1200/JCO.2016.70.7257. [DOI] [PubMed] [Google Scholar]
- 58.Stockmann P, Hinkmann FM, Lell MM, Fenner M, Vairaktaris E, Neukam FW, Nkenke E. Panoramic radiograph, computed tomography or magnetic resonance imaging. Which imaging technique should be preferred in bisphosphonate-associated osteonecrosis of the jaw? A prospective clinical study. Clin Oral Investig. 2010;14:311–317. doi: 10.1007/s00784-009-0293-1. [DOI] [PubMed] [Google Scholar]
- 59.Bianchi SD, Scoletta M, Cassione FB, Migliaretti G, Mozzati M. Computerized tomographic findings in bisphosphonate-associated osteonecrosis of the jaw in patients with cancer. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;104:249–258. doi: 10.1016/j.tripleo.2007.01.040. [DOI] [PubMed] [Google Scholar]
- 60.Kang B, Cheong S, Chaichanasakul T, Bezouglaia O, Atti E, Dry SM, Pirih FQ, Aghaloo TL, Tetradis S. Periapical disease and bisphosphonates induce osteonecrosis of the jaws in mice. J Bone Miner Res. 2013;28:1631–1640. doi: 10.1002/jbmr.1894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Ferraz CC, Gomes NV, Gomes BP, Zaia AA, Teixeira FB, Souza-Filho FJ. Apical extrusion of debris and irrigants using two hand and three engine-driven instrumentation techniques. Int Endod J. 2001;34:354–358. doi: 10.1046/j.1365-2591.2001.00394.x. [DOI] [PubMed] [Google Scholar]
- 62.Gallego L, Junquera L, Pelaz A, Díaz-Bobes C. Rubber dam clamp trauma during endodontic treatment: a risk factor of bisphosphonate-related osteonecrosis of the jaw? J Oral Maxillofac Surg. 2011;69:e93–e95. doi: 10.1016/j.joms.2010.06.197. [DOI] [PubMed] [Google Scholar]
- 63.Moinzadeh AT, Shemesh H, Neirynck NA, Aubert C, Wesselink PR. Bisphosphonates and their clinical implications in endodontic therapy. Int Endod J. 2013;46:391–398. doi: 10.1111/iej.12018. [DOI] [PubMed] [Google Scholar]
- 64.AlRahabi MK, Ghabbani HM. Clinical impact of bisphosphonates in root canal therapy. Saudi Med J. 2018;39:232–238. doi: 10.15537/smj.2018.3.20923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Marx RE, Sawatari Y, Fortin M, Broumand V. Bisphosphonate-induced exposed bone (osteonecrosis/osteopetrosis) of the jaws: risk factors, recognition, prevention, and treatment. J Oral Maxillofac Surg. 2005;63:1567–1575. doi: 10.1016/j.joms.2005.07.010. [DOI] [PubMed] [Google Scholar]
- 66.Poubel VL, Silva CA, Mezzomo LA, De Luca Canto G, Rivero ER. The risk of osteonecrosis on alveolar healing after tooth extraction and systemic administration of antiresorptive drugs in rodents: a systematic review. J Craniomaxillofac Surg. 2018;46:245–256. doi: 10.1016/j.jcms.2017.11.008. [DOI] [PubMed] [Google Scholar]
- 67.Borromeo GL, Tsao CE, Darby IB, Ebeling PR. A review of the clinical implications of bisphosphonates in dentistry. Aust Dent J. 2011;56:2–9. doi: 10.1111/j.1834-7819.2010.01283.x. [DOI] [PubMed] [Google Scholar]
- 68.Saia G, Blandamura S, Bettini G, Tronchet A, Totola A, Bedogni G, Ferronato G, Nocini PF, Bedogni A. Occurrence of bisphosphonate-related osteonecrosis of the jaw after surgical tooth extraction. J Oral Maxillofac Surg. 2010;68:797–804. doi: 10.1016/j.joms.2009.10.026. [DOI] [PubMed] [Google Scholar]
- 69.Kwon YD, Ohe JY, Kim DY, Chung DJ, Park YD. Retrospective study of two biochemical markers for the risk assessment of oral bisphosphonate-related osteonecrosis of the jaws: can they be utilized as risk markers? Clin Oral Implants Res. 2011;22:100–105. doi: 10.1111/j.1600-0501.2010.01965.x. [DOI] [PubMed] [Google Scholar]
- 70.Lee CY, Suzuki JB. CTX biochemical marker of bone metabolism. Is it a reliable predictor of bisphosphonate-associated osteonecrosis of the jaws after surgery? Part II: a prospective clinical study. Implant Dent. 2010;19:29–38. doi: 10.1097/ID.0b013e3181cec8bc. [DOI] [PubMed] [Google Scholar]
- 71.Kunchur R, Need A, Hughes T, Goss A. Clinical investigation of C-terminal cross-linking telopeptide test in prevention and management of bisphosphonate-associated osteonecrosis of the jaws. J Oral Maxillofac Surg. 2009;67:1167–1173. doi: 10.1016/j.joms.2009.02.004. [DOI] [PubMed] [Google Scholar]
- 72.O'Connell JE, Ikeagwani O, Kearns GJ. A role for C-terminal cross-linking telopeptide (CTX) level to predict the development of bisphosphonate-related osteonecrosis of the jaws (BRONJ) following oral surgery? Ir J Med Sci. 2012;181:237–242. doi: 10.1007/s11845-011-0790-5. [DOI] [PubMed] [Google Scholar]
- 73.Kim KM, Rhee Y, Kwon YD, Kwon TG, Lee JK, Kim DY. Medication related osteonecrosis of the jaw: 2015 position statement of the Korean Society for Bone and Mineral Research and the Korean Association of Oral and Maxillofacial Surgeons. J Bone Metab. 2015;22:151–165. doi: 10.11005/jbm.2015.22.4.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Hasegawa T, Kawakita A, Ueda N, Funahara R, Tachibana A, Kobayashi M, Kondou E, Takeda D, Kojima Y, Sato S, Yanamoto S, Komatsubara H, Umeda M, Kirita T, Kurita H, Shibuya Y, Komori T Japanese Study Group of Cooperative Dentistry with Medicine (JCDM) A multicenter retrospective study of the risk factors associated with medication-related osteonecrosis of the jaw after tooth extraction in patients receiving oral bisphosphonate therapy: can primary wound closure and a drug holiday really prevent MRONJ? Osteoporos Int. 2017;28:2465–2473. doi: 10.1007/s00198-017-4063-7. [DOI] [PubMed] [Google Scholar]
- 75.de Molon RS, Shimamoto H, Bezouglaia O, Pirih FQ, Dry SM, Kostenuik P, Boyce RW, Dwyer D, Aghaloo TL, Tetradis S. OPG-Fc but not zoledronic acid discontinuation reverses osteonecrosis of the jaws (ONJ) in mice. J Bone Miner Res. 2015;30:1627–1640. doi: 10.1002/jbmr.2490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Ohga N, Yamazaki Y, Tsuboi K, Kitagawa Y. Healing of osteonecrosis of the jaw (ONJ) after discontinuation of denosumab in a patient with bone metastases of colorectal cancer: a case report and hypothesis. Quintessence Int. 2015;46:621–626. doi: 10.3290/j.qi.a33528. [DOI] [PubMed] [Google Scholar]
- 77.Yamazaki T, Yamori M, Ishizaki T, Asai K, Goto K, Takahashi K, Nakayama T, Bessho K. Increased incidence of osteonecrosis of the jaw after tooth extraction in patients treated with bisphosphonates: a cohort study. Int J Oral Maxillofac Surg. 2012;41:1397–1403. doi: 10.1016/j.ijom.2012.06.020. [DOI] [PubMed] [Google Scholar]
- 78.Tsao C, Darby I, Ebeling PR, Walsh K, O'Brien-Simpson N, Reynolds E, Borromeo G. Oral health risk factors for bisphosphonate-associated jaw osteonecrosis. J Oral Maxillofac Surg. 2013;71:1360–1366. doi: 10.1016/j.joms.2013.02.016. [DOI] [PubMed] [Google Scholar]
- 79.Allen MR. Medication-related osteonecrosis of the jaw: basic and translational science updates. Oral Maxillofac Surg Clin North Am. 2015;27:497–508. doi: 10.1016/j.coms.2015.06.002. [DOI] [PubMed] [Google Scholar]
- 80.Hikita H, Miyazawa K, Tabuchi M, Kimura M, Goto S. Bisphosphonate administration prior to tooth extraction delays initial healing of the extraction socket in rats. J Bone Miner Metab. 2009;27:663–672. doi: 10.1007/s00774-009-0090-6. [DOI] [PubMed] [Google Scholar]
- 81.Landesberg R, Woo V, Cremers S, Cozin M, Marolt D, Vunjak-Novakovic G, Kousteni S, Raghavan S. Potential pathophysiological mechanisms in osteonecrosis of the jaw. Ann N Y Acad Sci. 2011;1218:62–79. doi: 10.1111/j.1749-6632.2010.05835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Ravosa MJ, Ning J, Liu Y, Stack MS. Bisphosphonate effects on the behaviour of oral epithelial cells and oral fibroblasts. Arch Oral Biol. 2011;56:491–498. doi: 10.1016/j.archoralbio.2010.11.003. [DOI] [PubMed] [Google Scholar]
- 83.Pabst AM, Ziebart T, Koch FP, Taylor KY, Al-Nawas B, Walter C. The influence of bisphosphonates on viability, migration, and apoptosis of human oral keratinocytes--in vitro study. Clin Oral Investig. 2012;16:87–93. doi: 10.1007/s00784-010-0507-6. [DOI] [PubMed] [Google Scholar]
- 84.Yamashita J, Koi K, Yang DY, McCauley LK. Effect of zoledronate on oral wound healing in rats. Clin Cancer Res. 2011;17:1405–1414. doi: 10.1158/1078-0432.CCR-10-1614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Allam E, Allen M, Chu TM, Ghoneima A, Jack Windsor L. In vivo effects of zoledronic acid on oral mucosal epithelial cells. Oral Dis. 2011;17:291–297. doi: 10.1111/j.1601-0825.2010.01739.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Iwamatsu-Kobayashi Y, Satoh-Kuriwada S, Yamamoto T, Hirata M, Toyoda J, Endo H, Kindaichi K, Komatsu M. A case of multiple idiopathic external root resorption: a 6-year follow-up study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2005;100:772–779. doi: 10.1016/j.tripleo.2004.11.047. [DOI] [PubMed] [Google Scholar]
- 87.Patel S, Saberi N. External cervical resorption associated with the use of bisphosphonates: a case series. J Endod. 2015;41:742–748. doi: 10.1016/j.joen.2015.01.035. [DOI] [PubMed] [Google Scholar]
- 88.Hewitt RE, Lissina A, Green AE, Slay ES, Price DA, Sewell AK. The bisphosphonate acute phase response: rapid and copious production of proinflammatory cytokines by peripheral blood gd T cells in response to aminobisphosphonates is inhibited by statins. Clin Exp Immunol. 2005;139:101–111. doi: 10.1111/j.1365-2249.2005.02665.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Makkonen N, Salminen A, Rogers MJ, Frith JC, Urtti A, Azhayeva E, Mönkkönen J. Contrasting effects of alendronate and clodronate on RAW 264 macrophages: the role of a bisphosphonate metabolite. Eur J Pharm Sci. 1999;8:109–118. doi: 10.1016/s0928-0987(98)00065-7. [DOI] [PubMed] [Google Scholar]
- 90.Dicuonzo G, Vincenzi B, Santini D, Avvisati G, Rocci L, Battistoni F, Gavasci M, Borzomati D, Coppola R, Tonini G. Fever after zoledronic acid administration is due to increase in TNF-alpha and IL-6. J Interferon Cytokine Res. 2003;23:649–654. doi: 10.1089/107999003322558782. [DOI] [PubMed] [Google Scholar]
- 91.Deeb JG, Azarnoush K, Laskin DM, Deeb GR. Discontinuation of denosumab as a potential cause of generalized external cervical root resorption: a case report. J Endod. 2019;45:640–644. doi: 10.1016/j.joen.2019.02.013. [DOI] [PubMed] [Google Scholar]
- 92.Eastell R, Christiansen C, Grauer A, Kutilek S, Libanati C, McClung MR, Reid IR, Resch H, Siris E, Uebelhart D, Wang A, Weryha G, Cummings SR. Effects of denosumab on bone turnover markers in postmenopausal osteoporosis. J Bone Miner Res. 2011;26:530–537. doi: 10.1002/jbmr.251. [DOI] [PubMed] [Google Scholar]
- 93.Hsiao A, Glickman G, He J. A retrospective clinical and radiographic study on healing of periradicular lesions in patients taking oral bisphosphonates. J Endod. 2009;35:1525–1528. doi: 10.1016/j.joen.2009.07.020. [DOI] [PubMed] [Google Scholar]
- 94.Dereci Ö, Orhan EO, Irmak Ö, Ay S. The effect of the duration of intravenous zolendronate medication on the success of non-surgical endodontic therapy: a retrospective study. BMC Oral Health. 2016;16:9. doi: 10.1186/s12903-016-0163-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Knight RJ, Reddy C, Rtshiladze MA, Lvoff G, Sherring D, Marucci D. Bisphosphonate-related osteonecrosis of the jaw: tip of the iceberg. J Craniofac Surg. 2010;21:25–32. doi: 10.1097/SCS.0b013e3181c347a0. [DOI] [PubMed] [Google Scholar]