Abstract
Background:
Early functional rehabilitation is frequently discussed in treating Achilles tendon rupture. A consistent definition of what constitutes early functional rehabilitation has not been established across the literature, despite studies supporting its efficacy. A standardized definition would be helpful to pool data across studies, allow for between-study comparisons, and ultimately work toward developing clinical guidelines.
Purpose:
To define early functional rehabilitation (including when it is initiated and what it entails) when used to treat Achilles tendon rupture and to identify outcome measures for evaluating the effect of treatment.
Study Design:
Systematic review; Level of evidence, 4.
Methods:
Ovid MEDLINE, EMBASE, PEDro, CINAHL, and Cochrane databases were searched for relevant studies. Eligibility criteria for selecting studies consisted of randomized controlled trials, cohort studies, and case series (≥10 participants) including weightbearing or exercise-based interventions within 8 weeks after Achilles tendon rupture.
Results:
A total of 174 studies published between 1979 and 2018 were included. Studies were rated a median (interquartile range [IQR]) of 17 (15-20) on the Downs & Black checklist and included 9098 participants. Early functional rehabilitation incorporated weightbearing (95%), range of motion (73%), and isometric/strengthening exercises (50%). Weightbearing was initiated within the first week, whereas exercise (eg, ankle range of motion, strengthening, whole-body conditioning) was initiated in the second week. Initiation of exercises varied based on whether treatment was nonsurgical (mean, 3.0 weeks; IQR, 2.0-4.0 weeks) or simple (mean, 2.0 weeks; IQR, 0.0-2.3 weeks) or augmented surgical repair (mean, 0.5 weeks; IQR, 0.0-2.8 weeks) (P = .017). Functional outcomes including ankle range of motion (n = 84) and strength (n = 76) were reported in 130 studies. Other outcome domains included patient-reported outcomes (n = 89), survey-based functional outcomes (n = 50), and tendon properties (n = 53).
Conclusion:
Early functional rehabilitation includes weightbearing and a variety of exercise-based interventions initiated within the first 2 weeks after acute Achilles tendon rupture/repair. Because early functional rehabilitation has lacked a standardized definition, interventions and outcome measures are highly variable, and pooling data across studies should be done with attention paid to what was included in the intervention and how treatment was assessed.
Keywords: Achilles, mobilization, weightbearing, ankle, outcomes
The yearly incidence of Achilles tendon rupture is up to 37 per 100,000 individuals.61,105,160 There is ongoing debate regarding optimal treatment, as attention has shifted away from outcomes such as rerupture rates and toward function-based outcomes.74 Plantar flexor weakness22,72,103 and biomechanical asymmetries with running and jumping activities23,200 persist in the long term. These may limit performance capacity or predispose these individuals to other orthopaedic conditions such as patellofemoral joint pain.200 It is important that patients recover within the first year after injury, as 1-year outcomes predict whether individuals will be left with long-term disabilities.23,69
Early functional rehabilitation has become a buzz phrase in treating Achilles tendon rupture. A consistent definition of what constitutes early functional rehabilitation has not been established across the literature, despite studies identifying that early functional rehabilitation was safe, resulted in higher patient satisfaction, improved function, and led to faster return to work and sport in some instances.24,67,99,117,193 Systematic reviews have supported the use of early functional rehabilitation to optimize patient outcomes regardless of whether a participant is managed nonsurgically55 or surgically.21,24,78,128 A standardized definition would be helpful to pool data across studies, allow for between-study comparison, and ultimately work toward developing clinical guidelines.
The components in defining early functional rehabilitation include establishing what types of treatment recommendations comprise early functional rehabilitation and when they are initiated. Prior systematic reviews investigating the efficacy of early functional rehabilitation21,24,55,78,128 have provided limited guidance as to the working definition of this term, relying on author-delineated, inconsistent definitions of early. For example, Brumann et al24 limited studies to those including weightbearing or ankle mobilization in the first 3 weeks, McCormack and Bovard128 included only studies that included any type of rehabilitation by 2 weeks, and El-Akkawi et al55 limited study inclusion to those that initiated rehabilitation by 4 weeks. Variations between systematic review–level evidence point to the lack of uniform definition of early functional rehabilitation.
The standardization of outcomes used to assess patient response to intervention is another critical piece in understanding the effectiveness of early functional rehabilitation. As part of the Core Outcome Measures in Effectiveness Trials (COMET) Initiative, core outcome sets are being developed and applied in an effort to improve direct comparisons across studies.198 This is in response to the challenge of pooling literature with large variability in reported outcomes13 as well as substantial problems with missing data for primary outcomes.198 A first step in the development of a core outcome set is to identify the outcome measures used in clinical trials. A core outcome set is being discussed for Achilles tendinopathy114,176; however, to date, an Achilles tendon rupture–specific set has not been initiated in the literature.
The purpose of this study was to comprehensively define early functional rehabilitation in terms of what types of interventions are delivered to patients with Achilles tendon rupture and when. We hypothesized that treatment was initiated earlier in more recent studies, so we investigated changes in trends of early functional rehabilitation onset over time. Secondarily, we sought to identify the outcome measures that have been used to assess patient response to these rehabilitative protocols as a first step in identifying a core outcome set for this patient population.
Methods
This study was a systematic review of the literature on early functional rehabilitation for Achilles tendon rupture. The study was performed according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines and was registered on the Prospero database (registration ID: CRD42017062300). Due to the size of the study, we are reporting results for the definition of early functional rehabilitation portion of the Prospero protocol, and work regarding specific rehabilitation protocols is ongoing. The search was completed on May 9, 2018.
Search Strategy
The search strategy was based on the PICO (Patient, Intervention, Comparator, and Outcome) model. Development of the search string and conduct of the search were done with the assistance of a research librarian. The complete search string is included in Appendix Table A1. Databases included in the search were Ovid MEDLINE, EMBASE, PEDro, CINAHL, and the Cochrane Database.
Study Inclusion and Exclusion
For the purposes of this review, we broadly defined early functional rehabilitation as having weightbearing and/or ankle-focused exercises beginning within the first 8 weeks and while the patient is still using an immobilization device (ie, orthosis, cast, specialized treatment boot). In the event that no immobilization device was used during the course of treatment, early functional rehabilitation was defined as weightbearing and exercises started within the first 8 weeks after injury or surgery.
Included studies needed to involve patients at least 18 years of age treated with early functional rehabilitation after acute (defined as treated within 2 weeks) Achilles tendon rupture. Studies needed to be randomized controlled trials (RCTs), cohort studies, or case series with a minimum of 10 participants. Narrative reviews, systematic reviews and meta-analyses, and case studies were excluded. Studies were excluded if participants with diabetes, neurological conditions, or only chronic or delayed treatment were included. In studies including participants with acute and delayed ruptures, only data pertaining to the acute rupture group were included in the review. Due to the limitations of languages spoken by the investigatory team and access to translators, only studies in English, Danish, Swedish, Norwegian, German, French, Spanish, or Portuguese were included.
Data Extraction: Defining Early Functional Rehabilitation
Study inclusion and exclusion were determined by 2 independent reviewers (J.A.Z., M.C.) using Covidence systematic review software (Veritas Health Innovation) for citation management. In the event that consensus regarding inclusion could not be met, a third reviewer was consulted (K.G.S.). Data extraction was completed by 2 independent reviewers (J.A.Z., M.C.) using a REDCap database,70 with the exception of non-English studies. Disagreements between reviewers were resolved through discussion, and if consensus could not be met, a third reviewer was consulted (K.G.S.). For non-English studies, a single reviewer completed data extraction due to language comprehension constraints among the study team.
Data extraction included study design (RCT, cohort study, or case series), number of participants, treatment type (surgical, nonsurgical, or both), and, when applicable, surgery type (simple repair or augmented repair). Type of early functional rehabilitation was categorized as follows: weightbearing, range of motion (exercises or as allowed by an orthosis permitting some movement), strength exercise with resistance and progression, isometric exercise, cardiovascular-based exercise (eg, stationary bike), general and core strengthening, balance, and other. All rehabilitation strategies used during the first 8 weeks and while participants were still using some form of immobilization were included. Timing of exercise and weightbearing onset was recorded. In cases where 2 or more groups with different rehabilitative protocols were used, the content of these protocols was combined for the purposes of describing type of rehabilitation, and the earliest onset time across groups was recorded.
Methodological Quality Assessment
Studies were assessed for methodological quality through use of the modified Downs & Black79,98,145 checklist, in which 26 or above indicates excellent, 20-25 good, 15-19 fair, and 14 or less poor quality. Studies in English were scored by 2 independent reviewers. If there were inconsistencies in reviewer response, a third reviewer (J.A.Z. or M.C. ) was consulted. Similar to data extraction, non–English language studies were scored by a single reviewer.
Data Extraction: Outcome Measures Data
Outcome measures used in each study were noted and subgrouped by domain (patient-reported outcome, survey-based functional outcome, functional outcome, and tendon properties). Time of outcomes assessment was recorded as 0-3 months, 4-6 months, 7-12 months, >1-5 years, and >5 years. All time points were extracted. If a study did not have predetermined time points for assessment, the mean or median time of assessment was recorded.
In cases where 2 or more studies analyzed the same group of participants, the studies were combined for the purposes of extracting outcome types and timing of outcomes assessment, and the primary study was used for total number of participants, rehabilitation strategy, and quality assessment. This was done to maximize the number of outcomes reported while not artificially inflating participant numbers.
Data Analysis
Data failed the assumptions of parametric statistics based on the Shapiro-Wilk test, so nonparametric tests were used for analysis. Descriptive statistics used are frequencies, medians, and interquartile ranges (IQRs). To better understand the types of studies included in this review, the relationship of study publication year and study quality was assessed by Spearman correlation.
To investigate timing of early functional rehabilitation, the onset of weightbearing and exercise (in weeks, with 0 indicating days 0-6, 1 indicating days 7-13, etc) is reported as frequencies of studies using a given start time. Time of weightbearing and exercise onset was also investigated by treatment intervention subgroup (nonsurgical, simple repair, or augmented repair), and differences in time of onset were compared between groups through use of an independent-samples Kruskal-Wallis test. Studies investigating only 1 type of treatment were included in the subgroup analysis. This is because it is possible that information from both treatment groups would have been listed together in studies comparing 2 different initial treatment strategies.
To identify changes in early functional rehabilitation over time, time of weightbearing and exercise onset was compared with publication year by use of Spearman correlation. Because not all studies included in the review were included in the individual analyses (eg, a study involving only early exercise would not be included in the weightbearing analyses), for each analysis the total number of primary studies included along with their median Downs & Black checklist score is reported.
Results
Search Results and Study Inclusion
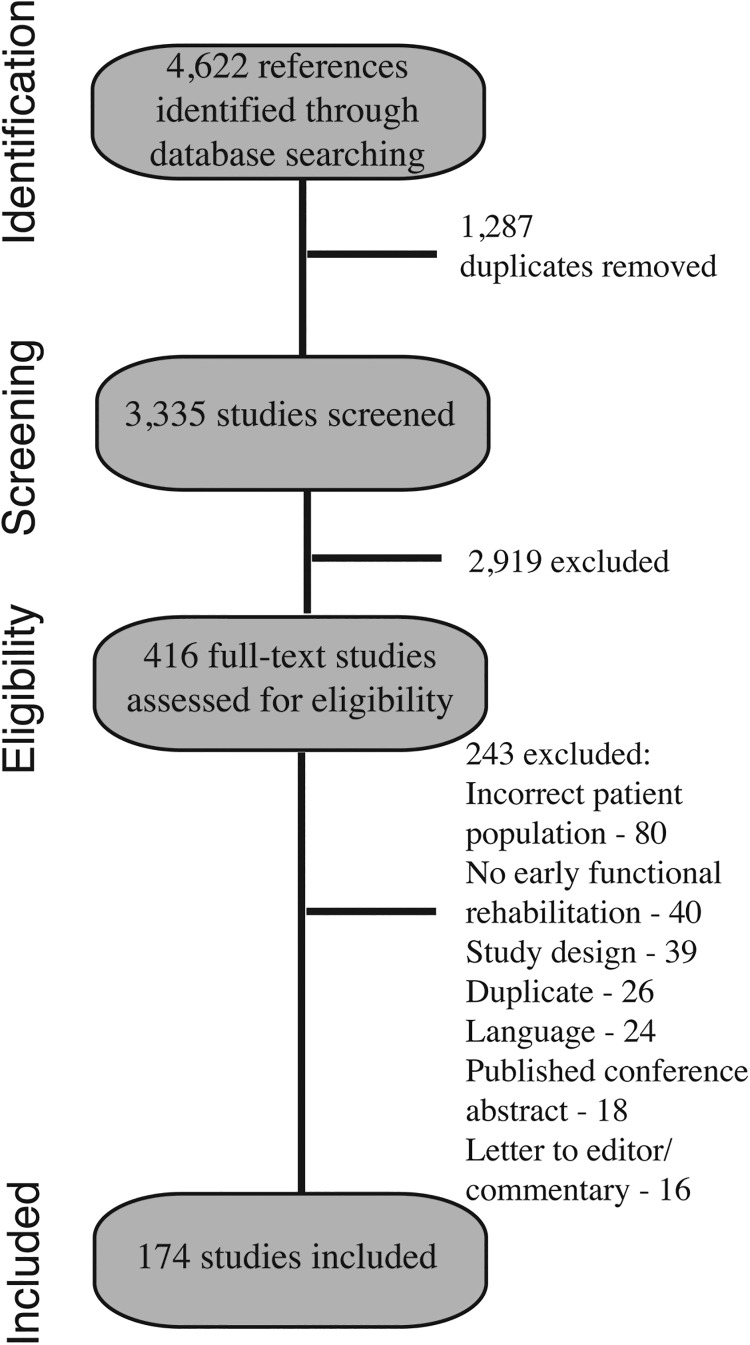
The results of the search and study inclusion are shown in Figure 1. Of the 174 included studies, 157 studies# were found to be primary studies, and 17 studies** were found to have overlapping populations and were included only in the reporting of additional outcomes and outcome assessment timeframes. We included 16 non-English studies: 12 in German, 2 in Portuguese, 1 in Danish, and 1 in Spanish (see Appendix Tables A2 and A3).
Figure 1.
Search results and study inclusion-exclusion flowchart.
Descriptive Analysis of Included Studies
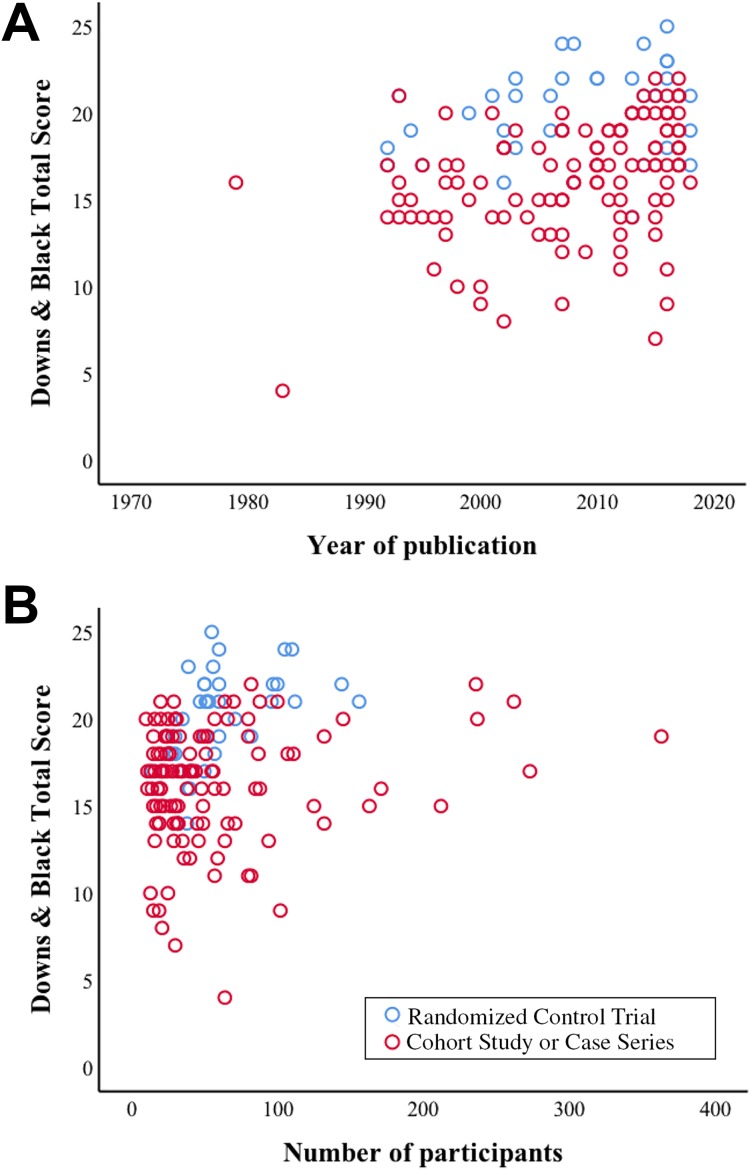
Included primary studies were published between 1979 and 2018 (median [IQR], 2010 [2002-2015]), consisting of 38 RCTs and 119 cohort studies or case series. Studies rated a median [IQR] (range) of 17 [15-20] (4-25) on the Downs & Black checklist for quality assessment (see Appendix Table A2).
Included studies had a median [IQR] (range) of 40 [25-66] (10-363) participants, with a total of 9098 participants included in this systematic review. The included RCTs contained significantly more participants versus the cohort studies (median [IQR], range: RCTs, 52 [39-74], 14-156; cohort/case series, 35 [22-66], 10-363; P = .011) (Figure 2). Participants were managed surgically in 112 studies and nonsurgically in 20 studies (see Appendix Tables A2 and A3). A total of 24 studies included both surgical and nonsurgical groups, and 1 study had treatment described as “other” (open fibrin gluing without end-to-end repair). Surgery type was a simple repair in 114 studies and augmented repair in 33 studies.
Figure 2.
(A) Year of publication positively relates to study quality. (B) Distribution of number of participants to study quality by study design.
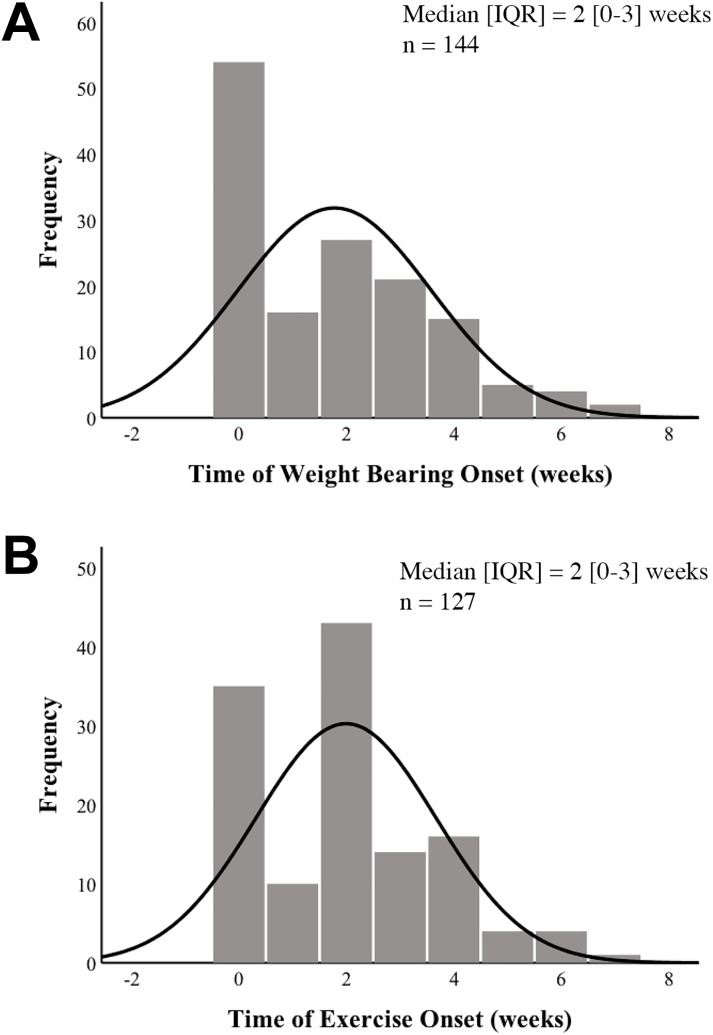
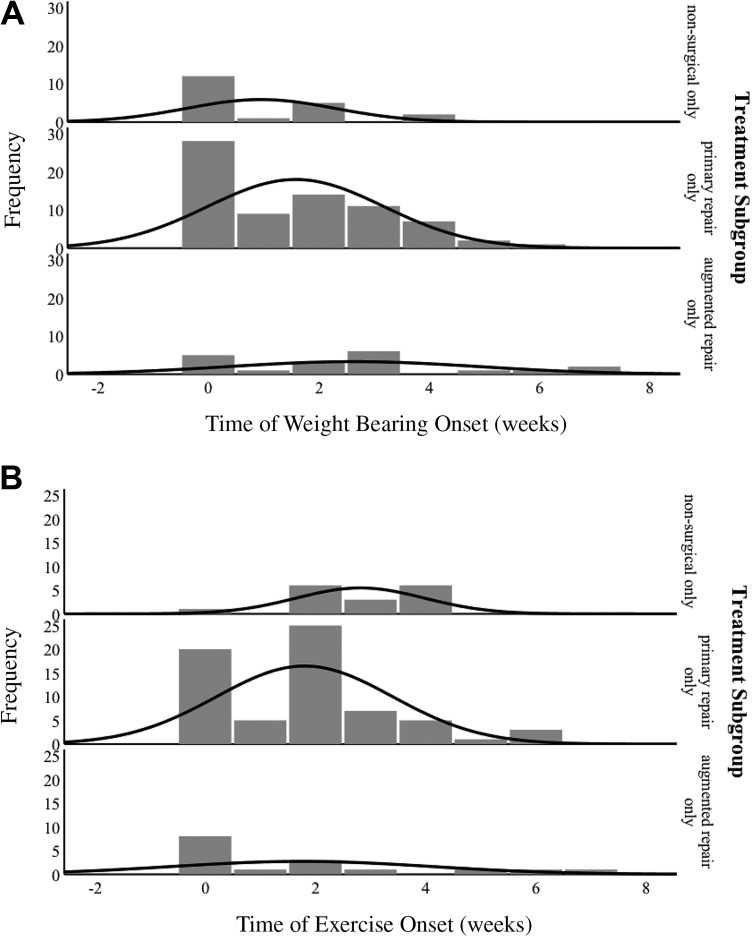
Onset of weightbearing was a median [IQR] of 2 weeks [0-3 weeks] after injury (Figure 3). Onset of exercise was a median (IQR) of 2 weeks (0-3 weeks) after injury (Figure 3).
Figure 3.
(A) Timing of weightbearing onset in entire group. (B) Timing of exercise onset in entire group.
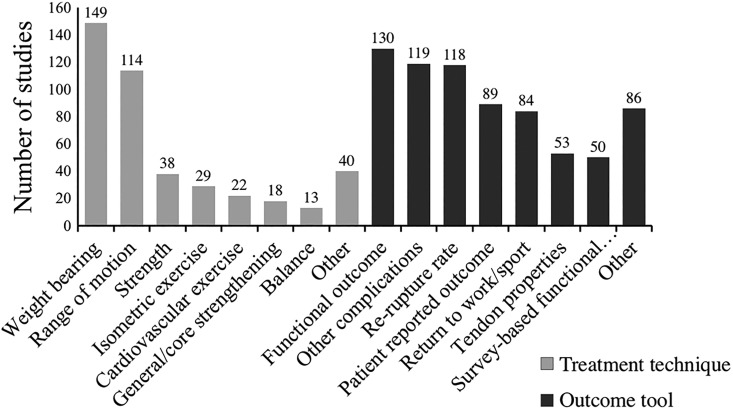
Type of Early Functional Rehabilitation
Type of early functional rehabilitation is depicted in Figure 4. Interventions that were categorized as “other” (number of studies in parentheses) included massage (8), stretching (8), proprioception (8), electrical stimulation (5), cryotherapy (4), coordination (3), aqua therapy (3), proprioceptive neuromuscular facilitation (2), joint mobilization (1), ankle self-mobilization (1), neuromuscular exercise (1), night splint (1), and laser (1).
Figure 4.
Type of early functional rehabilitation and outcome measures used.
Descriptive Analysis of Early Functional Rehabilitation Onset by Treatment Subgroup
Distribution of the timing of weightbearing onset was not significantly different between groups (median [IQR] nonsurgical, 0.0 [0.0-2.0]; simple surgical, 1.0 [0.0-3.0]; augmented surgical, 2.5 [0.0-3.0] weeks; P = .060) (Figure 5). Distribution of the timing of exercise onset was significantly different between groups (median [IQR] nonsurgical, 3.0 [2.0-4.0]; simple surgical, 2.0 [0.0-2.3]; augmented surgical, 0.5 [0.0-2.8 weeks]; P = .017) (Figure 5).
Figure 5.
Timing of (A) weightbearing and (B) exercise onset in nonsurgically and surgically managed (primary and augmented repair) patients.
No differences were found in year of publication (P = .530) or study quality (P = .148) between studies based on initial intervention (nonsurgery, primary repair, or augmented repair) (nonsurgery: n = 20, median [IQR] year of publication = 2008 [1998-2016], study quality = 17 [14-20]; primary repair: n = 82, year of publication = 2011 [2003-2015], study quality = 17 [15-19]; augmented repair: n = 20, year of publication = 2007 [2001-2012], study quality = 15 [13-18]).
Change in Study Quality Over Time
Study quality improved with year of publication (r sp = 0.33; P < .001) (Figure 2). In studies where exercise was initiated within the first 8 weeks (n = 127) (Downs & Black checklist score median [IQR], 17 [15-20]), time of exercise onset significantly increased with year of publication (r sp = 0.198; P = .026) but was not significantly related to study quality (r sp = –0.016; P = .862). In studies where weightbearing was initiated within the first 8 weeks (n = 144, Downs & Black checklist score median [IQR], 18 [15-20]), time of weightbearing onset was not significantly related to year of publication (r sp = –0.079; P = .344) or study quality (r sp = 0.047; P = .572).
Outcome Measures
Common outcome measures are shown in Figure 4 and Table 1. General outcomes categorized as “other” (number of studies in parentheses) in multiple studies included satisfaction (40), pain (29), time to a selected milestone (12), metrics regarding hospital stay or length (9), operative time (8), number of office or physical therapy visits (5), footwear restrictions (5), cost (4), Thompson/Matles test (4), Achilles tendon resting angle (3), Hannover scale (3), Boyden scale (3), aesthetics of surgical site (4), scale devised by the authors (2), Achilles tendon repair score (2), and pain medication use (2). A total of 4 studies included general “other” outcomes that were not used in any other study.
TABLE 1.
Outcome Measures Useda
| Outcome Measure | No. of Studies |
|---|---|
| Patient-reported outcome (total) | 89 |
| Achilles tendon Total Rupture Score | 27 |
| Foot and Ankle Outcome Score | 3 |
| No information provided | 1 |
| Other patient-reported outcome | 43 |
| Survey-based functional outcome (total) | 50 |
| AOFAS | 33 |
| Leppilahti score | 12 |
| Thermann score | 12 |
| Functional outcome (total) | 130 |
| Ankle range of motion | 84 |
| Strength | 76 |
| Calf circumference | 69 |
| Heel-rise | 56 |
| Biomechanics/gait analysis | 21 |
| Other | 39 |
| Tendon properties (total) | 53 |
| Morphology | 43 |
| Biology (cellular studies) | 1 |
| Other | 32 |
aAOFAS, American Orthopedic Foot and Ankle Score.
For the patient-reported outcomes domain, outcomes categorized as “other” in multiple studies included self-rating of specified functional activity (8), Victorian Institute of Sport Assessment – Achilles questionnaire (VISA-A) (6), EuroQol-5D (4), RAND 36-Item Health Survey (RAND-36) (3), Grimby Physical Activity Scale (4), Tegner Scale (3), Functional Index for Lower Leg (2), and 12-Item Short Form Health Survey (SF-12) (2). There were 9 studies that included outcomes not used by any other study.
For the functional outcomes domain, outcomes categorized as “other” in multiple studies included jump or hop testing (15), heel-toe walking (12), ankle circumference (4), pedobarography (3), ankle passive stiffness (3), muscle activity or electromyography (3), single-legged balance (3), and quadriceps circumference (2). For tendon-level outcomes, 2 studies reported other outcomes not used in any other study. Tendon-level outcomes categorized as “other” in multiple studies included tendon appearance on ultrasonography (11), tendon appearance on magnetic resonance imaging (7), tendon mechanical properties (7), gap distance (4), tendon adhesions (4), and muscle appearance on diagnostic imaging (3). We found that 7 studies reported outcomes that were not used in any other study.
Study outcomes were assessed between 0 and 3 months in 52 studies, between 4 and 6 months in 58 studies, between 7 and 12 months in 60 studies, between 1 and 5 years in 75 studies, and longer than 5 years in 8 studies (see Appendix Table A3).
Discussion
This systematic review is the first to comprehensively evaluate the available literature to define early functional rehabilitation after Achilles tendon rupture with regard to type and timing of rehabilitative treatment. Early functional rehabilitation in the treatment of Achilles tendon rupture is commonly used (>150 publications) but still lacks a consistent definition. Lack of standardization of content and timing when this intervention is initiated hampers evidence synthesis and implementation into clinical practice. Based on our comprehensive overview of the available literature, we define early functional rehabilitation as starting in the first 2 weeks after an acute Achilles tendon rupture. Such rehabilitation consists of a variety of weightbearing and exercise-based interventions.
Early functional rehabilitation tends to begin within the first 2 weeks after injury or surgery; however, there are subtleties in timing of weightbearing and exercise components based on initial treatment strategy (Figure 3). After surgical repair, both weightbearing and exercises tend to begin simultaneously—either immediately or 2 weeks after surgical repair. With nonsurgical management, the tendency is to initiate weightbearing immediately but delay initiation of exercise. Differences in trends of exercise onset between surgically and nonsurgically managed participants may result from clinical decision making aimed at approximating the tendon ends37 and avoiding complications29,49 while simultaneously providing enough tensile load to promote tendon healing.59,174
Early functional rehabilitation protocols incorporated a variety of different exercise-based intervention. Ankle range of motion was the most commonly included intervention. The goal of range of motion is likely to assist in tendon gliding and to prevent deep adhesion. In the context of this study, range of motion included both traditional ankle range of motion outside of the orthosis and use of a hinged orthosis. After ankle range of motion, strengthening was the next most common intervention. Despite mechanistic studies supporting the role of gradual tensile loading in order to promote tendon recovery,6,59,174 only 52% (66/127) of studies with exercise-based interventions included isometric or other strengthening exercise. Less frequently did exercise interventions address more holistic concerns such as cardiovascular and global strengthening.
Timing of rehabilitation onset did not decrease relative to study year as we had hypothesized. Exercises were started later in more recent studies, and no relationship was observed between publication year and weightbearing onset. These findings could be explained by our inclusion criteria. A higher number of studies from more recent years were included, which may reflect more studies initiating rehabilitation within the first 8 weeks and when participants were still using an orthosis. Studies published less recently may have been excluded, skewing relationships between publication year and timing of rehabilitation onset.
A variety of outcome measures are used to assess patient response to treatment after Achilles tendon rupture. Broadly, these measures can be described in 2 groups: population-specific outcomes and general outcomes. Specific to this patient population, a variety of functional measures are commonly used along with tendon morphology and diagnosis-specific outcome measures, such as the Achilles tendon Total Rupture Score (ATRS). When looking at general outcomes, the American Orthopedic Foot and Ankle Score (AOFAS) was used in several studies as were numerous other patient-reported outcomes, such as patient satisfaction. From a research standpoint, it would be beneficial to develop a core outcome set that uses a combination of general and population-specific measures to allow comparison between populations of individuals with varying diagnoses as well as measures that more comprehensively assess the concerns of this particular patient population. The data from this study can be used as a first step in developing a core outcome set, as we have compiled frequencies of commonly used outcomes across multiple domains of patient assessment.
The available literature poses a variety of challenges regarding early functional rehabilitation after Achilles tendon rupture. Looking across the included literature, we find that studies are primarily cohort studies or case series. Although RCTs had significantly more participants on average, 73% of studies presenting data from 100 or more individuals were case series or cohort studies. The majority of research has been done on individuals undergoing simple surgical repair (73% of studies), whereas 28% of studies investigated individuals managed nonsurgically. It seems that little research is available on rehabilitative strategies for nonsurgically managed individuals, which is potentially concerning given trends of increasing numbers of patients managed without surgery.61,177,178 Moving forward, it seems that tensile loading could be an area for rehabilitation protocol improvement. We found that only 1 in 2 studies included tensile-type loading, which has been suggested in basic science and mechanistic studies6,7,59,174 to be of importance in the recovery of this patient population. Additionally, a variety of orthoses are used in immobilizing patients—casts, unhinged walking boots with wedging, hinged walking boots—and the effect of these devices on tendon healing from a mechanistic standpoint is not well-described, with 1 study comparing foot position between strategies.56 The area of early functional rehabilitation continues to have great research potential, but standardizing outcomes and clearly stating rehabilitative protocols should be a focus moving forward.
Studies aimed at improving Achilles tendon rupture outcomes have used early functional rehabilitation, but this term has been applied without a well-established definition. Without a standardized definition, caution should be used when comparing outcomes between studies or pooling data from multiple studies, as the intervention could be very different even if treatment is labeled “early functional rehabilitation.” This study was intended to describe trends across the literature regarding type and timing of early rehabilitation to synthesize an explicit definition. Therefore, the results of this study cannot be taken in a prescriptive sense, because efficacy of treatment protocols was not assessed. We intentionally took a broad approach to study inclusion, and it is important to consider that the Downs & Black checklist can substantially favor RCTs over even very large cohort studies and case series.
Clinically, the findings of this systematic review suggest that in most cases, early functional rehabilitation begins within the first 2 weeks after treatment initiation in individuals with Achilles tendon rupture. Weightbearing and range of motion are commonly used intervention strategies; however, a growing body of literature is using additional rehabilitative strategies such as strengthening interventions and general conditioning. Although general foot and ankle functional scores are regularly reported, several outcomes more specific to this patient population could be considered to assess patient response to treatment.
Acknowledgment
The authors thank Tyler Tice and Jordan Denesik for their assistance in scoring studies for risk of bias assessment and Anne Thielecke, Camilla Rams Rathleff, Barbara C. Brocki, Kathryn Wiser, and Susan Wiser for translation of foreign studies.
Appendix
Table A1.
Search String
|
|
Table A2.
Summary of Interventions in All Included Studiesa
| First Author (Year) | Secondary Study? | No. of Patients | Weightbearing | ROM | Strength | Isometric Exercise | Cardiovascular Exercise | General Strength | Balance | Other | Quality Score |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Nonsurgical Management | |||||||||||
| Aujla12 (2018) | No | 236 | * | * | 22 | ||||||
| Aujla11 (2016) | No | 88 | * | * | 21 | ||||||
| Barfod14 (2014) | Yes | 60 | * | * | 24 | ||||||
| Dolphin48 (2016) | No | 25 | * | * | 20 | ||||||
| Ecker54 (2016) | No | 171 | * | * | * | * | * | 16 | |||
| Hüfner81 (2006) | No | 125 | * | * | * | * | * | 15 | |||
| Hüfner80 (2002) | No | 21 | * | * | * | * | * | * | 8 | ||
| Kaniki89 (2014) | No | 145 | * | * | * | * | * | * | 20 | ||
| Korkmaz99 (2015) | No | 47 | * | 21 | |||||||
| McComis127 (1997) | No | 30 | * | * | * | * | 20 | ||||
| McNair129 (2013) | No | 38 | * | 14 | |||||||
| Neumayer143 (2010) | No | 57 | * | * | * | * | 16 | ||||
| Persson155 (1979) | No | 20 | * | 16 | |||||||
| Petersen156 (2002)b | No | 50 | * | 19 | |||||||
| Reilmann161 (1996)c | No | 132 | * | * | * | * | 14 | ||||
| Roberts166 (2001) | No | 49 | * | * | 14 | ||||||
| Saleh168 (1992) | No | 40 | * | * | * | * | 17 | ||||
| Swennergren185 (2017) | No | 28 | * | * | 19 | ||||||
| Vavra- Hadziahmetovic194 (2000) | No | 19 | * | * | * | * | * | * | 9 | ||
| Walz195 (1993)c | No | 22 | * | * | 15 | ||||||
| Surgical Management | |||||||||||
| Agres1 (2018) | No | 14 | * | * | * | * | * | 17 | |||
| Aisaiding2 (2018) | No | 52 | * | * | * | * | * | 21 | |||
| Aktas3 (2007) | No | 30 | * | * | 19 | ||||||
| Al-Mouazzen4 (2015) | No | 30 | * | * | * | 15 | |||||
| Alviti5 (2017) | No | 20 | * | * | * | 20 | |||||
| Aoki8 (1998) | No | 22 | * | * | * | 17 | |||||
| Aspenberg9 (2015) | No | 16 | * | * | 13 | ||||||
| Assal10 (2002) | No | 87 | * | * | * | * | 18 | ||||
| Baumfeld16 (2019) | No | 38 | * | 16 | |||||||
| Bevoni17 (2014) | No | 66 | * | * | * | * | * | 20 | |||
| Bhattacharyya18 (2009) | Yes | 59 | * | * | 12 | ||||||
| Buchgraber25 (1997) | No | 48 | * | * | * | * | * | 16 | |||
| Calder26 (2005) | No | 46 | * | 13 | |||||||
| Carmont27 (2015) | No | 26 | * | * | * | 18 | |||||
| Carmont28 (2017) | No | 70 | * | * | 21 | ||||||
| Ceccarelli30 (2007) | No | 24 | * | * | * | * | 19 | ||||
| Cetti32 (1994) | No | 60 | * | * | * | 19 | |||||
| Chandrakant33 (2012) | No | 52 | * | * | * | * | * | 19 | |||
| Chen34 (2015) | No | 82 | * | * | 22 | ||||||
| Chiu35 (2013) | No | 19 | * | 14 | |||||||
| Chmielnicki36 (2016)c | No | 212 | * | 15 | |||||||
| Costa39 (2003) | No | 28 | * | * | 18 | ||||||
| Čretnik41 (2004) | Yes | 237 | * | * | * | 20 | |||||
| De Carli42 (2016) | No | 30 | * | * | 20 | ||||||
| De la Fuente43 (2016) | No | 39 | * | * | * | 23 | |||||
| De la Fuente44 (2016) | No | 26 | * | * | * | * | 18 | ||||
| Delgado-Brambila45 (2012)d | No | 35 | * | * | 13 | ||||||
| Ding46 (2012) | Yes | 88 | * | 16 | |||||||
| Don50 (2007) | No | 49 | * | * | 15 | ||||||
| Doral51 (2013) | No | 32 | * | * | * | * | 17 | ||||
| Dos Santos Gomes52 (1998)e | No | 13 | * | * | * | * | 10 | ||||
| Fernández-Fairén57 (1997) | No | 29 | * | * | * | * | * | 13 | |||
| Fitzgibbons58 (1993) | No | 14 | * | 16 | |||||||
| Gaiani60 (2012) | No | 80 | * | * | 11 | ||||||
| Garrido62 (2010) | No | 18 | * | * | 16 | ||||||
| Geremia63 (2015) | No | 18 | * | * | * | * | * | 18 | |||
| Gigante64 (2008) | No | 40 | * | * | 16 | ||||||
| Gorschewsky65 (2004) | No | 66 | * | * | * | * | 14 | ||||
| Gorschewsky66 (1999) | No | 20 | * | * | * | 15 | |||||
| Groetelaers67 (2014) | No | 60 | * | * | 21 | ||||||
| Heikkinen72 (2016) | No | 55 | * | * | 25 | ||||||
| Henríquez73 (2012) | No | 32 | * | * | * | 14 | |||||
| Holmenschlager75 (2002)c | No | 45 | * | * | 14 | ||||||
| Horter76 (2007)c | No | 102 | * | * | 9 | ||||||
| Hrnack77 (2012) | No | 15 | * | * | 15 | ||||||
| Jacob84 (2007) | No | 36 | * | * | 12 | ||||||
| Jallageas85 (2013) | No | 31 | * | * | * | 20 | |||||
| Jielile86 (2012) | No | 107 | * | * | * | * | * | * | 18 | ||
| Kangas88 (2003) | Yes | 50 | * | * | * | 22 | |||||
| Karabinas91 (2014) | No | 34 | * | 17 | |||||||
| Kauranen92 (2002) | No | 30 | * | * | * | 18 | |||||
| Keller94 (2014) | No | 100 | * | 21 | |||||||
| Kerkhoffs95 (2002) | No | 39 | * | 16 | |||||||
| Kim96 (2017) | No | 56 | * | * | * | 17 | |||||
| Kuskucu100 (2005) | No | 32 | * | * | 15 | ||||||
| Lacoste101 (2012) | No | 33 | * | * | 19 | ||||||
| Lansdaal102 (2007) | No | 163 | * | * | 15 | ||||||
| Lapidus106 (2007) | No | 105 | * | 24 | |||||||
| Lee107 (2008) | No | 11 | * | 16 | |||||||
| Leppilahti108 (2000) | No | 85 | * | 16 | |||||||
| Li109 (2017) | No | 24 | * | * | 18 | ||||||
| Lonzarić112 (2017) | No | 262 | * | * | 21 | ||||||
| Maffulli116 (2010) | No | 35 | * | * | * | * | 17 | ||||
| Maffulli117 (2003) | Yes | 53 | * | * | * | 21 | |||||
| Maffulli119 (2001) | No | 16 | * | 20 | |||||||
| Majewski120 (2008) | No | 28 | * | * | 17 | ||||||
| Mandelbaum121 (1995) | No | 29 | * | * | * | * | 14 | ||||
| Marti122 (1983) | No | 64 | * | 4 | |||||||
| Martinelli123 (2000) | No | 30 | * | 7 | |||||||
| Mauch124 (2017)c | No | 42 | * | * | * | 17 | |||||
| Mavrodontidis125 (2015) | No | 11 | * | 17 | |||||||
| Mayer126 (2010)e | No | 24 | * | * | * | 17 | |||||
| Mezzarobba131 (2012) | No | 40 | * | * | 12 | ||||||
| Miyamoto133 (2017) | No | 44 | * | * | * | 17 | |||||
| Moberg134 (1992) | No | 17 | * | 14 | |||||||
| Mortensen139 (1992) | No | 57 | * | 18 | |||||||
| Mortensen138 (1999) | No | 71 | * | * | 20 | ||||||
| Motta140 (1997) | No | 71 | * | * | 14 | ||||||
| Mukundan141 (2010) | No | 21 | * | 17 | |||||||
| Mullaney142 (2006) | No | 20 | * | * | 17 | ||||||
| Ocguder146 (2011) | No | 41 | * | * | * | 17 | |||||
| Ozer151 (2016) | No | 23 | * | * | * | 19 | |||||
| Ozkan152 (2016) | No | 15 | * | * | 19 | ||||||
| Ozkaya153 (2009) | No | 25 | * | * | * | * | * | 19 | |||
| Peng154 (2017) | No | 15 | * | * | * | * | * | 18 | |||
| Porter157 (2014) | No | 40 | * | * | * | * | * | 17 | |||
| Porter158 (2015) | No | 51 | * | * | * | 21 | |||||
| Quagliarella159 (2010) | No | 51 | * | 18 | |||||||
| Richardson163 (2003) | No | 30 | * | * | * | * | 15 | ||||
| Rozis167 (2018) | No | 82 | * | * | * | * | 19 | ||||
| Sandberg169 (2015) | No | 31 | * | * | 14 | ||||||
| Saper170 (2016) | No | 82 | * | * | 11 | ||||||
| Saw171 (1993) | No | 19 | * | * | 14 | ||||||
| Saxena172 (2011) | No | 27 | * | * | * | 15 | |||||
| Schäfer173 (2002)c | No | 40 | * | 18 | |||||||
| Schepull174 (2013) | No | 35 | * | * | * | 20 | |||||
| Schepull175 (2007) | No | 10 | * | 20 | |||||||
| Solveborn179 (1994) | No | 17 | * | * | 15 | ||||||
| Sorrenti180 (2006) | No | 64 | * | * | * | * | 13 | ||||
| Speck181 (1998) | No | 20 | * | * | 16 | ||||||
| Steele182 (1993) | No | 20 | * | 21 | |||||||
| Strauss183 (2007) | No | 52 | * | * | 19 | ||||||
| Suchak184 (2008) | Yes | 110 | * | * | * | 24 | |||||
| Tarniţă186 (2016) | No | 15 | * | * | 9 | ||||||
| Tezeren187 (2006) | No | 24 | * | * | * | * | * | 19 | |||
| Troop190 (1995) | No | 13 | * | * | 17 | ||||||
| Vadalá192 (2012) | No | 80 | * | 19 | |||||||
| Valkering193 (2017) | No | 56 | * | * | 23 | ||||||
| Wredmark201 (1992) | No | 34 | * | 17 | |||||||
| Yotsumoto202 (2010) | No | 20 | * | * | * | 18 | |||||
| Zayni203 (2017) | No | 29 | * | * | 21 | ||||||
| Zell204 (2000) | No | 25 | * | * | * | 10 | |||||
| Both Nonsurgical and Surgical Management | |||||||||||
| Cetti31 (1993) | No | 156 | * | 21 | |||||||
| Costa38 (2006) | No | 96 | * | 21 | |||||||
| Ebinesan53 (2008) | No | 63 | * | * | * | * | 16 | ||||
| Gwynne-Jones68 (2011) | No | 363 | * | * | * | * | 19 | ||||
| Hutchison82 (2015) | No | 273 | * | * | * | 17 | |||||
| Jackson83 (2013) | No | 80 | * | * | 20 | ||||||
| Karaaslan90 (2016) | No | 16 | * | 17 | |||||||
| Kearney93 (2011) | No | 49 | * | * | 19 | ||||||
| Lantto103 (2016) | Yes | 60 | * | * | 22 | ||||||
| Lill110 (1996)c | No | 57 | * | * | * | * | * | 11 | |||
| Lim111 (2018) | No | 132 | * | * | * | * | 19 | ||||
| Lorkowski113 (2007) | No | 94 | * | 13 | |||||||
| Maffulli115 (2017) | No | 26 | * | * | * | * | 18 | ||||
| Miller132 (2005) | No | 111 | * | 18 | |||||||
| Moller137 (2001) | Yes | 112 | * | * | 21 | ||||||
| Nilsson-Helander144 (2010) | Yes | 97 | * | * | 22 | ||||||
| Olsson150 (2013) | Yes | 100 | * | * | * | * | * | * | * | 22 | |
| Renninger162 (2016) | No | 57 | * | * | * | * | * | 20 | |||
| Richter164 (1994)c | No | 32 | * | 14 | |||||||
| Richter165 (1997)c | No | 55 | * | * | * | * | * | 17 | |||
| Thermann189 (1995)c | Yes | 50 | * | * | * | * | * | 17 | |||
| Twaddle191 (2007) | No | 50 | * | * | 22 | ||||||
| Weber196 (2003) | No | 47 | * | * | * | * | * | * | 19 | ||
| Willits199 (2010) | No | 144 | * | * | * | * | * | * | 22 | ||
| Knobe97 (2015) | No | 64 | * | * | 21 | ||||||
Table A3.
Summary of Outcomes in All Included Studies
| First Author (Year) | Outcome Type | Time of Outcome Assessment, mo | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Functional Outcome | Other Complications | Rerupture Rate | PROs | Return to Work/Sport | Tendon Properties | Survey- Based Functional Outcome | Other General Outcome (Description) | ||||||
| ≤3 | 4-6 | 7-12 | >1-5 | >5 | |||||||||
| Nonsurgical Management | |||||||||||||
| Aujla12 (2018) | * | * | * | * | |||||||||
| Aujla11 (2016) | * | * | * | * | |||||||||
| Barfod14 (2014) | * | * | * | * | Quality of life | * | * | ||||||
| Dolphin48 (2016) | * | * | * | * | |||||||||
| Ecker54 (2016) | * | * | * | * | * | * | * | Pain, satisfaction, meteosensitivity | * | ||||
| Hüfner81 (2006) | * | * | * | * | * | * | Pain | * | |||||
| Hüfner80 (2002) | * | * | * | ||||||||||
| Kaniki89 (2014) | * | * | * | * | * | * | |||||||
| Korkmaz99 (2015) | * | * | * | * | * | * | * | ||||||
| McComis127 (1997) | * | * | * | * | Cost of treatment | * | * | ||||||
| McNair129 (2013) | * | * | * | ||||||||||
| Neumayer143 (2010) | * | * | * | * | * | Satisfaction | * | * | * | ||||
| Persson155 (1979) | * | * | * | * | * | Satisfaction | * | ||||||
| Petersen156 (2002)b | * | * | * | * | * | ||||||||
| Reilmann161 (1996)c | * | * | * | * | * | Meteosensitivity, pain, shoewear problems | * | ||||||
| Roberts166 (2001) | * | * | * | * | * | ||||||||
| Saleh168 (1992) | * | * | * | * | Satisfaction | * | * | * | |||||
| Swennergren185 (2017) | * | Achilles tendon resting angle | * | * | |||||||||
| Vavra- Hadziahmetovic194 (2000) | * | * | * | * | * | Thompson, Simmond and Matles signs; pain | * | ||||||
| Walz195 (1993) | * | * | * | * | * | * | |||||||
| Surgical Management | |||||||||||||
| Agres1 (2018) | * | * | * | ||||||||||
| Aisaiding2 (2018) | * | * | * | * | * | * | * | * | * | ||||
| Aktas3 (2007) | * | * | * | * | * | * | Pain | * | |||||
| Al-Mouazzen4 (2015) | * | * | * | * | Satisfaction | * | * | * | |||||
| Alviti5 (2017) | * | ||||||||||||
| Aoki8 (1998) | * | * | * | Time from surgery to weightbearing/heel rising | * | * | |||||||
| Aspenberg9 (2015) | * | * | * | ||||||||||
| Assal10 (2002) | * | * | * | * | * | * | |||||||
| Baumfeld16 (2019) | * | * | * | * | * | Satisfaction | * | ||||||
| Bevoni17 (2014) | * | * | * | * | * | * | * | ||||||
| Bhattacharyya18 (2009) | * | * | Pain/stiffness, readmission to hospital, length of hospital stay, pain medication | * | * | * | |||||||
| Buchgraber25 (1997) | * | * | * | * | * | ||||||||
| Calder26 (2005) | * | * | * | * | * | * | * | * | |||||
| Carmont27 (2015) | * | * | * | * | Achilles tendon resting angle | * | * | * | |||||
| Carmont28 (2017) | * | * | * | Achilles tendon resting angle, calf squeeze test | * | * | * | ||||||
| Ceccarelli30 (2007) | * | * | * | * | * | ||||||||
| Cetti32 (1994) | * | * | * | * | * | Satisfaction | * | * | * | ||||
| Chandrakant33 (2012) | * | * | * | Time to plateau in improvement | * | ||||||||
| Chen34 (2015) | * | * | * | * | Operative time, scar length | * | * | ||||||
| Chiu35 (2013) | * | * | * | * | * | * | * | ||||||
| Chmielnicki36 (2016)c | * | * | * | ||||||||||
| Costa39 (2003) | * | * | * | * | * | * | * | ||||||
| Čretnik41 (2004) | * | * | * | * | * | * | Holz score, satisfaction | * | |||||
| De Carli42 (2016) | * | * | * | * | * | * | Pain | * | * | * | |||
| De la Fuente43 (2016) | * | * | * | * | Pain, pain medication | * | |||||||
| De la Fuente44 (2016) | * | * | * | * | * | * | |||||||
| Delgado-Brambila45 (2012)d | * | * | Number of physical therapy visits | * | |||||||||
| Ding46 (2012) | * | * | * | * | Scar length | * | |||||||
| Don50 (2007) | * | * | * | * | * | * | |||||||
| Doral51 (2013) | * | * | * | * | |||||||||
| Dos Santos Gomes52 (1998)e | * | * | * | Pain, edema in Achilles tendon area | * | ||||||||
| Fernández-Fairén57 (1997) | * | * | * | * | * | Stiffness | * | ||||||
| Fitzgibbons58 (1993) | * | * | * | * | * | ||||||||
| Gaiani60 (2012) | * | * | * | * | Satisfaction | ||||||||
| Garrido62 (2010) | * | * | * | * | * | * | Satisfaction | * | |||||
| Geremia63 (2015) | * | * | * | ||||||||||
| Gigante64 (2008) | * | * | * | * | * | Operative time | * | * | |||||
| Gorschewsky65 (2004) | * | * | * | * | Satisfaction | * | |||||||
| Gorschewsky66 (1999) | * | * | * | * | Length of hospitalization, operative time, time to full weightbearing, wound healing, satisfaction | * | |||||||
| Groetelaers67 (2014) | * | * | * | * | * | Satisfaction, Achilles tendon repair score | * | * | * | ||||
| Heikkinen72 (2016) | * | * | * | * | * | * | * | * | * | ||||
| Henríquez73 (2012) | * | * | * | * | Cosmesis, length of scar | * | |||||||
| Holmenschlager75 (2002)c | * | * | * | * | * | * | * | * | |||||
| Horter76 (2007)c | * | * | * | ||||||||||
| Hrnack77 (2012) | * | * | * | * | |||||||||
| Jacob84 (2007) | * | * | * | * | Pain, satisfaction | * | |||||||
| Jallageas85 (2013) | * | * | * | * | * | * | Number of physical therapy sessions, pain | * | |||||
| Jielile86 (2012) | * | * | * | * | * | * | * | * | * | ||||
| Kangas88 (2003) | * | * | * | * | * | * | * | * | * | ||||
| Karabinas91 (2014) | * | * | * | * | * | * | Satisfaction, wound healing, Thompson test | * | |||||
| Kauranen92 (2002) | * | * | Satisfaction | * | * | ||||||||
| Keller94 (2014) | * | * | * | * | * | * | Satisfaction | * | |||||
| Kerkhoffs95 (2002) | * | * | * | * | Length of hospital stay, satisfaction | * | |||||||
| Kim96 (2017) | * | * | * | * | Time until able to do single heel-raise | * | |||||||
| Kuskucu100 (2005) | * | * | * | * | * | * | * | * | |||||
| Lacoste101 (2012) | * | * | * | * | Socioeconomic and global satisfaction | * | * | ||||||
| Lansdaal102 (2007) | * | * | * | * | Operative time | * | |||||||
| Lapidus106 (2007) | * | * | * | ||||||||||
| Lee107 (2008) | * | * | * | * | * | * | Pain | * | * | * | * | ||
| Leppilahti108 (2000) | * | * | * | ||||||||||
| Li109 (2017) | * | * | * | * | * | * | Satisfaction, pain | * | * | ||||
| Lonzarić112 (2017) | * | * | * | * | Number of physical therapy/clinic sessions, duration of immobilization, duration of crutch use | * | * | ||||||
| Maffulli116 (2010) | * | * | * | * | * | Time to full weightbearing | * | ||||||
| Maffulli117 (2003) | * | * | * | * | * | * | Number of clinic/physical therapy sessions, Boyden scale, satisfaction, footwear restrictions, time to full weightbearing | * | |||||
| Maffulli119 (2001) | * | * | * | * | Boyden scale | * | |||||||
| Majewski120 (2008) | * | * | * | Hannover score, satisfaction | * | ||||||||
| Mandelbaum121 (1995) | * | * | * | * | * | * | * | ||||||
| Marti122 (1983) | * | * | * | * | * | ||||||||
| Martinelli123 (2000) | * | * | * | * | * | ||||||||
| Mauch124 (2017)c | * | * | |||||||||||
| Mavrodontidis125 (2015) | * | * | * | * | * | * | Pain, satisfaction | * | |||||
| Mayer126 (2010)e | * | * | |||||||||||
| Mezzarobba131 (2012) | * | * | * | ||||||||||
| Miyamoto133 (2017) | * | * | * | * | * | * | Time until able to perform heel-rises | * | * | * | |||
| Moberg134 (1992) | * | * | |||||||||||
| Mortensen139 (1992) | * | * | * | * | * | * | Satisfaction | * | * | ||||
| Mortensen138 (1999) | * | * | * | * | * | * | Whether they had physical therapy, pain, satisfaction | * | * | ||||
| Motta140 (1997) | * | * | * | * | * | Length of hospital stay | * | * | * | ||||
| Mukundan141 (2010) | * | * | * | * | * | ||||||||
| Mullaney142 (2006) | * | * | |||||||||||
| Ocguder146 (2011) | * | * | * | * | * | * | Operative time, pain | * | |||||
| Ozer151 (2016) | * | * | * | * | * | ||||||||
| Ozkan152 (2016) | * | * | * | * | |||||||||
| Ozkaya153 (2009) | * | * | * | * | * | * | |||||||
| Peng154 (2017) | * | * | * | * | |||||||||
| Porter157 (2014) | * | * | * | ||||||||||
| Porter158 (2015) | * | * | * | * | * | ||||||||
| Quagliarella159 (2010) | * | Hannover score | * | ||||||||||
| Richardson163 (2003) | * | * | * | * | * | * | Footwear restrictions, satisfaction, pain | * | |||||
| Rozis167 (2018) | * | * | * | * | * | * | * | ||||||
| Sandberg169 (2015) | * | * | * | * | |||||||||
| Saper170 (2016) | * | * | * | ||||||||||
| Saw171 (1993) | * | * | * | * | * | ||||||||
| Saxena172 (2011) | * | ||||||||||||
| Schäfer173 (2002)c | * | * | * | * | * | * | Length of time using crutches, special shoe and night splint | * | * | ||||
| Schepull174 (2013) | * | * | * | * | * | * | * | ||||||
| Schepull175 (2007) | * | * | * | * | * | * | Pain | * | * | * | |||
| Solveborn179 (1994) | * | * | * | * | * | * | Satisfaction | * | * | ||||
| Sorrenti180 (2006) | * | * | * | Time to activities of daily living | * | ||||||||
| Speck181 (1998) | * | * | * | * | * | * | Achilles tendon evaluation score (created by the authors), pain, satisfaction | * | * | * | |||
| Steele182 (1993) | * | * | * | * | |||||||||
| Strauss183 (2007) | * | * | * | * | * | Pain, satisfaction, footwear restrictions, Boyden scale | * | ||||||
| Suchak184 (2008) | * | * | * | * | Number of steps | * | * | * | |||||
| Tarniţă186 (2016) | * | * | Aesthetics of surgical site | * | |||||||||
| Tezeren187 (2006) | * | * | * | * | * | Operative time, duration of hospital stay, scar adhesions, footwear problems, satisfaction, pain | * | ||||||
| Troop190 (1995) | * | * | * | * | * | Satisfaction | * | ||||||
| Vadalá192 (2012) | * | * | * | * | * | * | Hannover score | * | |||||
| Valkering193 (2017) | * | * | * | * | * | * | * | ||||||
| Wredmark201 (1992) | * | * | * | * | * | * | |||||||
| Yotsumoto202 (2010) | * | * | * | * | * | * | Time to walk without pain or fear, time to normal walk, double- and single-legged heel-rises | * | * | ||||
| Zayni203 (2017) | * | * | * | * | * | * | Satisfaction | * | |||||
| Zell204 (2000) | * | * | * | * | * | * | |||||||
| Both Nonsurgical and Surgical Management | |||||||||||||
| Cetti31 (1993) | * | * | * | * | Length of hospital stay, pain | * | * | ||||||
| Costa38 (2006) | * | * | * | * | Time to activities (sport, walking, stair climbing, work) | * | * | * | |||||
| Ebinesan53 (2008) | * | * | Operative time, length of hospital stay, cost | * | |||||||||
| Gwynne-Jones68 (2011) | * | * | Operative time | ||||||||||
| Hutchison82 (2015) | * | * | * | Achilles tendon repair score, cost | * | * | |||||||
| Jackson83 (2013) | * | * | * | * | |||||||||
| Karaaslan90 (2016) | * | * | * | * | * | Satisfaction | * | ||||||
| Kearney93 (2011) | * | Completion rates | * | * | * | ||||||||
| Lantto103 (2016) | * | * | * | * | * | * | * | * | * | ||||
| Lill110 (1996)c | * | * | * | * | * | * | Length of hospital stay | * | |||||
| Lim111 (2018) | * | * | * | ||||||||||
| Lorkowski113 (2007) | * | * | * | * | * | Pain | * | ||||||
| Maffulli115 (2017) | * | * | * | * | * | * | Satisfaction | * | |||||
| Miller132 (2005) | * | * | * | * | Pain, satisfaction | * | |||||||
| Moller137 (2001) | * | * | * | * | * | * | Pain, satisfaction | * | * | * | * | ||
| Nilsson-Helander144 (2010) | * | * | * | * | * | * | |||||||
| Olsson150 (2013) | * | * | * | * | * | * | * | ||||||
| Renninger162 (2016) | * | * | * | * | |||||||||
| Richter164 (1994)c | * | * | * | * | * | ||||||||
| Richter165 (1997)c | * | * | * | * | * | Pain | * | ||||||
| Thermann189 (1995)c | * | * | * | * | * | * | Author-developed score, pain, satisfaction | * | * | * | * | ||
| Twaddle191 (2007) | * | * | * | Squeeze test | * | * | * | ||||||
| Weber196 (2003) | * | * | * | * | * | * | Length of hospital stay, pain, time to discontinuation of crutch use, satisfaction | * | * | ||||
| Willits199 (2010) | * | * | * | * | * | * | |||||||
| Knobe97 (2015) | * | * | * | * | * | * | * | Satisfaction, pain | * | ||||
aPROs, patient-reported outcomes.
bIn Danish.
cIn German.
dIn Spanish.
eIn Portuguese.
References 1 -12, 14, 16 -18, 25 -28, 30 -36, 38 -40, 42 -46, 48, 50 -54, 57, 58, 60, 62 -68, 72, 73, 75 -77, 80 -86, 88 -97, 99 -103, 106 -113, 115 -117, 119 -127, 129, 131 -134, 137 -144, 146, 150 -159, 161 -175, 179 -187, 189 -196, 199, 201 -204.
One or more of the authors has declared the following potential conflict of interest or source of funding: The project received financial support from the Danish Physiotherapy Research Foundation (to M.C.). This study was also funded by the Foundation for Physical Therapy (to K.G.S. and J.A.Z.) and National Institutes of Health under award numbers 1R01AR072034-01A1 (to K.G.S. and J.A.Z.) and T32HD007434 (to J.A.Z.). Funding sources had no role in describing the protocol, planning the project, performing analyses, or interpreting the results. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Agres AN, Gehlen TJ, Arampatzis A, Taylor WR, Duda GN, Manegold S. Short-term functional assessment of gait, plantarflexor strength, and tendon properties after Achilles tendon rupture. Gait Posture. 2018;62:179–185. [DOI] [PubMed] [Google Scholar]
- 2. Aisaiding A, Wang J, Maimaiti R, et al. A novel minimally invasive surgery combined with early exercise therapy promoting tendon regeneration in the treatment of spontaneous Achilles tendon rupture. Injury. 2018;49(3):712–719. [DOI] [PubMed] [Google Scholar]
- 3. Aktas S, Kocaoglu B, Nalbantoglu U, Seyhan M, Guven O. End-to-end versus augmented repair in the treatment of acute Achilles tendon ruptures. J Foot Ankle Surg. 2007;46(5):336–340. [DOI] [PubMed] [Google Scholar]
- 4. Al-Mouazzen L, Rajakulendran K, Najefi A, Ahad N. Percutaneous repair followed by accelerated rehabilitation for acute Achilles tendon ruptures. J Orthop Surg (Hong Kong). 2015;23(3):352–356. [DOI] [PubMed] [Google Scholar]
- 5. Alviti F, Gurzì M, Santilli V, et al. Achilles tendon open surgical treatment with platelet-rich fibrin matrix augmentation: biomechanical evaluation. J Foot Ankle Surg. 2017;56(3):581–585. [DOI] [PubMed] [Google Scholar]
- 6. Andersson T, Eliasson P, Aspenberg P. Tissue memory in healing tendons: short loading episodes stimulate healing. J Appl Physiol. 2009;107:417–421. [DOI] [PubMed] [Google Scholar]
- 7. Andersson T, Eliasson P, Hammerman M, Sandberg O, Aspenberg P. Low-level mechanical stimulation is sufficient to improve tendon healing in rats. J Appl Physiol. 2012;113(9):1398–1402. [DOI] [PubMed] [Google Scholar]
- 8. Aoki M, Ogiwara N, Ohta T, Nabeta Y. Early active motion and weightbearing after cross-stitch Achilles tendon repair. Am J Sports Med. 1998;26(6):794–800. [DOI] [PubMed] [Google Scholar]
- 9. Aspenberg P, Schepull T. Substantial creep in healing human Achilles tendons: a pilot study. Muscles Ligaments Tendons J. 2015;5(3):151–155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Assal M, Jung M, Stern R, Rippstein P, Delmi M, Hoffmeyer P. Limited open repair of Achilles tendon ruptures. J Bone Joint Surg. 2002;84(2):161–170. [PubMed] [Google Scholar]
- 11. Aujla R, Kumar A, Bhatia M. Non-surgical treatment of Achilles rupture: does duration in functional weight bearing orthosis matter? Foot Ankle Surg. 2016;22(4):254–258. [DOI] [PubMed] [Google Scholar]
- 12. Aujla R, Patel S, Jones A, Bhatia M. Predictors of functional outcome in non-operatively managed Achilles tendon ruptures. Foot Ankle Surg. 2018;24(4):336–341. [DOI] [PubMed] [Google Scholar]
- 13. Bäcker HC, Yenchak AJ, Trofa DP, Vosseller JT. Strength measurement after Achilles tendon repair. Foot Ankle Spec. 2019;12(5):471-479. [DOI] [PubMed] [Google Scholar]
- 14. Barfod KW, Bencke J, Lauridsen HB, Ban I, Ebskov L, Troelsen A. Nonoperative dynamic treatment of acute Achilles tendon rupture: the influence of early weight-bearing on clinical outcome: a blinded, randomized controlled trial. J Bone Joint Surg Am. 2014;96(18):1497–1503. [DOI] [PubMed] [Google Scholar]
- 15. Barfod KW, Bencke J, Lauridsen HB, Dippmann C, Ebskov L, Troelsen A. Nonoperative, dynamic treatment of acute Achilles tendon rupture: influence of early weightbearing on biomechanical properties of the plantar flexor muscle-tendon complex—a blinded, randomized, controlled trial. J Foot Ankle Surg. 2015;54(2):220–226. [DOI] [PubMed] [Google Scholar]
- 16. Baumfeld D, Baumfeld T, Spiezia F, Nery C, Zambelli R, Maffulli N. Isokinetic functional outcomes of open versus percutaneous repair following Achilles tendon tears. Foot Ankle Surg. 2019;25(4):503-506. [DOI] [PubMed] [Google Scholar]
- 17. Bevoni R, Angelini A, D’Apote G, et al. Long term results of acute Achilles repair with triple-bundle technique and early rehabilitation protocol. Injury. 2014;45(8):1268–1274. [DOI] [PubMed] [Google Scholar]
- 18. Bhattacharyya M, Gerber B. Mini-invasive surgical repair of the Achilles tendon—does it reduce post-operative morbidity? Int Orthop. 2009;33:151–156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bhattacharyya M, Gerber B. Minimally-invasive surgical repair of ruptured Achilles tendon as a day case procedure with early full weight bearing. Journal of One-day Surgery. 17(3):70–75. [Google Scholar]
- 20. Bostick GP, Jomha NM, Suchak AA, Beaupré LA. Factors associated with calf muscle endurance recovery 1 year after Achilles tendon rupture repair. J Orthop Sports Phys Ther. 2010;40(6):345–351. [DOI] [PubMed] [Google Scholar]
- 21. Braunstein M, Baumbach SF, Boecker W, Carmont MR, Polzer H. Development of an accelerated functional rehabilitation protocol following minimal invasive Achilles tendon repair. Knee Surg Sports Traumatol Arthrosc. 2018;26(3):846–853. [DOI] [PubMed] [Google Scholar]
- 22. Brorsson A, Silbernagel KG, Olsson N, Helander KN. Calf muscle performance deficits remain 7 years after an Achilles tendon rupture. Am J Sports Med. 2017;46(2):470–477. [DOI] [PubMed] [Google Scholar]
- 23. Brorsson A, Willy RW, Tranberg R, Grävare Silbernagel K. Heel-rise height deficit 1 year after Achilles tendon rupture relates to changes in ankle biomechanics 6 years after injury. Am J Sports Med. 2017;45(13):3060–3068. [DOI] [PubMed] [Google Scholar]
- 24. Brumann M, Baumbach SF, Mutschler W, Polzer H. Accelerated rehabilitation following Achilles tendon repair after acute rupture—development of an evidence-based treatment protocol. Injury. 2014;45(11):1782–1790. [DOI] [PubMed] [Google Scholar]
- 25. Buchgraber A, Pässler HH. Percutaneous repair of Achilles tendon rupture: immobilization versus functional postoperative treatment. Clin Orthop Relat Res. 1997;341:113–122. [PubMed] [Google Scholar]
- 26. Calder JDF, Saxby TS. Early, active rehabilitation following mini-open repair of Achilles tendon rupture: a prospective study. Br J Sports Med. 2005;39:857–859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Carmont MR, Grävare Silbernagel K, Brorsson A, Olsson N, Maffulli N, Karlsson J. The Achilles tendon resting angle as an indirect measure of Achilles tendon length following rupture, repair, and rehabilitation. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2015;2(2):49–55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Carmont MR, Zellers JA, Brorsson A, et al. Functional outcomes of Achilles tendon minimally invasive repair using 4- and 6-strand nonabsorbable suture: a cohort comparison study. Orthop J Sports Med. 2017;5(8):2325967117723347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Carvalho FA, Kamper SJ. Effects of early rehabilitation following operative repair of Achilles tendon rupture (PEDro synthesis). Br J Sports Med. 2016;50(13):829–830. [DOI] [PubMed] [Google Scholar]
- 30. Ceccarelli F, Berti L, Giuriati L, Romagnoli M, Giannini S. Percutaneous and minimally invasive techniques of Achilles tendon repair. Clin Orthop Relat Res. 2007;458:188–193. [DOI] [PubMed] [Google Scholar]
- 31. Cetti R, Christensen S-E, Ejsted R, Jensen NM, Jorgensen U. Operative versus nonoperative treatment of Achilles tendon rupture: a prospective randomized study and review of the literature. Am J Sports Med. 1993;21:791–799. [DOI] [PubMed] [Google Scholar]
- 32. Cetti R, Henriksen LO, Jacobsen KS. A new treatment of ruptured Achilles tendons: a prospective randomized study. Clin Orthop Relat Res. 1994;308:155–165. [PubMed] [Google Scholar]
- 33. Chandrakant V, Lozano-Calderon S, McWilliam J. Immediate weight bearing after modified percutaneous Achilles tendon repair. Foot Ankle Int. 2012;33(12):1093–1097. [DOI] [PubMed] [Google Scholar]
- 34. Chen H, Ji X, Zhang Q, Liang X, Tang P. Channel-assisted minimally invasive repair of acute Achilles tendon rupture. J Orthop Surg Res. 2015;10:167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Chiu C-H, Yeh W-L, Tsai M-C, Chang S-S, Hsu K-Y, Chan Y-S. Endoscopy-assisted percutaneous repair of acute Achilles tendon tears. Foot Ankle Int. 2013;34(123):1168–1176. [DOI] [PubMed] [Google Scholar]
- 36. Chmielnicki M, Prokop A. Zwipp percutaneous suture of the Achilles tendon with the Dresden instruments. Z Orthop Unfall. 2016;154:303–305. [DOI] [PubMed] [Google Scholar]
- 37. Collins R, Sudlow A, Loizou C, Loveday DT, Smith G. Closing the gap on Achilles tendon rupture: a cadaveric study quantifying the tendon apposition achieved with commonly used immobilisation practices. Foot Ankle Surg. 2018;24(2):124–127. [DOI] [PubMed] [Google Scholar]
- 38. Costa ML, MacMillan K, Halliday D, et al. Randomised controlled trials of immediate weight-bearing mobilisation for rupture of the tendo Achillis. J Bone Joint Surg Br. 2006;88(1):69–77. [DOI] [PubMed] [Google Scholar]
- 39. Costa ML, Shepstone L, Darrah C, Marshall T, Donell ST. Immediate full-weight-bearing mobilisation for repaired Achilles tendon ruptures: a pilot study. Injury. 2003;34:874–876. [DOI] [PubMed] [Google Scholar]
- 40. Cretnik A, Kosanovic M, Smrkolj V. Percutaneous versus open repair of the ruptured Achilles tendon: a comparative study. Am J Sports Med. 2005;33(9):1369–1379. [DOI] [PubMed] [Google Scholar]
- 41. Čretnik A, Kosanović M, Smrkolj V. Percutaneous suturing of the ruptured Achilles tendon under local anesthesia. J Foot Ankle Surg. 2004;43(2):72–81. [DOI] [PubMed] [Google Scholar]
- 42. De Carli A, Lanzetti RM, Ciompi A, et al. Can platelet-rich plasma have a role in Achilles tendon surgical repair? Knee Surg Sports Traumatol Arthrosc. 2016;24(7):2231–2237. [DOI] [PubMed] [Google Scholar]
- 43. De la Fuente C, Peña y Lillo R, Carreño G, Marambio H. Prospective randomized clinical trial of aggressive rehabilitation after acute Achilles tendon ruptures repaired with Dresden technique. Foot (Edinb). 2016;26:15–22. [DOI] [PubMed] [Google Scholar]
- 44. De la Fuente CI, Lillo RPY, Campillo RR, et al. Medial gastrocnemius myotendinous junction displacement and plantar-flexion strength in patients treated with immediate rehabilitation after Achilles tendon repair. J Athl Train. 2016;51(12):1013–1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Delgado-Brambila H, Cristiani- DG, Tinajero- EC, Burgos-Elías V. Reparación de ruptura del tendón calcáneo y rehabilitación temprana. Acta Ortopédica Mex. 2012;26(2):50–89. [PubMed] [Google Scholar]
- 46. Ding W, Yan W, Zhu Y, Liu Z. Treatment of acute and closed Achilles tendon ruptures by minimally invasive tenocutaneous suturing. Ulus Travma Acil Cerrahi Derg. 2012;18(5):405–410. [DOI] [PubMed] [Google Scholar]
- 47. Ding WG, Zhu YP, Yan WH. Treatment of acute and closed Achilles tendon ruptures by minimally invasive tenocutaneous suturing. J Foot Ankle Surg. 2013;52(2):143–146. [DOI] [PubMed] [Google Scholar]
- 48. Dolphin P, Bainbridge K, Mackenney P, Dixon J. Functional dynamic bracing and functional rehabilitation for Achilles tendon ruptures: a case series. Physiotherapy Practice and Research. 2016;37(2):119–125. [Google Scholar]
- 49. Domeij-Arverud E, Labruto F, Latifi A, Nilsson G, Edman G, Ackermann PW. Intermittent pneumatic compression reduces the risk of deep vein thrombosis during postoperative lower limb immobilisation: a prospective randomised trial of acute ruptures of the Achilles tendon. Bone Joint J. 2015;97(5):675–680. [DOI] [PubMed] [Google Scholar]
- 50. Don R, Ranavolo A, Cacchio A, et al. Relationship between recovery of calf-muscle biomechanical properties and gait pattern following surgery for Achilles tendon rupture. Clin Biomech (Bristol, Avon). 2007;22:211–220. [DOI] [PubMed] [Google Scholar]
- 51. Doral MN. What is the effect of the early weight-bearing mobilisation without using any support after endoscopy-assisted Achilles tendon repair? Knee Surg Sports Traumatol Arthrosc. 2013;21:1378–1384. [DOI] [PubMed] [Google Scholar]
- 52. Dos Santos Gomes CT. Ruptura do tendão de Aquiles: tratamento cirúrgico, mobilização e carga precoces. Rev Bras Ortop. 1998;33(12):951–958. [Google Scholar]
- 53. Ebinesan AD, Sarai BS, Walley GD, Maffulli N. Conservative, open or percutaneous repair for acute rupture of the Achilles tendon. Disabil Rehabil. 2008;30:1721–1725. [DOI] [PubMed] [Google Scholar]
- 54. Ecker TM, Bremer AK, Krause FG, Müller T, Weber M. Prospective use of a standardized nonoperative early weightbearing protocol for Achilles tendon rupture: 17 years of experience. Am J Sports Med. 2016;44(4):1004–1010. [DOI] [PubMed] [Google Scholar]
- 55. El-Akkawi AI, Joanroy R, Barfod KW, Kallemose T, Kristensen SS, Viberg B. Effect of early versus late weightbearing in conservatively treated acute Achilles tendon rupture: a meta-analysis. J Foot Ankle Surg. 2018;57(2):346–352. [DOI] [PubMed] [Google Scholar]
- 56. Ellison P, Molloy A, Mason LW. Early protected weightbearing for acute ruptures of the Achilles tendon: do commonly used orthoses produce the required equinus? J Foot Ankle Surg. 2017;56(5):960–963. [DOI] [PubMed] [Google Scholar]
- 57. Fernández-Fairén M, Gimeno C. Augmented repair of Achilles tendon ruptures. Am J Sports Med. 1997;25(2):177–181. [DOI] [PubMed] [Google Scholar]
- 58. Fitzgibbons RE, Hefferon J, Hill J. Percutaneous Achilles tendon repair. Am J Sports Med. 1993;21(5):724–727. [DOI] [PubMed] [Google Scholar]
- 59. Freedman B, Gordon J, Bhatt P, et al. Nonsurgical treatment and early return to activity leads to improved Achilles tendon fatigue mechanics and functional outcomes during early healing in an animal model. J Orthop Res. 2016;34(12):2172–2180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Gaiani L, Bertelli R, Palmonari M. Dynamic percutaneous repair of the ruptured tendo Achillis. Eur J Orthop Surg Traumatol. 2012;22:709–712. [DOI] [PubMed] [Google Scholar]
- 61. Ganestam A, Kallemose T, Troelsen A, Barfod KW. Increasing incidence of acute Achilles tendon rupture and a noticeable decline in surgical treatment from 1994 to 2013: a nationwide registry study of 33,160 patients. Knee Surg Sports Traumatol Arthrosc. 2016;24(12):3730–3737. [DOI] [PubMed] [Google Scholar]
- 62. Garrido IM, Deval JC, Bosch MN, Mediavilla DH, Garcia VP, González MS. Treatment of acute Achilles tendon ruptures with Achillon device: clinical outcomes and kinetic gait analysis. Foot Ankle Surg. 2010;16(4):189–194. [DOI] [PubMed] [Google Scholar]
- 63. Geremia JM, Bobbert MF, Casa Nova M, et al. The structural and mechanical properties of the Achilles tendon 2 years after surgical repair. Clin Biomech (Bristol, Avon). 2015;30(5):485–492. [DOI] [PubMed] [Google Scholar]
- 64. Gigante A, Moschini A, Verdenelli A, Del Torto M, Ulisse S, De Palma L. Open versus percutaneous repair in the treatment of acute Achilles tendon rupture: a randomized prospective study. Knee Surg Sports Traumatol Arthrosc. 2008;16:204–209. [DOI] [PubMed] [Google Scholar]
- 65. Gorschewsky O, Pitzl M, Pütz A, Klakow A, Neumann W. Percutaneous repair of acute Achilles tendon rupture. Foot Ankle Int. 2004;25(4):219–224. [DOI] [PubMed] [Google Scholar]
- 66. Gorschewsky O, Vogel U, Schweizer A, van Laar B. Percutaneous tenodesis of the Achilles tendon: a new surgical method for the treatment of acute Achilles tendon rupture through percutaneous tenodesis. Injury. 1999;30:315–321. [DOI] [PubMed] [Google Scholar]
- 67. Groetelaers RPTGC, Janssen L, van der Velden J, et al. Functional treatment or cast immobilization after minimally invasive repair of an acute Achilles tendon rupture: prospective, randomized trial. Foot Ankle Int. 2014;35(8):771–778. [DOI] [PubMed] [Google Scholar]
- 68. Gwynne-Jones DP, Sims M, Handcock D. Epidemiology and outcomes of acute Achilles tendon rupture with operative or nonoperative treatment using an identical functional bracing protocol. Foot Ankle Int. 2011;32:337–343. [DOI] [PubMed] [Google Scholar]
- 69. Hansen M, Christensen M, Budolfsen T, et al. Achilles tendon total rupture score at 3 months can predict patients’ ability to return to sport 1 year after injury. Knee Surg Sports Traumatol Arthrosc. 2016;24(4):1365–1371. [DOI] [PubMed] [Google Scholar]
- 70. Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)—a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71. Heikkinen J, Lantto I, Flinkkila T, et al. Soleus atrophy is common after the nonsurgical treatment of acute Achilles tendon ruptures. Am J Sports Med. 2017;45(6):1395–1404. [DOI] [PubMed] [Google Scholar]
- 72. Heikkinen J, Lantto L, Flinkkila T, et al. Augmented compared with nonaugmented surgical repair after total Achilles rupture: results of a prospective randomized trial with thirteen or more years of follow-up. J Bone Joint Surg. 2016;98:85–92. [DOI] [PubMed] [Google Scholar]
- 73. Henríquez H, Muñoz R, Carcuro G, Bastías C. Is percutaneous repair better than open repair in acute Achilles tendon rupture? Clin Orthop Relat Res. 2012;470:998–1003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Holm C, Kjaer M, Eliasson P. Achilles tendon rupture—treatment and complications: a systematic review. Scand J Med Sci Sports. 2015;25(1):e1–e10. [DOI] [PubMed] [Google Scholar]
- 75. Holmenschlager F, Schubert S, Winckler S. Achilles tendon rupture: early dynamic mobilisation after surgery. Zentralbl Chir. 2002;127:519–522. [DOI] [PubMed] [Google Scholar]
- 76. Horter M, Horter M, Wetterkamp D, Rieger H. Offene rekonstruktion der Achillessehnenruptur—wann und wie? Chir Prax. 2007;67:611–620. [Google Scholar]
- 77. Hrnack SA, Crates JM, Barber FA. Primary Achilles tendon repair with mini-dorsolateral incision technique and accelerated rehabilitation. Foot Ankle Int. 2012;33:848–851. [DOI] [PubMed] [Google Scholar]
- 78. Huang J, Wang C, Ma X, Wang X, Zhang C, Chen L. Rehabilitation regimen after surgical treatment of acute Achilles tendon ruptures: a systematic review with meta-analysis. Am J Sports Med. 2015;43(4):1008–1016. [DOI] [PubMed] [Google Scholar]
- 79. Huffer D, Hing W, Newton R, Clair M. Strength training for plantar fasciitis and the intrinsic foot musculature: a systematic review. Phys Ther Sport. 2017;24(2016):44–52. [DOI] [PubMed] [Google Scholar]
- 80. Hüfner T, Wohifarth K, Fink M, Thermann H, Rollnik JD. EMG monitoring during functional non-surgical therapy of Achilles tendon rupture. Foot Ankle Int. 2002;23(7):614–618. [DOI] [PubMed] [Google Scholar]
- 81. Hüfner TM, Brandes DB, Thermann H, Richter M, Knobloch K, Krettek C. Long-term results after functional nonoperative treatment of Achilles tendon rupture. Foot Ankle Int. 2006;27:167–171. [DOI] [PubMed] [Google Scholar]
- 82. Hutchison AM, Topliss C, Beard D, Evans RM, Williams P. The treatment of a rupture of the Achilles tendon using a dedicated management programme. Bone Joint J. 2015;97(4):510–515. [DOI] [PubMed] [Google Scholar]
- 83. Jackson G, Sinclair VF, McLaughlin C, Barrie J. Outcomes of functional weight-bearing rehabilitation of Achilles tendon ruptures. Orthopedics. 2013;36(8):e1053–e1059. [DOI] [PubMed] [Google Scholar]
- 84. Jacob KM, Paterson R. Surgical repair followed by functional rehabilitation for acute and chronic Achilles tendon injuries: excellent functional results, patient satisfaction and no reruptures. ANZ J Surg. 2007;77(4):287–291. [DOI] [PubMed] [Google Scholar]
- 85. Jallageas R, Bordes J, Daviet J-C, Mabit C, Coste C. Evaluation of surgical treatment for ruptured Achilles tendon in 31 athletes. Orthop Traumatol Surg Res. 2013;99(5):577–584. [DOI] [PubMed] [Google Scholar]
- 86. Jielile J, Sabirhazi G, Chen J, et al. Novel surgical technique and early kinesiotherapy for acute Achilles tendon rupture. Foot Ankle Int. 2012;33:1119–1127. [DOI] [PubMed] [Google Scholar]
- 87. Kangas J, Pajala A, Ohtonen P, Leppilahti J. Achilles tendon elongation after rupture repair: a randomized comparison of 2 postoperative regimens. Am J Sports Med. 2007;35:59–64. [DOI] [PubMed] [Google Scholar]
- 88. Kangas J, Pajala A, Siira P, Hämäläinen M, Leppilahti J. Early functional treatment versus early immobilization in tension of the musculotendinous unit after Achilles rupture repair: a prospective, randomized, clinical study. J Trauma. 2003;54(6):1171–1180. [DOI] [PubMed] [Google Scholar]
- 89. Kaniki N, Willits K, Mohtadi NGH, Fung V, Bryant D. A retrospective comparative study with historical control to determine the effectiveness of platelet-rich plasma as part of nonoperative treatment of acute Achilles tendon rupture. Arthroscopy. 2014;30(9):1139–1145. [DOI] [PubMed] [Google Scholar]
- 90. Karaaslan F, Mermerkaya MU, Cirakli A, Karaoglu S, Duygulu F. Surgical versus conservative treatment following acute rupture of the Achilles tendon: is there a pedobarographic difference? Ther Clin Risk Manag. 2016;12:1311–1315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Karabinas PK, Benetos IS, Lampropoulou-Adamidou K, Romoudis P, Mavrogenis AF, Vlamis J. Percutaneous versus open repair of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol. 2014;24:607–613. [DOI] [PubMed] [Google Scholar]
- 92. Kauranen K, Kangas J, Leppilahti J. Recovering motor performance of the foot after Achilles rupture repair: a randomized clinical study about early functional treatment vs. early immobilization of Achilles tendon in tension. Foot Ankle Int. 2002;23(7):600–605. [DOI] [PubMed] [Google Scholar]
- 93. Kearney RS, Achten J, Parsons NR, Costa ML. The comprehensive cohort model in a pilot trial in orthopaedic trauma. BMC Med Res Methodol. 2011;11(1):39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Keller A, Ortiz C, Wagner E, Wagner P, Mococain P. Mini-open tenorrhaphy of acute Achilles tendon ruptures: medium-term follow-up of 100 cases. Am J Sports Med. 2014;42(3):731–736. [DOI] [PubMed] [Google Scholar]
- 95. Kerkhoffs GM, Struijs PA, Raaymakers EL, Marti RK. Functional treatment after surgical repair of acute Achilles tendon rupture: wrap vs walking cast. Arch Orthop Trauma Surg. 2002;122:102–105. [DOI] [PubMed] [Google Scholar]
- 96. Kim U, Choi YS, Jang GC, Choi YR. Early rehabilitation after open repair for patients with a rupture of the Achilles tendon. Injury. 2017;48(7):1710–1713. [DOI] [PubMed] [Google Scholar]
- 97. Knobe M, Gradl G, Klos K, et al. Is percutaneous suturing superior to open fibrin gluing in acute Achilles tendon rupture? Int Orthop. 2015;39(3):535–542. [DOI] [PubMed] [Google Scholar]
- 98. Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction. Br J Sports Med. 2018;52(6):387–407. [DOI] [PubMed] [Google Scholar]
- 99. Korkmaz M, Erkoc MF, Yolcu S, Balbaloglu O, Öztemur Z, Karaaslan F. Weight bearing the same day versus non-weight bearing for 4 weeks in Achilles tendon rupture. J Orthop Sci. 2015;20(3):513–516. [DOI] [PubMed] [Google Scholar]
- 100. Kuskucu M, Mahirogullari M, Solakoglu C, et al. Treatment of rupture of the Achilles tendon with fibrin sealant. Foot Ankle Int. 2005;26(10):826–831. [DOI] [PubMed] [Google Scholar]
- 101. Lacoste S, Cherrier B, Féron JM. Intra-operative ultrasonography in the percutaneous tenorraphy of acute Achilles tendon ruptures. Eur J Orthop Surg Traumatol. 2012;22(7):585–591. [DOI] [PubMed] [Google Scholar]
- 102. Lansdaal JR, Goslings JC, Reichart M, et al. The results of 163 Achilles tendon ruptures treated by a minimally invasive surgical technique and functional aftertreatment. Injury. 2007;38:839–844. [DOI] [PubMed] [Google Scholar]
- 103. Lantto I, Heikkinen J, Flinkkila T, et al. A prospective randomized trial comparing surgical and nonsurgical treatments of acute Achilles tendon ruptures. Am J Sports Med. 2016;44(9):2406–2414. [DOI] [PubMed] [Google Scholar]
- 104. Lantto I, Heikkinen J, Flinkkila T, et al. Early functional treatment versus cast immobilization in tension after Achilles rupture repair: results of a prospective randomized trial with 10 or more years of follow-up. Am J Sports Med. 2015;43(9):2302–2309. [DOI] [PubMed] [Google Scholar]
- 105. Lantto I, Heikkinen J, Flinkkila T, Ohtonen P, Leppilahti J. Epidemiology of Achilles tendon ruptures: increasing incidence over a 33-year period. Scand J Med Sci Sports. 2015;25(1):e133–e138. [DOI] [PubMed] [Google Scholar]
- 106. Lapidus LJ, Rosfors S, Ponzer S, et al. Prolonged thromboprophylaxis with dalteparin after surgical treatment of Achilles tendon rupture: a randomized, placebo-controlled study. J Orthop Trauma. 2007;21(1):52–57. [DOI] [PubMed] [Google Scholar]
- 107. Lee DK. A preliminary study on the effects of acellular tissue graft augmentation in acute Achilles tendon ruptures. J Foot Ankle Surg. 2008;47(1):8–12. [DOI] [PubMed] [Google Scholar]
- 108. Leppilahti J, Lahde S, Forsman K, Kangas J, Kauranen K, Orava S. Relationship between calf muscle size and strength after Achilles rupture repair. Foot Ankle Int. 2000;21(4):330–335. [DOI] [PubMed] [Google Scholar]
- 109. Li C-G, Li B, Yang Y-F. Management of acute Achilles tendon rupture with tendon-bundle technique. J Int Med Res. 2017;45(1):310–319. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Lill H, Moor C, Fecht E, Kalbe P, Echtermeyer V. Achillessehnenruptur—operative oder konservativ funktionelle Behandlung? Akt Traumatol. 1996;26:95–100. [Google Scholar]
- 111. Lim CS, Lees D, Gwynne-Jones DP. Functional outcome of acute Achilles tendon rupture with and without operative treatment using identical functional bracing protocol. Foot Ankle Int. 2018;38(12):1331–1336. [DOI] [PubMed] [Google Scholar]
- 112. Lonzarić D, Kruščić A, Dinevski D, Povalej Bržan P, Jesenšek Papež B. Primary surgical repair of acute Achilles tendon rupture: comparative results of three surgical techniques. Wien Klin Wochenschr. 2017;129(5-6):176–185. [DOI] [PubMed] [Google Scholar]
- 113. Lorkowski J, Brongel L, Hładki W, et al. Evaluation of long term therapy outcomes for Achilles tendon ruptures. Pol Przegl Chir. 2007;79(6):745–756. [Google Scholar]
- 114. MacDermid JC, Silbernagel KG. Outcome evaluation in tendinopathy: foundations of assessment and a summary of selected measures. J Orthop Sports Phys Ther. 2015;45(11):950–964. [DOI] [PubMed] [Google Scholar]
- 115. Maffulli G, Del Buono A, Richards P, Oliva F, Maffulli N. Conservative, minimally invasive and open surgical repair for management of acute ruptures of the Achilles tendon: a clinical and functional retrospective study. Muscles Ligaments Tendons J. 2017;7(1):46–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116. Maffulli N, Longo UG, Ronga M, Khanna A, Denaro V. Favorable outcome of percutaneous repair of Achilles tendon ruptures in the elderly. Clin Orthop Relat Res. 2010;468:1039–1046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117. Maffulli N, Tallon C, Wong J, Lim KP, Bleakney R. Early weightbearing and ankle mobilization after open repair of acute midsubstance tears of the Achilles tendon. Am J Sports Med. 2003;31(5):692–700. [DOI] [PubMed] [Google Scholar]
- 118. Maffulli N, Tallon C, Wong J, Peng Lim K, Bleakney R. No adverse effect of early weight bearing following open repair of acute tears of the Achilles tendon. J Sports Med Phys Fitness. 2003;43(3):367–379. [PubMed] [Google Scholar]
- 119. Maffulli N, Thorpe AP, Smith EW. Magnetic resonance imaging after operative repair of Achilles tendon rupture. Scand J Med Sci Sports. 2001;11:156–162. [PubMed] [Google Scholar]
- 120. Majewski M, Schaeren S, Kohlhaas U, Ochsner PE. Postoperative rehabilitation after percutaneous Achilles tendon repair: early functional therapy versus cast immobilization. Disabil Rehabil. 2008;30(20-22):1726–1732. [DOI] [PubMed] [Google Scholar]
- 121. Mandelbaum BR, Myerson MS, Forster R. Achilles tendon ruptures: a new method of repair, early range of motion, and functional rehabilitation. Am J Sports Med. 1995;23(4):392–395. [DOI] [PubMed] [Google Scholar]
- 122. Marti R, Werken van der, Schutte P, Bast T. Operative repair of ruptured Achilles tendon and functional after-treatment—I: acute rupture. Neth J Surg. 1983;35(2):61–64. [PubMed] [Google Scholar]
- 123. Martinelli B. Percutaneous repair of the Achilles tendon in athletes. Bull Hosp Jt Dis. 2000;59(3):149–152. [PubMed] [Google Scholar]
- 124. Mauch M, Ulrich M, Kaelin X, Segesser B, Paul J. Biomechanical evaluation of rehabilitation after surgical repair of Achilles tendon ruptures. Sportverletz Sportschaden. 2017;31:222–230. [DOI] [PubMed] [Google Scholar]
- 125. Mavrodontidis A, Lykissas M, Koulouvaris P, Pafilas D, Kontogeorgakos V, Zalavras C. Percutaneous repair of acute Achilles tendon rupture: a functional evaluation study with a minimum 10-year follow-up. Acta Orthop Traumatol Turc. 2015;49(6):661–667. [DOI] [PubMed] [Google Scholar]
- 126. Mayer A, Frasson VB, Ott R, Fortuna RO, Vaz MA. Desequilíbrios musculares entre flexores dorsais e plantares do tornozelo após tratamento conservador e acelerado da ruptura do tendão calcâneo. Muscle imbalance between ankle dorsiflexors and plantarflexors after conservative and accelerated treatment. Fisioter e Pesqui. 2010;17(2):108–113. [Google Scholar]
- 127. McComis GP, Nawoczenski DA, DeHaven K. Functional bracing for rupture of the Achilles tendon: clinical results and analysis of ground-reaction forces and temporal data. J Bone Joint Surg. 1997;79(12):1799–1808. [DOI] [PubMed] [Google Scholar]
- 128. McCormack R, Bovard J. Early functional rehabilitation or cast immobilisation for the postoperative management of acute Achilles tendon rupture? A systematic review and meta-analysis of randomised controlled trials. Br J Sports Med. 2015;49(20):1329–1335. [DOI] [PubMed] [Google Scholar]
- 129. McNair P, Nordez A, Olds M, Young SW, Cornu C. Biomechanical properties of the plantar flexor muscle-tendon complex 6 months post-rupture of the Achilles tendon. J Orthop Res. 2013;31(9):1469–1474. [DOI] [PubMed] [Google Scholar]
- 130. Metz R, van der Heijden GJMG, Verleisdonk E-JMM, Tamminga R, van der Werken C. Recovery of calf muscle strength following Achilles tendon rupture treatment: a comparison between minimally invasive surgery and conservative treatment. Foot Ankle Spec. 2009;2(5):219–226. [DOI] [PubMed] [Google Scholar]
- 131. Mezzarobba S, Bortolato S, Giacomazzi A, Fancellu G, Marcovich R, Valentini R. Percutaneous repair of Achilles tendon ruptures with Tenolig: quantitative analysis of postural control and gait pattern. Foot (Edinb). 2012;22(4):303–309. [DOI] [PubMed] [Google Scholar]
- 132. Miller D, Waterston S, Reaper J, Barrass V, Maffulli N. Conservative management, percutaneous or open repair of acute Achilles tendon rupture: a retrospective study. Scott Med J. 2005;50(4):160–165. [DOI] [PubMed] [Google Scholar]
- 133. Miyamoto W, Imade S, Innami K, Kawano H, Takao M. Acute Achilles tendon rupture treated by double side-locking loop suture technique with early rehabilitation. Foot Ankle Int. 2017;38(2):167–173. [DOI] [PubMed] [Google Scholar]
- 134. Moberg A, Nordgren B, Solveborn S. Surgically repaired Achilles tendon ruptures with postoperative mobile ankle cast: a 12-month follow-up study with an isokinetic and a dynamic muscle function test. Scand J Med Sci Sports. 1992;2(4):231–233. [Google Scholar]
- 135. Möller M, Kälebo P, Tidebrant G, Movin T, Karlsson J. The ultrasonographic appearance of the ruptured Achilles tendon during healing: a longitudinal evaluation of surgical and nonsurgical treatment, with comparisons to MRI appearance. Knee Surg Sports Traumatol Arthrosc. 2002;10:49–56. [DOI] [PubMed] [Google Scholar]
- 136. Möller M, Lind K, Movin T, Karlsson J. Calf muscle function after Achilles tendon rupture: a prospective, randomised study comparing surgical and non-surgical treatment. Scand J Med Sci Sports. 2002;12(1):9–16. [DOI] [PubMed] [Google Scholar]
- 137. Moller M, Movin T, Granhed H, Lind K, Faxen E, Karlsson J. Acute rupture of tendon Achillis: a prospective randomised study of comparison between surgical and non-surgical treatment. J Bone Joint Surg Br. 2001;83(6):843–848. [DOI] [PubMed] [Google Scholar]
- 138. Mortensen HM, Skov O, Jensen PE. Early motion of the ankle after operative treatment of a rupture of the Achilles tendon: a prospective, randomized clinical and radiographic study. J Bone Joint Surg. 1999;81(7):983–990. [DOI] [PubMed] [Google Scholar]
- 139. Mortensen N, Saether J, Steinke M, Staehr H, Mikkelsen S. Separation of tendon ends after Achilles tendon repair: a prospective, randomized, multicenter study. Orthopedics. 1992;15(8):899–903. [DOI] [PubMed] [Google Scholar]
- 140. Motta P, Errichiello C, Pontini I. Achilles tendon rupture: a new technique for easy surgical repair and immediate movement of the ankle and foot. Am J Sports Med. 1997;25(2):172–176. [DOI] [PubMed] [Google Scholar]
- 141. Mukundan C, El Husseiny M, Rayan F, Salim J, Budgen A. “Mini-open” repair of acute tendo Achilles ruptures—the solution? Foot Ankle Surg. 2010;16(3):122–125. [DOI] [PubMed] [Google Scholar]
- 142. Mullaney MJ, McHugh MP, Tyler TF, Nicholas SJ, Lee SJ. Weakness in end-range plantar flexion after Achilles tendon repair. Am J Sports Med. 2006;34:1120–1125. [DOI] [PubMed] [Google Scholar]
- 143. Neumayer F, Mouhsine E, Arlettaz Y, Gremion G, Wettstein M, Crevoisier X. A new conservative-dynamic treatment for the acute ruptured Achilles tendon. Arch Orthop Trauma Surg. 2010;130(3):363–368. [DOI] [PubMed] [Google Scholar]
- 144. Nilsson-Helander K, Silbernagel KG, Thomeé R, et al. Acute Achilles tendon rupture: a randomized, controlled study comparing surgical and nonsurgical treatments using validated outcome measures. Am J Sports Med. 2010;38(11):2186–2193. [DOI] [PubMed] [Google Scholar]
- 145. O’Connor SR, Tully MA, Ryan B, Bradley JM, Baxter GD, McDonough SM. Failure of a numerical quality assessment scale to identify potential risk of bias in a systematic review: a comparison study. BMC Res Notes. 2015;8:224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Ocguder DA, Dogan M, Bektaser SB, Akgun E, Tolunay T, Ugurlu M. Comparison of the open primary repair with augmentation and without augmentation in acute Achilles tendon rupture. Turkish J Med Sci. 2011;41(4):639–646. [Google Scholar]
- 147. Olsson N, Karlsson J, Eriksson BI, Brorsson A, Lundberg M, Silbernagel KG. Ability to perform a single heel-rise is significantly related to patient-reported outcome after Achilles tendon rupture. Scand J Med Sci Sports. 2014;24:152–158. [DOI] [PubMed] [Google Scholar]
- 148. Olsson N, Nilsson-Helander K, Karlsson J, et al. Major functional deficits persist 2 years after acute Achilles tendon rupture. Knee Surg Sports Traumatol Arthrosc. 2011;19:1385–1393. [DOI] [PubMed] [Google Scholar]
- 149. Olsson N, Petzold M, Brorsson A, Karlsson J, Eriksson BI, Grävare Silbernagel K. Predictors of clinical outcome after acute Achilles tendon ruptures. Am J Sports Med. 2014;42(6):1448–1455. [DOI] [PubMed] [Google Scholar]
- 150. Olsson N, Silbernagel KG, Eriksson BI, et al. Stable surgical repair with accelerated rehabilitation versus nonsurgical treatment for acute Achilles tendon ruptures: a randomized controlled study. Am J Sports Med. 2013;41(12):2867–2876. [DOI] [PubMed] [Google Scholar]
- 151. Ozer H, Selek HY, Harput G, Oznur A, Baltaci G. Achilles tendon open repair augmented with distal turndown tendon flap and posterior crural fasciotomy. J Foot Ankle Surg. 2016;55(6):1180–1184. [DOI] [PubMed] [Google Scholar]
- 152. Ozkan H, Ege T, Koca K, Can N, Yurttas Y, Tunay S. Pedobarographic measurements after repair of Achilles tendon by minimal invasive surgery. Acta Orthop Belg. 2016;82:271–274. [PubMed] [Google Scholar]
- 153. Ozkaya U, Parmaksizoglu AS, Kabukcuoglu Y, Sokucu S, Basilgan S. Open minimally invasive Achilles tendon repair with early rehabilitation: functional results of 25 consecutive patients. Injury. 2009;40(6):669–672. [DOI] [PubMed] [Google Scholar]
- 154. Peng W-C, Chang Y-P, Chao Y-H, et al. Morphomechanical alterations in the medial gastrocnemius muscle in patients with a repaired Achilles tendon: associations with outcome measures. Clin Biomech (Bristol, Avon). 2017;43:50–57. [DOI] [PubMed] [Google Scholar]
- 155. Persson A, Wredmark T. The treatment of total ruptures of the Achilles tendon by plaster immobilisation. Int Orthop. 1979;3(2):149–152. [DOI] [PubMed] [Google Scholar]
- 156. Petersen OF, Nielsen MB, Jensen KH, Solgaard S. Randomiseret sammenligning af genanvendelig stovle og letvaegtsgips til behandling af forstegangs akillesseneruptur. Ugeskr Laeger. 2002;164:3852–3855. [PubMed] [Google Scholar]
- 157. Porter DA, Barnes AF, Rund AM, Kaz AJ, Tyndall JA, Millis AA. Acute Achilles tendon repair: strength outcomes after an acute bout of exercise in recreational athletes. Foot Ankle Int. 2014;35(2):123–130. [DOI] [PubMed] [Google Scholar]
- 158. Porter MD, Shadbolt B. Randomized controlled trial of accelerated rehabilitation versus standard protocol following surgical repair of ruptured Achilles tendon. ANZ J Surg. 2015;85(5):373–377. [DOI] [PubMed] [Google Scholar]
- 159. Quagliarella L, Sasanelli N, Notarnicola A, Belgiovine G, Moretti L. Comparative functional analysis of two different Achilles tendon surgical repairs. Foot Ankle Int. 2010;31(4):306–315. [DOI] [PubMed] [Google Scholar]
- 160. Raikin SM, Garras DN, Krapchev PV. Achilles tendon injuries in a United States population. Foot Ankle Int. 2013;34(4):475–480. [DOI] [PubMed] [Google Scholar]
- 161. Reilmann H, Forster E, Weinberg A, Bruggemann F, Peukert J. Conservative functional therapy of closed rupture of the Achilles tendon: treatment approach and analysis of results. Unfallchirurg. 1996;99:576–580. [PubMed] [Google Scholar]
- 162. Renninger CH, Kuhn K, Fellars T, Youngblood S, Bellamy J. Operative and nonoperative management of Achilles tendon ruptures in active duty military population. Foot Ankle Int. 2016;37(3):269–273. [DOI] [PubMed] [Google Scholar]
- 163. Richardson LC, Reitman R, Wilson M. Achilles tendon ruptures: functional outcome of surgical repair with a “pull-out” wire. Foot Ankle Int. 2003;24(5):439–443. [DOI] [PubMed] [Google Scholar]
- 164. Richter J, Josten DA, Clasbrummel B, Muhr G. Sportfahigkeit nach konservativ-funktioneller versus operativer Behandlung von akuten Achillessehnenrupturen. Zentralbl Chir. 1994;119:538–544. [PubMed] [Google Scholar]
- 165. Richter J, Pommer A, Hahn M, David A, Muhr G. Moglichkeiten und grenzen der funktionell konservativen therapie akuter Achillessehnenrupturen. Chirurg. 1997;68:517–524. [DOI] [PubMed] [Google Scholar]
- 166. Roberts CP, Palmer S, Vince A, Deliss LJ. Dynamised cast management of Achilles tendon ruptures. Injury. 2001;32(5):423–426. [DOI] [PubMed] [Google Scholar]
- 167. Rozis M, Benetos I, Karampinas P, Polyzois V, Vlamis J, Pneumaticos S. Outcome of percutaneous fixation of acute Achilles tendon ruptures. Foot Ankle Int. 2018;39(6):689–693. [DOI] [PubMed] [Google Scholar]
- 168. Saleh M, Marshall PD, Senior R, MacFarlane A. The Sheffield splint for controlled early mobilisation after rupture of the calcaneal tendon: a prospective, randomised comparison with plaster treatment. J Bone Joint Surg Br. 1992;74(2):206–209. [DOI] [PubMed] [Google Scholar]
- 169. Sandberg OH, Danmark I, Eliasson P, Aspenberg P. Influence of a lower leg brace on traction force in healthy and ruptured Achilles tendons. Muscles Ligaments Tendons J. 2015;5(2):63–67. [PMC free article] [PubMed] [Google Scholar]
- 170. Saper D, Lybrand K, Creevy W, Li X. Using a posterior compartment fasciotomy and paratenon closure in acute Achilles tendon repair. Orthopedics. 2016;39(4):e790–e793. [DOI] [PubMed] [Google Scholar]
- 171. Saw Y, Baltzopoulos V, Lim A, Rostron PKM. Early mobilization Achilles tendon after operative repair of ruptured Achilles tendon. Injury. 1993;24(7):479–484. [DOI] [PubMed] [Google Scholar]
- 172. Saxena A, Ewen B, Maffulli N. Rehabilitation of the operated Achilles tendon: parameters for predicting return to activity. J Foot Ankle Surg. 2011;50(1):37–40. [DOI] [PubMed] [Google Scholar]
- 173. Schäfer D, Regazzoni P, Hintermann B. Frühfunktionelle behandlung der operativ versorgten Achillessehnenruptur. Unfallchirurg. 2002;105(8):699–702. [DOI] [PubMed] [Google Scholar]
- 174. Schepull T, Aspenberg P. Early controlled tension improves the material properties of healing human Achilles tendons after ruptures: a randomized trial. Am J Sports Med. 2013;41:2550–2557. [DOI] [PubMed] [Google Scholar]
- 175. Schepull T, Kvist J, Andersson C, Aspenberg P. Mechanical properties during healing of Achilles tendon ruptures to predict final outcome: a pilot Roentgen stereophotogrammetric analysis in 10 patients. BMC Musculoskelet Disord. 2007;8:116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176. Scott A, Docking S, Vicenzino B, et al. Sports and exercise-related tendinopathies: a review of selected topical issues by participants of the second International Scientific Tendinopathy Symposium (ISTS) Vancouver 2012. Br J Sports Med. 2013;47:536–544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177. Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal S. Practice patterns in the care of acute Achilles tendon ruptures. Bone Joint J. 2017;99(12):1629–1636. [DOI] [PubMed] [Google Scholar]
- 178. Sheth U, Wasserstein D, Jenkinson R, Moineddin R, Kreder H, Jaglal SB. The epidemiology and trends in management of acute Achilles tendon ruptures in Ontario, Canada. Bone Joint J. 2017;99(1):78–86. [DOI] [PubMed] [Google Scholar]
- 179. Solveborn S, Moberg A. Immediate free ankle motion after surgical repair of acute Achilles tendon ruptures. Am J Sports Med. 1994;22(5):607–610. [DOI] [PubMed] [Google Scholar]
- 180. Sorrenti S. Achilles tendon rupture: effect of early mobilization in rehabilitation after surgical repair. Foot Ankle Int. 2006;27(6):407–410. [DOI] [PubMed] [Google Scholar]
- 181. Speck M, Klaue K. Early full weightbearing and functional treatment after surgical repair of acute Achilles tendon rupture. Am J Sports Med. 1998;26(6):789–793. [DOI] [PubMed] [Google Scholar]
- 182. Steele GJ, Harter RA, Ting AJ. Comparison of functional ability following percutaneous and open surgical repairs of acutely ruptured Achilles tendons. J Sport Rehabil. 1993;2:115–127. [Google Scholar]
- 183. Strauss E, Ishak C, Jazrawi L, Sherman O, Rosen J. Operative treatment of acute Achilles tendon ruptures: an institutional review of clinical outcomes. Injury. 2007;38(7):832–838. [DOI] [PubMed] [Google Scholar]
- 184. Suchak A, Bostick G, Beaupre L, Durand D, Jomha N. The influence of early weight-bearing compared with non-weight-bearing after surgical repair of the Achilles tendon. J Bone Joint Surg. 2008;90(9):1876–1883. [DOI] [PubMed] [Google Scholar]
- 185. Swennergren Hansen M, Weisskirchner Barfod K, Tange Kristensen M. Development and reliability of the Achilles tendon length measure and comparison with the Achilles tendon resting angle on patients with an Achilles tendon rupture. Foot Ankle Surg. 2017;23(4):275–280. [DOI] [PubMed] [Google Scholar]
- 186. Tarniţă DN, Tarniţă D, Grecu DC, Calafeteanu DM, Căpitănescu B. New technical procedure involving Achilles tendon rupture treatment through transcutaneous suture. Rom J Morphol Embryol. 2016;57(1):211–214. [PubMed] [Google Scholar]
- 187. Tezeren G, Kuru I. Augmentation vs nonaugmentation techniques for open repairs of Achilles tendon ruptures with early functional treatment: a prospective randomized study. J Sports Sci Med. 2006;5(4):607–614. [PMC free article] [PubMed] [Google Scholar]
- 188. Thermann H, Zwipp H. Achillessehnenruptur. Orthopade. 1989;18:321–335. [PubMed] [Google Scholar]
- 189. Thermann H, Zwipp H, Tscherne H. Functional treatment concept of acute rupture of the Achilles tendon: 2 years results of a prospective randomized study. Unfallchirurg. 1995;98(1):21–32. [PubMed] [Google Scholar]
- 190. Troop RL, Losse GM, Lane JG, Robertson DB, Hastings PS, Howard ME. Early motion after repair of Achilles tendon ruptures. Foot Ankle Int. 1995;16(11):705–709. [DOI] [PubMed] [Google Scholar]
- 191. Twaddle BC, Poon P. Early motion for Achilles tendon ruptures: is surgery important? A randomized, prospective study. Am J Sports Med. 2007;35:2033–2038. [DOI] [PubMed] [Google Scholar]
- 192. Vadalá A, De Carli A, Vulpiani M, et al. Clinical, functional and radiological results of Achilles tenorraphy surgically treated with mini-open technique. J Sports Med Phys Fitness. 2012;52:616–621. [PubMed] [Google Scholar]
- 193. Valkering KP, Aufwerber S, Ranuccio F, Lunini E, Edman G, Ackermann PW. Functional weight-bearing mobilization after Achilles tendon rupture enhances early healing response: a single-blinded randomized controlled trial. Knee Surg Sports Traumatol Arthrosc. 2017;25(6):1807–1816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194. Vavra-Hadžiahmetovic N, Hadžiahmetovic Z, Smajlovic F. Physical therapy in conservative (functional) treatment of acute Achilles tendon rupture. Med Arh. 2000;54(2):121–122. [PubMed] [Google Scholar]
- 195. Walz M, Cramer J, Mollenhoff G, Muhr G. Ultrasonographic monitoring of conservative-functional treatment of rupture of the Achilles tendon. Orthopade. 1993;22(5):317–322. [PubMed] [Google Scholar]
- 196. Weber M, Niemann M, Lanz R, Müller T. Nonoperative treatment of acute rupture of the Achilles tendon: results of a new protocol and comparison with operative treatment. Am J Sports Med. 2003;31(5):685–691. [DOI] [PubMed] [Google Scholar]
- 197. Westin O, Nilsson Helander K, Grävare Silbernagel K, Möller M, Kälebo P, Karlsson J. Acute ultrasonography investigation to predict reruptures and outcomes in patients with an Achilles tendon rupture. Orthop J Sports Med. 2016;4(10):2325967116667920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 198. Williamson PR, Altman DG, Bagley H, et al. The COMET Handbook: version 1.0. Trials. 2017;18(suppl 3):280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 199. Willits K, Amendola A, Bryant D, et al. Operative versus nonoperative treatment of acute Achilles tendon ruptures: a multicenter randomized trial using accelerated functional rehabilitation. J Bone Joint Surg. 2010;92(17):2767–2775. [DOI] [PubMed] [Google Scholar]
- 200. Willy RW, Brorsson A, Powell HC, Willson JD, Tranberg R, Grävare Silbernagel K. Elevated knee joint kinetics and reduced ankle kinetics are present during jogging and hopping after Achilles tendon ruptures. Am J Sports Med. 2017;45(5):1124–1133. [DOI] [PubMed] [Google Scholar]
- 201. Wredmark T, Carlstedt CA. Tendon elongation and muscle function after repair of Achilles tendon rupture. Scand J Med Sci Sports. 1992;2(3):139–142. [Google Scholar]
- 202. Yotsumoto T, Miyamoto W, Uchio Y. Novel approach to repair of acute Achilles tendon rupture: early recovery without postoperative fixation or orthosis. Am J Sports Med. 2010;38:287–292. [DOI] [PubMed] [Google Scholar]
- 203. Zayni R, Coursier R, Zakaria M, et al. Activity level recovery after acute Achilles tendon rupture surgically repaired: a series of 29 patients with a mean follow-up of 46 months. Muscles Ligaments Tendons J. 2017;7(1):69–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204. Zell RA, Santoro VM. Augmented repair of acute Achilles tendon ruptures. Foot Ankle Int. 2000;21(6):469–474. [DOI] [PubMed] [Google Scholar]