Abstract
Although ambulatory data collection techniques have been used in elderly populations, their feasibility and validity amongst elderly individuals with cognitive impairment and amongst couples remains unexplored. The main objective of this study is to examine the validity of Ecological Momentary Assessment (EMA) in elderly persons with or without cognitive impairment and their spouses. The sample included 58 retired farmers (mean 77.3 years, standard deviation [SD] 5.5) with or without cognitive impairment, recruited within a French cohort and 60 spouses (mean 73.4 years, SD 6.9). The presence of cognitive impairment determining by a panel of specialized neurologists permitted to define two groups: “The Cognitive Impairment Group” and “The Control Group”. EMA procedures consisted of repeated telephone interviews five times per day during four days for each spouse. Our results demonstrate the validity of EMA procedures through a 92.1% level of compliance, the absence of fatigue effects, and the lack of evidence for major reactivity to the methods. However, the specificity of our sample may explain the acceptance (42%) and response (75%) rates and may reduce the generalizability of the results to the general population of elderly individuals. Finally, the validation of such techniques may contribute to future research examining community‐dwelling elderly individuals and their spouses. Copyright © 2013 John Wiley & Sons, Ltd.
Keywords: elderly couples, community, cognitive impairment, Ecological Momentary Assessment, validity
Introduction
Despite growing interest for ambulatory monitoring in psychiatry, a relatively small portion of studies have been conducted in the elderly in the last two decades (Cain et al., 2009). Ecological Momentary Assessment (EMA) techniques (Moskowitz and Young, 2006; Schiffman et al., 2008) such as the Experience Sampling Method (ESM; Csikszentmihalyi and Larson, 1987; Hektner et al., 2007) have been used in elderly populations to prospectively assess behavior, social interactions, and environmental contexts (Bouisson and Swendsen, 2003; Cain et al., 2009). EMA methods rely on repeated within‐day and between‐day assessments in ecologically valid contexts to examine the daily life functioning of individuals. The main advantage of EMA is its ability to gather real time data on affective, behavioral, and contextual experiences (Cain et al., 2009) thereby reducing retrospective recall bias (Bolger et al., 2003; Hurlburt, 1997; Johnson et al., 2009; Scollon, et al., 2003). However, studies to date have focused on elderly persons with normal cognitive functioning and have typically excluded those with a Mini Mental State Examination (MMSE; Folstein et al., 1975) score equal or lower than 24 points (Cain et al., 2009). Given the increase in cognitive impairment and the risk of neurodegenerative diseases with age (Bäckman et al., 2004), it may be important to include these individuals in studies of the elderly. Examining the validity of ambulatory techniques in elderly populations with mild or moderate cognitive impairments may prove helpful for future studies of daily life functioning.
In addition to including individuals with mild cognitive impairment, investigations focused on daily life experiences and functioning of elderly individuals may benefit from the inclusion of live‐in partners. Daily experiences, emotions and behaviors of persons living in close proximity are interrelated. Moreover, one family member's daily experiences would affect the other family member's emotions or behaviors (e.g. Larson and Almeida, 1999). However, to our knowledge, no study involving ambulatory monitoring in elderly individuals has involved couples, and the feasibility of such methods needs to be examined. Larson and Almeida (1999) underlined the interests to consider interrelatedness of the wife–husband relationship to better understand daily life expression of vulnerability.
An important decision when implementing EMA techniques is the data collection procedure itself. EMA has relied on paper and pencil techniques, cell phones, personal digital assistants or microcomputers, and more recently smartphones (Schiffman et al., 2008). While computerized methods are preferred in healthy or psychiatric samples, their use remains limited in elderly subjects due to their inability or unwillingness to use such devices (Namazi and McClintic, 2003). Paper and pencil protocols are the most frequently used in the elderly (Cain et al., 2009). However, patients often provide inaccurate reports of assessment times when using such techniques, thereby biasing estimates of compliance and reactive effects. Relying on study phones may be the most suitable data collection technique in elderly populations, with a high participation rate combined with a means by which to monitor the actual time of each assessment (Bouisson, 2002; Bouisson and Swendsen, 2003).
When examining the feasibility and validity of ambulatory monitoring in a given population, two important parameters are typically examined: compliance and reactivity. Compliance includes participation or acceptance rates, and the proportion of daily assessments the participant responded to (Johnson et al., 2009; Ohly et al., 2010). Reactivity refers to the potential effect of the repeated assessment procedure itself on the subject's responses. Repeated within‐day assessments over periods of several days may contribute to alter the frequency or the intensity of the variables under study, through increased awareness of specific responses. EMA studies conducted in the elderly commonly do not report these parameters, though they remain essential to the understanding of the validity of these methods in this population. The main objective of the present study is to examine the feasibility and validity of telephone‐based EMA procedures in elderly persons with varying levels of cognitive impairment and their spouses by assessing: (1) acceptance rates and compliance, (2) fatigue effects, and (3) reactivity to EMA procedures.
Methods
Participants
The present study is based on a large prospective epidemiological cohort study named Aging Multidisciplinary Investigation/Agrica‐MSA‐Institut de recherche en santé publique (AMI). This longitudinal four‐year design began in 2007 and included a sample of 1002 retired farmers over 70 years old, living in rural areas of southern France (Pérès et al., 2012). The participants of the present study were drawn from the AMI cohort. Inclusion criteria included: (1) living in the community, (2) living with his or her spouse, (3) speaking and understanding French, and (4) having mild or moderate cognitive impairments defined clinically. All AMI participants completed a comprehensive battery of neuropsychological tests. Participants classified by a panel of specialized neurologists as presenting a clinical dementia diagnosis or mild cognitive impairment were selected. Exclusion criteria were: (1) living in a retirement home (to avoid bias to the rhythms imposed by a retirement home), (2) severe hearing impairment, (3) inability to provide informed consent or to follow basic research procedures, and (4) having a MMSE score equal or lower than 16 points to exclude severely cognitively impaired individuals in order to ensure that participants would be capable of providing informed consent.
Among the AMI sample, 67 participants (32 participants with dementia and 35 participants with mild cognitive impairment) met inclusion criteria for the Cognitive Impairment Group (CIG) based on a clinical dementia diagnosis or mild cognitive impairment, living at home with his or her spouse, and speaking French. Each participant was then matched on socio‐demographic variables (age, gender, and educational level) with two or more AMI participants without cognitive impairment (n =162, the latter group being referred to as the Control Group or CG) and characterized by similar age, gender, and educational level. A flow chart reporting sample selection is presented in Figure 1. After this initial selection, members of the research team verified eligibility and the willingness of both spouses to participate in the present study, further reducing the final sample enrolled in the study.
Figure 1.
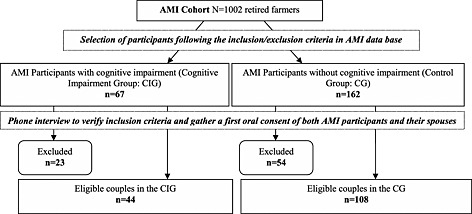
Study flow chart.
A total of 23 couples were excluded from the CIG and 54 from the CG. Of the couples excluded from the CIG, 19 (82.6%) were excluded due to morbidity or mortality (death, hospitalization, recent admission in a nursing home, mental or physical disabilities). A minority (n = 4) were excluded for language comprehension difficulties or refusal to participate in further AMI assessments. Of the couples excluded in the CG, 34 (62.9%) were excluded due to morbidity or mortality and 20 for logistical reasons. The final sample of eligible couples comprised 304 individuals: 44 AMI participants in the CIG and 108 in the CG and their respective spouses (Figure 1).
Procedure
Written informed consent was obtained from each participant, including spouses, and each couple was randomly assigned to one of six EMA periods of four consecutive days.
EMA procedure
EMA assessments start days were counterbalanced across weekdays in order to capture a variety of behaviors and situations. Five times per day, for four consecutive days, each participant and spouse received a telephone call on their landline from a member of the research team. The person answering the telephone was interviewed first, the spouse was interviewed either immediately after or within a period of one hour. All phone assessments were scheduled at fixed intervals and occurred approximately every three hours between 8:00 a.m. and 10:00 p.m., within the following time intervals 8:00 to 11:00 a.m., 11:00 a.m. to 2:00 p.m., 2:00 to 5:00 p.m., 5:00 to 8:00 p.m., and finally, 8:00 to 10:00 p.m. Each telephone interview lasted approximately five minutes.
Materials
Socio‐demographic and clinical variables
Socio‐demographic variables included age, sex, and education. Education level was divided into two categories as follows: low educational level which corresponds to participants without schooling or having only obtained the French “Certificat d'Etudes Primaires”, equivalent to seventh grade; and medium to high level which corresponds to participants with a higher education level.
Global cognitive functioning was examined using the MMSE (Folstein et al., 1975), with scores ranging from 0 to 30 points.
Compliance and ambulatory measures
Minimum compliance and response rates
An EMA assessment was considered valid if both partners responded within one hour of each other in order to minimize potential retrospective biases and reducing time intervals between spouses. Compliance was defined as the provision of more than one full day of valid assessments per assessment period, or six valid assessments in order to provide minimally sufficient data for examining both within‐day and between‐day variation (Johnson et al., 2009). Response rates among individuals meeting minimum compliance were then calculated considering the total number of valid assessments for each individual divided by the total number of scheduled phone interviews (Johnson et al., 2009).
Behaviors, environments, social contexts, and psychological states
The assessments of behavior, physical environment and social relations at the time of the telephone call and occurring since the previous telephone call were similar to those used in previous ESM studies (e.g. Bouisson and Swendsen, 2003). Each spouse was asked to describe what they were doing (behavior), where they were at (physical environment), and with whom (social company) at the time of the telephone call, and since the previous telephone call. Examples of questions are: “What are you doing right now? Where are you right now and with whom?” Answers were subsequently classified using previously established categories (Bouisson and Swendsen, 2003; Brandstatter, 1994). These categories were then classified into three broader categories. Behavior was coded as: “Inactive”, “Home activities”, or “Social activities”. Environment was coded as: “Inside the house”, “Outside the house”, or “In other places”. Social company was coded as being “Alone”, “With spouse”, or “With other person”.
Each participant was asked to indicate, on a five‐point Likert scale, their current level of well‐being, sadness, loneliness, anxiety and tiredness.
Overview of statistical analyses
Between‐group comparisons of socio‐demographic variables, compliance and response rates were carried out with R (R Development Core Team, 2008). The χ 2 test was used to compare percentages, and Fisher's exact test was used when appropriate. Independent sample t‐tests were used to compare means. The normality of the distribution of each variable was assessed using a normal probability plot and the Shapiro–Wilk test. In case of significant deviations from normal distribution and heterogeneity of variance, appropriate non‐parametric tests were used in place of t‐tests.
EMA data were analyzed using Hierarchical Linear and Non‐linear Modeling (HLM 6.03; Raudenbush et al., 2005) to accommodate the hierarchical structure of the data. Sample size was calculated according to the parameter being tested in the regressions computed. Previous studies have recommended a minimum of 20 units at level 2 in order to execute multilevel analyses (e.g. Bressoux, 2010; Kreft, 1996) and to assure good coefficients estimation in reducing error measures. Moreover, as we used growth multilevel modeling, a small level 2 n may be partially offset by a large number of observations at level 1. Intercepts‐and‐slopes as outcomes models were used to examine compliance, fatigue, and reactivity effects. All analyses controlled for sex, education level, and age. Dichotomous variables were estimated using Bernoulli models. Regression coefficients (γ) are presented for both dichotomous and continuous variables.
Results
Study acceptance
Full study acceptance was considered when both spouses agreed to participate. Overall, of those offered participation (n = 152), 41.5% (n = 63) agreed to participate, 34.1% (n = 15) of the CIG, and 44.5% (n = 48) of the CG (Table 1).
Table 1.
Socio‐demographic characteristics of eligible AMI participants by study acceptance status.
| Cognitive impairment group | Control group | All | ||||
|---|---|---|---|---|---|---|
| Eligible AMI participants N = 152 | Study acceptance n = 15 | Study refusal n = 29 | Study acceptance n = 48 | Study refusal n = 60 | Study acceptance n = 63 | Study refusal n = 89 |
| Age, mean (SD) | 76.4 (5.3) | 78.8 (4.9) | 76.8 (5.6) | 76.9 (5.9) | 76.7 (5.5) | 77.5 (5.6) |
| Sex, n (%) | ||||||
| Male | 12 (80.0) | 25 (86.2) | 43 (89.6) | 49 (81.7) | 55 (87.3) | 74 (83.1) |
| Female | 3 (20.0) | 4 (13.8) | 5 (10.4) | 11 (18.3) | 8 (12.7) | 15 (16.9) |
| Education levela, n (%) | ||||||
| Low, medium low | 11 (73.3) | 17 (58.6) | 14 (29.2)** | 35 (58.3) | 25 (39.7)* | 52 (58.4) |
| Medium high, high | 4 (26.7) | 12 (41.4) | 34 (70.8) | 25 (41.7) | 38 (60.3) | 37 (41.6) |
| MMSEb, mean (SD) | 23.6 (3.1) | 24.5 (2.8) | 27.5 (1.7)* | 26.5 (2.1) | 26.6 (2.7) | 25.8 (2.5) |
Educational level: (0) without schooling or having only obtained the French “Certificat d'Etudes Primaires” (equivalent to seven years of schooling); (1) higher education level.
MMSE = Mini Mental State Examination with scores ranging from 0 to 30 points.
Note: Statistical comparisons for the cognitive impairment group, the control group and all eligible AMI participants by study acceptance status: percentages were compared using chi‐square tests; means were compared using t‐tests or appropriate nonparametric test.
p < 0.05.
p < 0.01.
Bivariate comparisons indicate that those who agreed to participate had a higher level of education as compared to those who refused in the overall sample (χ 2 (1, 152) = 5.185, p < 0.05) and in the CG (χ 2 (1, 108) = 9.153, p < 0.01) but not in the CIG. In the CG, those who agreed to participate also had a higher MMSE score (W = 1060.5, p < 0.05, 95% confidence interval [CI] [−1.999 ; –0.000]). No differences regarding sex or age were observed.
In the CIG and CG, reasons for refusing to participate included: being unavailable during the time of the study (65.5% and 61.6%, respectively), having health problems (27.5% and 15.0%, respectively) and having too frequent requests for research or refusing ambulatory monitoring procedure (6.7% and 23.3%, respectively).
Compliance with EMA procedures
Results show no significant between‐group differences in minimal compliance (see Table 2). However, the average number of valid responses was greater in the CG as compared to the CIG (t (56, 6) = 2.986, p < 0.01).
Table 2.
Compliance and response rates by group status
| Cognitive impairment group n = 15 | Control group n = 48 | All n = 63 | |
|---|---|---|---|
| Minimum compliance, n (%) | |||
| Participant | 12 (80.0) | 46 (95.8) | 58 (92.1) |
| Spouse | 13 (86.6) | 47 (97.9) | 60 (95.2) |
| Average response ratesa | |||
| Participant | |||
| mean (SD) | 12.6 (2.3)** | 15.5 (3.2) | 14.9 (3.2) |
| percentage | 62.5 | 77.5 | 74.5 |
| Spouse | |||
| mean (SD) | 14.3 (2.9) | 15.3 (3.3) | 15.1 (3.2) |
| percentage | 71.5 | 76.5 | 75.5 |
Average response and rate are calculated among retired farmers and spouses having minimum compliance.
Note: Statistical comparisons between the cognitive impairment group and the control group: between‐group means comparisons using t‐tests or appropriate non‐parametric test.
p < 0.05.
p < 0.01.
Fatigue and reactivity
Fatigue effects and reactivity were examined in participants meeting minimum compliance criteria (see Table 3 for description). Results indicate no fatigue effects in the overall sample or within each group as the frequency of missing data was not affected by the duration of the study (Table 4).
Table 3.
Sample characteristics of couples with minimal compliance by group status
| Cognitive impairment group | Control group | All | |
|---|---|---|---|
| Participants | n = 12 | n = 46 | n = 58 |
| Age, mean (SD) | 77.2 (5.5) | 77.4 (5.5) | 77.3 (5.5) |
| Sex, n (%) | |||
| Male | 9 (75.0) | 41 (89.1) | 50 (86.2) |
| Female | 3 (25.0) | 5 (10.9) | 8 (13.8) |
| Education levela, n (%) | |||
| Low, medium low | 12 (100.0) | 36 (78.3) | 48 (82.8) |
| Medium high, high | 0 (0.0) | 10 (21.7) | 10 (17.2) |
| MMSEb, mean (SD) | 24.2 (3.1)** | 27.5 (1.8) | 26.8 (2.5) |
| Spouses | n = 13 | n = 47 | n = 60 |
| Age, mean (SD) | 72.7 (7.2) | 73.6 (6.9) | 73.4 (6.9) |
| Sex, n (%) | |||
| Male | 0 (0) | 2 (4.3) | 2 (3.3) |
| Female | 13 (100) | 45 (95.7) | 58 (96.7) |
| Education levela, n (%) | |||
| Low, medium low | 10 (76.9) | 32 (68.1) | 42 (70.0) |
| Medium high, high | 3 (23.1) | 15 (31.9) | 18 (30.0) |
Educational level: (0) without schooling or having only obtained the French “Certificat d'Etudes Primaires” (equivalent to seven years of schooling); (1) higher education level.
MMSE = Mini Mental State Examination with scores ranging from 0 to 30 points.
Note: Statistical comparisons between the cognitive impairment group and the control group: percentages were compared using chi‐square tests; means were compared using t‐tests or appropriate non‐parametric test.
p < 0.05.
p < 0.01.
Table 4.
Frequency of specific environments, social contexts, behaviors and psychological states as a function of time of study
| Participants cognitive impairment group n = 12 | Participants control group n = 46 | Spouses cognitive impairment group n = 13 | Spouses control group n = 47 | All n = 118 | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Variables | γ | SE | γ | SE | γ | SE | γ | SE | γ | SE |
| Compliance | ||||||||||
| Missing data | −0.018 | 0.024 | 0.018 | 0.012 | 0.014 | 0.027 | 0.009 | 0.016 | 0.009 | 0.008 |
| Environment | ||||||||||
| Inside house | −0.009 | 0.025 | 0.009 | 0.013 | 0.026 | 0.020 | −0.005 | 0.013 | 0.002 | 0.007 |
| Outside house | −0.005 | 0.031 | −0.009 | 0.016 | −0.023 | 0.024 | −0.000 | 0.015 | −0.006 | 0.008 |
| Social context | ||||||||||
| With spouse | −0.006 | 0.036 | 0.004 | 0.015 | 0.015 | 0.041 | −0.000 | 0.012 | 0.000 | 0.008 |
| With other person | 0.006 | 0.037 | 0.001 | 0.015 | −0.006 | 0.039 | 0.007 | 0.013 | 0.004 | 0.008 |
| Activity | ||||||||||
| Home activities | −0.025 | 0.033 | −0.008 | 0.017 | −0.049 | 0.026 | −0.006 | 0.018 | −0.013 | 0.010 |
| Social activities | −0.003 | 0.034 | 0.011 | 0.021 | 0.023 | 0.030 | −0.014 | 0.021 | −0.005 | 0.011 |
| Psychological states | ||||||||||
| Well‐beinga | 0.007 | 0.013 | 0.000 | 0.003 | 0.000 | 0.010 | −0.000 | 0.000 | 0.000 | 0.011 |
| Tirednessb | 0.083 | 0.023** | 0.029 | 0.016 | 0.093 | 0.019** | 0.015 | 0.017 | 0.033 | 0.009** |
Note: Analyses included only variables where each modality of response comprised at least 10% of valid observations. Age, sex and education level were entered as covariates. Regression coefficients (γ) are presented for both dichotomous and continuous variables. The p‐values reflect Bonferroni adjustments for multiple comparisons.
p < 0.05.
p < 0.01.
This variable is coded 1 for the lowest levels of well‐being and 0 for the highest levels of well‐being.
This variable is coded 1 for the lowest levels of tiredness and 0 for the highest levels of tiredness.
No major reactivity effects were found. The frequency of specific physical and social environments, or behaviors did not significantly change as a function of study.
When examining reactivity in psychological variables, overall, couples and more specifically participants in the CIG and their spouses, reported decreased tiredness as the study progressed (respectively γ = 0.033, standard error [SE] = 0.009, p < 0.01; γ = 0.083, SE = 0.023, p < 0.01; γ = 0.093, SE = 0.019, p < 0.01).
Discussion
On a methodological standpoint, the study of daily functioning in the elderly is complex and often hindered by problems associated with recalling events or feelings, and fatigability. In recent years, the use of computerized ambulatory techniques such as EMA has greatly increased and offers a true improvement in the way in which daily functioning is investigated. These techniques have been used in a variety of populations including individuals with serious psychiatric disorders. However, the validity of these methods in older populations remains unclear (Cain et al., 2009). The objective of the present study was to examine this important question in elderly persons with or without cognitive impairment and their spouses.
In light of the difficulty associated with the specificity of recruitment of our sample, we can consider that acceptance rates in both groups are acceptable. First, low participation rates may be attributed to the inclusion of elderly participants drawn from the general population and in rural settings. This general population sample is likely to be unfamiliar with such research protocols. Second, participation was considered when both spouses agreed to enroll, which considerably impacted participation rates. Moreover, in accordance with previous research on study participation (Jacomb et al., 2002), significant differences between participants and non‐participants with regard to education level and general cognitive functioning were observed.
Compliance rates were also generally good considering the data collection technique was through landlines for both participants and spouses, as well as for those with cognitive impairment though at a lower rate.
Finally, taken together, acceptance and compliance levels indicate that ambulatory methods seem adapted to this population. Landlines appeared more familiar in the present rural elderly population in that this technique did not modify their daily life habits. Moreover, the telephone method used in the present study seems not only to contribute to minimizing missing data (Claassen et al., 2009), but it also promotes the validity and the quality of data collection (Bouisson and Swendsen, 2003; Senior et al., 2007).
The validity of EMA in elderly populations is further supported by the present findings regarding fatigue and reactivity effects. First, as demonstrated in previous studies in younger populations (Johnson et al., 2009), the proportion of missing data does not increase with study duration suggesting no salient method‐induced fatigue effects. Second, as showed in populations with psychiatric disorders there was little evidence of reactivity effects (Hufford et al., 2002; Aaron et al., 2004; Freedman et al., 2006). Overall, the frequency of specific responses regarding physical and social environments, or specific behaviors did not vary as a function of study duration. Reactivity was also examined with responses to psychological states suggesting minimal reactivity effects whereby tiredness tended to decrease over time, especially in participants with cognitive impairment and their spouses. These results are counterintuitive as one may expect the burden of monitoring and multiple daily assessments to impact reactivity and possibly cause distress and tiredness (Schiffman et al., 2008). Previous EMA studies have also reported partial reactive effects (e.g. Hufford and Schiffman, 2002; Litt et al., 1998) but, as in our findings, those concerned only one or two variables and permitted the validity of the data collected to be considered. Indeed, no reactivity effects were observed with all other variables under consideration including specific environments, social contexts, activities, or well‐being suggesting that this method is suitable for use in elderly populations and to examine daily life activities and functioning. Finally, the present findings indicate that EMA procedures did not overburden elderly participants as demonstrated by the absence of increasing missing data (i.e. fatigue effect).
Several limitations should be acknowledged. The specificity of the inclusion and exclusion criteria may limit the generalizability of the present results. First, the retired farmers included in the sample may differ from the general population of elderly individuals on socio‐demographic characteristics, health status, or behaviors (Evans, 2009; Therrien and Desrosiers, 2010). Second, study acceptance was considered a conservative estimate in that both spouses had to participate in order to enroll in the study. Third, the sample size is relatively small and these findings require replication in a larger sample.
Taken together these results support the use of EMA not only in cognitively impaired individuals, but also in elderly couples. Further research may benefit from this methodology to investigate daily life psychological, behavioral, and clinical phenomena in elderly individuals and their partners.
Declaration of interest statement
The authors have no competing interest.
Acknowledgments
Participants were drawn from the AMI cohort conducted by Institut de Santé Publique d'Epidémiologie et de Développement (ISPED) and the University of Bordeaux 2. This manuscript was prepared in collaboration with the AMI study Steering Committee. The AMI study was supported by the AGRICA group (CAMARCA, CRCCA, CCPMA PREVOYANCE, CPCEA, AGRI PREVOYANCE), the Mutualité Sociale Agricole de Gironde and the Caisse Centrale de la Mutualité Sociale Agricole. The present study was also funded by the France Alzheimer association.
The authors are grateful to Marie Carrier, Audrey Dal Bo, Camille Delbary, Marlène Doussy, Aurore Hannedouche‐Reclus, Céline Indurain, Laure‐Amélie Laclau, Maïté Lanusse and Mailis Hegoburu, for their contribution to this investigation.
References
- Aaron L.A., Mancl L., Turner J.A., Sawchuk C.N., Klein K.M. (2004) Reasons for missing interviews in the daily electronic assessment of pain, mood, and stress. Pain, 109, 389–398, DOI: 10.1016/j.pain.2004.02.014 [DOI] [PubMed] [Google Scholar]
- Bäckman L., Wahlin A., Small B.J., Herlitz A., Winblad B., Fratiglioni L. (2004) Aging cognitive functioning in aging and dementia: the Kungsholmen Project. Aging, Neuropsychology, and Cognition, 11(2–3), 212–244. [Google Scholar]
- Bolger N., Davis A., Rafaeli E. (2003) Diary methods: capturing life as it is lived. Annual Review of Psychology, 54, 579–616, DOI: 10.1146/annurev.psych.54.101601.145030 [DOI] [PubMed] [Google Scholar]
- Bouisson J. (2002) Routinization preferences, anxiety and depression in an elderly French sample. Journal of Aging Studies, 16, 295–302. [Google Scholar]
- Bouisson J., Swendsen J. (2003) Routinization and emotional well‐being: an experience sampling investigation in an elderly French sample. Journal of Gerontology, Series B: Psychological Sciences and Social Sciences, 5, 280–282. [DOI] [PubMed] [Google Scholar]
- Brandstatter H. (1994) Well‐being and motivational person‐environment fit: a time‐sampling study of emotions. European Journal of Personality, 8, 75–93, DOI: 10.1002/per.2410080202 [DOI] [Google Scholar]
- Bressoux, P. (2010) Modélisations statistiques appliquées aux sciences sociales. Brussels: De Boeck supérieur. [Google Scholar]
- Cain A.E., Depp C.A., Jeste D.V. (2009) Ecological momentary assessment in aging research: a critical review. Journal of Psychiatric Research, 43, 987–996, DOI: 10.1016/j.jpsychires.2009.01.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Claassen C., Kurian B., Trivedu M., Grannemann B., Tuli E., Pipes R., Preston A., Flood A. (2009) Telephone‐based assessments to minimize missing data in longitudinal depression trials: a project IMPACTS study reports. Contemporary Clinical Trials, 30, 13–19, DOI: 10.1016/j.cct.2008.08.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Csikszentmihalyi M., Larson R. (1987) Validity and reliability of the Experience‐Sampling Method. Journal of Nervous and Mental Disease, 175(9), 526–536, DOI: 10.1097/00005053-198709000-00004 [DOI] [PubMed] [Google Scholar]
- Evans R.J. (2009) A comparison of rural and urban older adults in Iowa on specific markers of successful aging. Journal of Gerontological Social Work, 52, 423–438, DOI: 10.1080/01634370802609197 [DOI] [PubMed] [Google Scholar]
- Folstein M.F., Folstein S.E., McHugh P.R. (1975) Mini‐Mental State: a practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research, 12, 189–198. [DOI] [PubMed] [Google Scholar]
- Freedman M.J., Lester K.M., McNamara C., Milby J.B., Schumacher J.E. (2006) Cell phones for ecological momentary assessment with cocaine‐addicted homeless patients in treatment. Journal of Substance Abuse Treatment, 30, 105–111, DOI: 10.1016/j.jsat.2005.10.005 [DOI] [PubMed] [Google Scholar]
- Hektner J.M., Schmidt J.A., Csikszentmihalyi M. (2007) Experience Sampling Method: Measuring the Quality of Everyday Life, Thousand Oaks: CA, Sage Publications. [Google Scholar]
- Hufford M.R., Schiffman S.S. (2002) Methodological issues affecting the value of patient‐reported outcomes data. Expert Review of Pharmacoeconomics, 2, 119–128. [DOI] [PubMed] [Google Scholar]
- Hufford M.R., Shields A.L., Schiffman S., Paty J., Balabanis M. (2002) Reactivity to ecological momentary assessment: an example using undergraduate problem drinkers. Psychology of Addictive Behaviors, 16, 205–211, DOI: 10.1037/0893-164X.16.3.205 [DOI] [PubMed] [Google Scholar]
- Hurlburt R.T. (1997) Randomly sampling thinking in the natural environment. Journal of Consulting and Clinical Psychology, 65, 941–949, DOI: 10.1037/0022-006X.65.6.941 [DOI] [PubMed] [Google Scholar]
- Jacomb P., Jorm A., Korten A., Christensen H., Henderson A. (2002) Predictors of refusal to participate: a longitudinal health survey of the elderly in Australia. BMC Public Health, 2(4), DOI: 10.1186/1471-2458-2-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson E.I., Grondin O., Barrault M., Faytout M., Helbig S., Husky M., … Swendsen J. (2009) Computerized ambulatory monitoring in psychiatry: a multi‐site collaborative study of acceptability, compliance, and reactivity. International Journal of Methods in Psychiatric Research, 18(1), 48–57, DOI: 10.1002/mpr.276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kreft G.G. (1996) Are Multilevel Techniques Necessary? An Overview, Including Simulation Studies, Los Angeles, CA: California State University. [Google Scholar]
- Larson R., Almeida D. (1999) Emotional transmission in the daily lives of families: a new paradigm for studying family process. Journal of Marriage and Family, 61(1), 5–20. [Google Scholar]
- Litt M.D., Cooney N.L., Morse P. (1998) Ecological Momentary Assessment (EMA) with treated alcoholics: methodological problems and potential solutions. Health Psychology, 17, 48–52. [DOI] [PubMed] [Google Scholar]
- Moskowitz D.S., Young S.N. (2006) Ecological momentary assessment: what it is and why it is a method of the future in clinical psychopharmacology. Journal of Psychiatry and Neuroscience, 31(1), 13–20. [PMC free article] [PubMed] [Google Scholar]
- Namazi K., McClintic M. (2003) Computer use among elderly person in long‐term care facilities. Educational Gerontology, 29, 535–550. [Google Scholar]
- Ohly S., Sonnentag S., Niessen C., Zapf D. (2010) Diary studies in organizational research. An introduction and some practical recommendations. Journal of Personnel Psychology, 9(2), 79–93, DOI: 10.1027/1866-5888/a000009 [DOI] [Google Scholar]
- Pérès K., Matharan F., Allard M., Amieva H., Baldi I., Barberger‐Gateau P., … Dartigues J.F. (2012) Health and aging in elderly farmers: the AMI cohort. BMC Public Health, 12, 558, DOI: 10.1186/1471-2458-12-558 [DOI] [PMC free article] [PubMed] [Google Scholar]
- R Development Core Team . (2008) R: A Language and Environment for Statistical Computing, Vienna, R Foundation for Statistical Computing.
- Raudenbush S., Bryk A., Congdon R. (2005) HLM for Windows, version 6.03, Skokie, IL, Scientific Software International.
- Schiffman S., Stone A., Hufford M.R. (2008) Ecological momentary assessment. Annual Review of Clinical Psychology, 4, 1–32, DOI: 10.1146/annurev.clinpsy.3.022806.091415 [DOI] [PubMed] [Google Scholar]
- Scollon C.N., Kim‐Prieto C., Diener E. (2003) Experience sampling: promises and pitfalls, strengths and weakness. Journal of Happiness Studies, 4, 5–34. [Google Scholar]
- Senior A., Kunik M., Rhoades H., Novy D., Wilson N., Stanley M. (2007) Utility of telephone assessments in an older adult population. Psychology and Aging, 22(2), 392–397, DOI: 10.1037/0882-7974.22.2.392 [DOI] [PubMed] [Google Scholar]
- Therrien F.H., Desrosiers J. (2010) Participation of metropolitan, urban and rural community‐dwelling older adults. Archives of Gerontology and Geriatrics, 51, e52–e56, DOI: 10.1016/j.archger.2009.11.017 [DOI] [PubMed] [Google Scholar]


