Abstract
A 76-year-old Japanese man visited a nearby medical clinic complaining of abdominal distention. He had undergone extraperitoneal laparoscopic prostatectomy at our institution 5 months before the onset of abdominal distention. An imaging study revealed a large cystic lesion, and biochemical examination of a sample obtained via cyst puncture led to a diagnosis of lymphocele. As the lymphocele was resistant to puncture, drainage, and sclerotherapy with minomycin, laparoscopic fenestration was performed. Although the patient developed an adhesive ileus postoperatively, the cyst has not recurred. Fenestration surgery is a feasible option for lymphocele refractory to various conservative therapies.
Keywords: lymphocele, laparoscopy, prostatectomy
Introduction
Lymphocele is one of the postoperative complications occurring after procedures such as retroperitoneum lymph node dissection or para-aortic lymph node dissection.
The incidence of lymphocele after laparoscopic lymph node dissection is reported to be 29%1), and lymphocele is reported as the most frequent non-functional complication of radical prostatectomy and pelvic lymph node dissection2).
Most lymphoceles are known to be small and asymptomatic and sometimes disappear naturally, but they may cause severe symptoms such as secondary infection2), thrombotic events2), and renal failure3), among others, when enlarged. Although the treatment strategy for lymphocele has not been established yet, when lymphocele is symptomatic, paracentesis, sclerotherapy, or surgeries such as fenestration are performed4).
Herein, we report a case of lymphocele that was refractory to paracentesis and sclerotherapy and performed laparoscopic fenestration surgery of the cyst at our institution.
Case Report
A 76-year-old Japanese man visited a nearby medical clinic complaining of abdominal distention. He presented at our department for further examination and treatment. Extraperitoneal laparoscopic prostatectomy had been performed for his prostate cancer at our institution 5 months before he complained of abdominal distention. His physical examination results and vital signs were normal. He had a medical history of appendicitis and osteoarthritis. His blood test results were also unremarkable. Urinary examination showed hematuria but negative urine cytology. Total body computed tomography (CT) revealed the presence of a 10-cm-sized cystic lesion on the ventral side of his bladder (Figure 1). A retrograde cystourethrogram showed no connection between the cystic lesion and urinary tract. First, cystic lesion puncture was performed for drainage and to identify the components of the lesion content. The lesion content was approximately 300 ml in volume and the creatinine concentration was 0.6 mg/dl (normal creatinine content of urine is 67–100 mg/dl in our hospital); thus, the lesion content was not considered. On the basis of these findings, the cystic lesion was finally diagnosed as pelvic lymphocele, which was considered to have been caused by lymph node dissection on laparoscopic radical prostatectomy. As lymphocele recurred 2 weeks after paracentesis, sclerotherapy was chosen as a second treatment. A 16-Fr pigtail catheter was placed in the cyst to drain its contents, and 100 ml of minomycin (1 mg/ml each time, 3 times every 3 days) was injected into the lymphocele. However, 3 weeks after sclerotherapy, the patient complained of abdominal distention again and lymphocele recurrence was confirmed using ultrasonography. As the lymphocele was considered refractory and difficult to manage by paracentesis and sclerotherapy, laparoscopic fenestration surgery was finally performed. A total of 3 ports were inserted: a 10-cm multi-channel port inserted just beside the patient’s navel and two 5-mm ports on his bilateral lower quadrants, one on the right side of the appendectomy scar and the other on the left side of the laparoscopic radical prostatectomy scar (Figure 2). The 10-cm-sized lymphocele was identified by the intraperitoneal approach (Figure 3a). The entire lymphocele could not be completely removed because a part of the lymphocele was strongly adhered to the surrounding area. Therefore, lymphocele dissection was performed (Figure 3b) by opening the cyst wall and removing the lymphocele as much as possible, except in the adhered areas. Furthermore, the open areas that could not be removed were electrocoagulated. Three days postoperatively, the patient developed adhesive ileus. The inserted ileus tube did not work well; thus, open ileus surgery was performed. After the ileus surgery, the patient recovered and was discharged from the hospital in a few weeks. He is alive without prostate cancer, lymphocele, and ileus recurrence until 5 months after the laparoscopic fenestration surgery of the lymphocele.
Figure 1.
Enhanced coronal view CT image. A cystic mass (arrow) was observed on the ventral side of the patient’s bladder (arrowhead).
Figure 2.
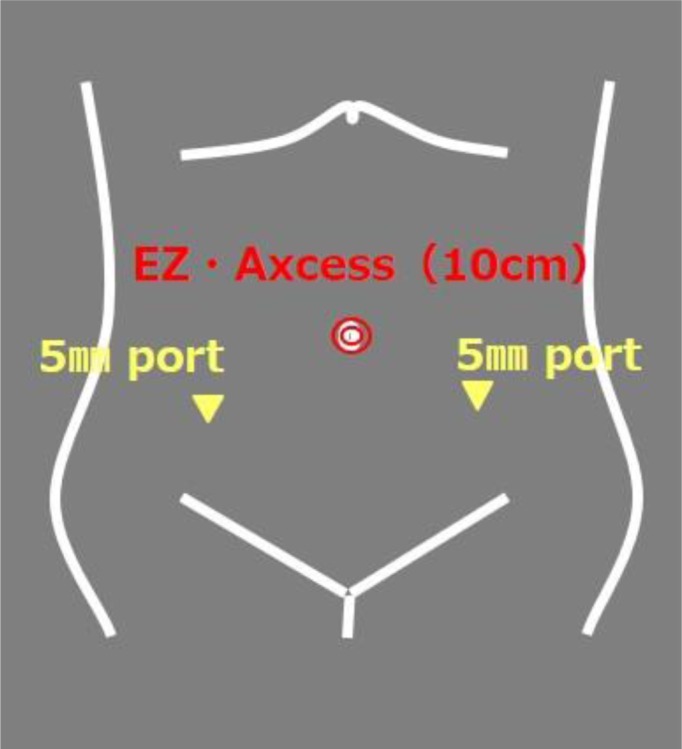
Three ports were inserted: a 10-cm multi-channel port just beside the navel and two 5-mm ports on the bilateral lower quadrants: one on the right side of the appendectomy scar and the other on the left side of the laparoscopic radical prostatectomy scar.
Figure 3.
(a) Lymphocele occupied the Retzius’ space (arrowhead). (b) Center of the lymphocele, which is fenestrated (arrow).
Discussion
Lymphocele is a common complication after radical prostatectomy and bilateral pelvic lymph node dissection. The incidence of lymphocele after laparoscopic lymph node dissection is reported to be 29%1). Cases of lymphocele that are ≥5 cm are rare, and even fewer cause clinical consequences5). The incidence rate of symptomatic lymphocele occurring after radical prostatectomy and bilateral pelvic lymph node dissection has been reported to be 4%, with a median time to presentation of 19 days6). The primary presenting complaints reported are fever in 47%, abdominal pain in 40%, and lower extremity swelling in 37%6). In our case, the patient complained of abdominal distention, a nonspecific symptom, but lymphocele was not difficult to diagnose using diagnostic imaging and based on the past medical history of pelvic lymph node dissection.
Several management options are available for lymphocele. Most lymphoceles naturally disappear, but some of them enlarge and need treatments such as paracentesis and drainage. As conservative therapy, transcutaneous drainage and sclerotherapy using agents such as tetracycline and povidone iodine are selected7, 8). Approximately 50% of lymph cysts have been reported to disappear after a paracentesis or transcutaneous drainage alone, and approximately 80–90% of them disappear after sclerotherapy7, 8). Tetracycline, mostly minomycin, is used as sclerotherapy to reduce the low pH level (2.0–3.5) and finally causes cyst inflammation and sclerosis8). As minomycin is used as an antibiotic with a well-established safety, it was selected for sclerotherapy in our case. Considering the dose of minocycline, 80% of lymphoceles have been reported to disappear in the group using 100 mg of minocycline, whereas 86% of them disappear in the group using 200 mg of minocycline8). In our case, 300 mg of minomycin was administered because the cyst was considered large and 200 mg of minocycline was not considered as a suitable dose for efficient drug dispersion. Surgical options, such as lymphocelectomy and fenestration, are selected when the lymphocele is refractory to drug treatment. Fenestration performed as a laparoscopic procedure yielded a 97% disappearance rate of the lymphocele postoperatively9). A comparison of laparoscopic and open surgery showed that laparoscopic marsupialization is more effective, usually immediately definitive, results in minimal patient morbidity, and allows more rapid recovery10). We chose laparoscopic fenestration surgery because the patient had opted for laparoscopic radical prostatectomy considering its esthetic outcome. A few reports have demonstrated that laparoscopic fenestration itself causes adhesive ileus. In general, laparoscopic surgery can be a cause of adhesive ileus, but whether the ileus event is caused by fenestration remains unclear.
Conclusion
We reported that lymphocele developed after extraperitoneal laparoscopic radical prostatectomy and lymph node dissection. The possibility of lymphocele development should be considered during the follow-up of patients who have undergone extraperitoneal laparoscopic radical prostatectomy and lymph node dissection. Moreover, if the lymphocele is resistant to conservative therapies such as puncture, drainage, and sclerotherapy, fenestration surgery is a feasible method to treat the lymphocele.
Conflict of interest
None declared.
References
- 1.Solberg A, Angelsen A, Bergan U. Frequency of lymphoceles after open and laparoscopic pelvic lymph node dissection in patients with prostate cancer. Scand J Urol Nephrol 2003; 37: 218–221. doi: 10.1080/00365590310008082 [DOI] [PubMed] [Google Scholar]
- 2.Khoder WY, Trottmann M, Buchner A. Risk factors for pelvic lymphoceles post-radical prostatectomy. Int J Urol 2011; 18: 638–643. [DOI] [PubMed] [Google Scholar]
- 3.Sihra N, Kujawa M, Counsell A. Post-prostatectomy lymphocoele presenting with renal failure. Urology 2019; 123: e9–e10. doi: 10.1016/j.urology.2018.09.023 [DOI] [PubMed] [Google Scholar]
- 4.White M, Mueller PR, Ferrucci JT., Jr Percutaneous drainage of postoperative abdominal and pelvic lymphoceles. AJR Am J Roentgenol 1985; 145: 1065–1069. doi: 10.2214/ajr.145.5.1065 [DOI] [PubMed] [Google Scholar]
- 5.Loeb S, Partin AW, Schaeffer EM. Complications of pelvic lymphadenectomy: do the risks outweigh the benefits? Rev Urol 2010; 12: 20–24. [PMC free article] [PubMed] [Google Scholar]
- 6.Gotto GT, Yunis LH, Guillonneau B. Predictors of symptomatic lymphocele after radical prostatectomy and bilateral pelvic lymph node dissection. Int J Urol 2011; 18: 291–296. doi: 10.1111/j.1442-2042.2010.02710.x [DOI] [PubMed] [Google Scholar]
- 7.Gilliland JD, Spies JB, Brown SB. Lymphoceles: percutaneous treatment with povidone-iodine sclerosis. Radiology 1989; 171: 227–229. doi: 10.1148/radiology.171.1.2648473 [DOI] [PubMed] [Google Scholar]
- 8.Okasho A, Yamamoto H, Asari T. [A new treatment of simple renal cyst: percutaneous instillation of minocycline hydrochloride into simple renal cyst]. Hinyokika Kiyo 1987; 33: 1162–1166 (in Japanese, Abstract in English). [PubMed] [Google Scholar]
- 9.Khoder WY, Gratzke C, Haseke N. Laparoscopic marsupialisation of pelvic lymphoceles in different anatomic locations following radical prostatectomy. Eur Urol 2012; 62: 640–648. doi: 10.1016/j.eururo.2012.05.060 [DOI] [PubMed] [Google Scholar]
- 10.Gill IS, Hodge EE, Munch LC. Transperitoneal marsupialization of lymphoceles: a comparison of laparoscopic and open techniques. J Urol 1995; 153: 706–711. doi: 10.1016/S0022-5347(01)67693-6 [DOI] [PubMed] [Google Scholar]




