Abstract
Background
Clinical variables may correlate with lack of response to treatment (primary resistance) or clinical benefit in patients with clear cell renal cell carcinoma (ccRCC) treated with anti-programmed death 1/ligand one antibodies.
Methods
In this multi-institutional collaboration, clinical characteristics of patients with primary resistance (defined as progression on initial computed tomography scan) were compared to patients with clinical benefit using Two sample t-test and Chi-square test (or Fisher’s Exact test). The Kaplan–Meier method was used to estimate the distribution of progression-free survival (PFS) and overall survival (OS) in all patients and the subsets of patients with clinical benefit or primary resistance. Cox’s regression model was used to evaluate the correlation between survival endpoints and variables of interest. To explore clinical factors in a larger, independent patient sample, The Cancer Genome Atlas (TCGA) was analyzed. RNAseq gene expression data as well as demographic and clinical information were downloaded for primary tumors of 517 patients included within TCGA-ccRCC.
Results
Of 90 patients, 38 (42.2%) had primary resistance and 52 (57.8%) had clinical benefit. Compared with the cohort of patients with initial benefit, primary resistance was more likely to occur in patients with worse ECOG performance status (p = 0.03), earlier stage at diagnosis (p = 0.04), had no prior nephrectomy (p = 0.04) and no immune-related adverse events (irAE) (p = 0.02). In patients with primary resistance, improved OS was significantly correlated with lower International Metastatic RCC Database Consortium risk score (p = 0.02) and lower neutrophil:lymphocyte ratio (p = 0.04). In patients with clinical benefit, improved PFS was significantly associated with increased BMI (p = 0.007) and irAE occurrence (p = 0.02) while improved OS was significantly correlated with overweight BMI (BMI 25–30; p = 0.03) and no brain metastasis (p = 0.005). The cohort TCGA-ccRCC was examined for the correlations between gene expression patterns, clinical factors, and survival outcomes observing associations of T-cell inflammation and angiogenesis signatures with histologic grade, pathologic stage and OS.
Conclusions
Clinical characteristics including performance status, BMI and occurrence of an irAE associate with outcomes in patients with ccRCC treated with immunotherapy. The inverse association of angiogenesis gene signature with ccRCC histologic grade highlight opportunities for adjuvant combination VEGFR2 tyrosine kinase inhibitor and immune-checkpoint inhibition.
Keywords: Renal cell carcinoma, Immune-checkpoint inhibition, Immunotherapy, Biomarkers, BMI
Background
Renal cell carcinoma is eighth in incidence and mortality among all cancers as measured in the Surveillance, Epidemiology, and End Results database [1]. Clear cell renal cell carcinoma (ccRCC) is the most common and well-studied histologic subtype of RCC and carries the highest risk of metastatic spread [2]. Eighty percent of ccRCC have inactivating mutations in the Von Hippel Lindau gene which stabilizes hypoxia inducible factors and leads to overexpression of vascular endothelial growth factor receptor and platelet-derived growth factor receptor which promote angiogenesis, tumor growth and metastasis [3].
Treatment of ccRCC has changed dramatically over a short period of time. Historically ccRCC has been one of a select number of tumors where cytokine therapies such as interleukin-2 or interferon-α have been used to treat metastatic disease [4, 5]. mTOR inhibitors and tyrosine kinase inhibitors (TKI) against VEGF receptor 2 (VEGFR2) developed as disease specific targeted therapies and remain therapeutic standards [6]. More recently immune-checkpoint inhibition (ICI), centered on programmed death-1 (PD-1) or programmed death ligand-1 (PD-L1) as well as cytotoxic T lymphocyte antigen 4 (CTLA4), has become a backbone of therapy. In previously untreated metastatic ccRCC, anti-PD1/L1 antibodies combined with VEGFR2 TKI is emerging [7, 8].
Despite promising activity, many patients have tumors that are refractory to ICI or suffer early progression on treatment. Identifying predictive molecular and clinical markers of resistance is a priority to guide optimal treatment selection. Established biomarkers, such as tumor PD-L1 expression and tumor mutational burden (TMB), have not been demonstrated to have a highly predictive utility in ccRCC [9, 10]. Expression of PD-L1 in ccRCC is somewhat correlated with improved outcomes to ICI however patients with tumors without PD-L1 expression also achieve responses [11–13]. Composite gene expression profiling (GEP) across tumor types has identified gene signatures that associate with treatment response. The T-cell inflamed GEP comprised of IFNγ signaling and T-cell related genes has correlated with treatment response to immunotherapy in multiple tumor types [14–16]. A gene signature of six VEGF-dependent genes validated as a predictive biomarker for anti-VEGF therapy has been used to assess angiogenic activity in ccRCC [17, 18].
Clinical variables may more easily be identified in association with treatment resistance and more favorable outcomes to immunotherapy. ECOG and Karnofsky performance status define functional status of cancer patients and are predictive of outcomes to systemic chemotherapy [19, 20]. The RCC International Metastatic Database Consortium (IDMC) Risk Score defines adverse clinical prognostic risk factors in patients with ccRCC treated with VEGF-targeted therapy [21, 22]. Smoking status and serum albumin correlate with immunotherapy outcomes in some tumors [23]. Increased body-mass index (BMI) was found to correlate with improved outcomes in colorectal and lung cancers as well as immunotherapy response in melanoma and other cancers [24–26]. A prognostic signature incorporating both clinical and genomic variables has been developed in breast cancer [27]. In ccRCC, duration of prior anti-VEGFR2 TKI therapy and neutrophil:lymphocyte ratio (NLR) have been found to be independent predictors of survival [28].
As immunotherapy has become a backbone therapy in the treatment of ccRCC, predictors of lack of response, or primary resistance, are needed. Here we assessed for clinical characteristics that correlate with outcomes in a cohort of patients with ccRCC treated with anti-PD1/PD-L1 and The Cancer Genome Atlas Kidney Renal Clear Cell Carcinoma cohort (TCGA-ccRCC). Recent biomarker analysis found correlation between angiogenesis, T-effector and myeloid inflammatory gene expression and treatment response in ccRCC [18, 29]. VEGF signaling has known immunosuppressive activity and preclinical work has suggested anti-VEGF treatment might enhance efficacy of ICI [30–34]. As such, we interrogated the TCGA cohort with angiogenesis and T-cell inflammation gene signatures and identified clinical, neoplasm histologic grade and stage specific associations that may inform treatment selection and support adjuvant or neo-adjuvant use of ICI and/or VEGFR2-TKI.
Methods
Data collection
We performed an international multi-center data collection from patients with stage IV ccRCC who received at least one dose of anti-PD-1/PD-L1 (pembrolizumab, nivolumab, atezolizumab) between 01/01/2011 and 06/01/2018. The participating centers included the University of Chicago Comprehensive Cancer Center (n = 22), Laura and Isaac Perlmutter Comprehensive Cancer Center at NYU Langone (n = 21), Massey Cancer Center at Virginia Commonwealth University (n = 14), London Health Sciences Centre at Western University, Ontario, Canada (n = 17) and Marqués de Valdecilla University Hospital in Santander, Spain (n = 16). Local institutional review board approval, including waiver of consent where appropriate, was obtained at all participating sites using a master data collection protocol.
Study design
De-identified demographic and clinical variables including but not limited to age, gender, BMI, smoking status, performance status as defined by the Eastern Cooperative Oncology Group (ECOG) were collected. Clinical and laboratory data required for calculation of the RCC IMDC risk score were also collected [21, 22]. Information regarding additional treatments including prior radiation, prior therapies, additional therapies after anti-PD1/L1 treatment and the occurrence of an immune-related adverse event (irAE) were recorded. Clinical outcomes from each center were obtained from their respective electronic medical records with identifiers and dates removed prior to data aggregation.
Radiologic tumor assessment for each patient included computed tomography (CT) scans performed every 8–12 weeks unless otherwise clinically indicated. Patients with either clinical progression or disease progression on first CT evaluation by investigator assessment or death due to cancer prior to first CT evaluation were defined as having primary resistance. Characteristics of patients alive with clinical benefit by investigator assessment on first CT, i.e. those found to not have primary resistance, were then evaluated to identify factors associated with subsequent progression or secondary resistance and survival outcomes.
Statistical analysis
Baseline demographic data was used to generate descriptive statistics. Tabular summaries were presented for overall patient population and those with primary resistance vs. those with clinical benefit. Continuous variables were summarized using descriptive statistics (n, mean, standard deviation, standard error median, minimum, and maximum). Categorical variables were summarized showing the number and percentage (n, %) of patients within each category. Baseline characteristics between patients with primary resistance and those with clinical benefit were compared using Two sample t-test and Chi-square test (or Fisher’s Exact test).
The Kaplan–Meier method was used to estimate the distribution of progression-free survival (PFS) and overall survival (OS) in all patients and the subsets of patients with clinical benefit or primary resistance. PFS was defined as time from start of treatment to progression by investigator assessment or death from any cause. OS was defined as time from the start of treatment until death from any cause. If no event had occurred, patients were censored at their last follow up visit or 6/30/18, whichever came sooner. Cox’s regression model was used to evaluate the correlation between survival endpoints and the variables of interest. Univariable Cox’s model was first implemented to examine the relationship between survival endpoint and each covariate. Covariates with p-value less than 0.10 were then included in the multivariable models, and a backward selection was performed to derive the final multivariable model for PFS and OS. Statistical analyses were done with SAS 9.4. All statistical tests were two-sided and considered significant at p < 0.05.
Analysis of TCGA-ccRCC data set
RNAseq gene expression data (release date January 28, 2016) were downloaded from Broad Institute’s GDAC Firehose website [35] for primary tumor of 517 patients from TCGA Kidney RCC (TCGA-ccRCC) database. Harmonized survival data were extracted from the previously published TCGA Pan-Cancer study [36] for progression-free interval event (PFI, defined as “for patient having new tumor event whether it was a progression of disease, local recurrence, distant metastasis, new primary tumors all sites, or died with the cancer without new tumor event, including cases with a new tumor event whose type is N/A” [36]) and OS. Additional demographic and clinical information were downloaded from Genomic Data Commons data portal (GDC) [37]. All tumor samples were used for analysis.
Bioinformatics analysis
For the TCGA-ccRCC patients, the RSEM [38]—summarized gene level read counts were upper quartile normalized across all tumor samples and log2 transformed. For each tumor, the scores for the T cell-inflamed (Tinfl) or Angiogenesis (Angio) gene signatures were calculated by averaging the expression level of all genes from each signature after centering and scaling across samples for each gene. The probability of survival including PFI and OS were compared between designated groups by log-rank test. The Cox proportional hazard (PH) model was used to evaluate significance of factor of interest in multivariate model with p-values computed by Wald test in function coxph from R library survival (v2.43-3).
Gene expression comparison between groups were performed using two-sided Student’s t-test. For multiple comparisons, p-value was adjusted using Benjamini–Hochberg false discovery rate (FDR) correction [39]. Spearman’s correlation ρ was used for measuring statistical dependence between normalized and log2-transformed expression level of different gene signatures and was applied in 2 biologically relevant sets: one within non-T cell-inflamed plus intermediate and the other within the T cell-inflamed group. p < 0.05 was considered statistically significant. Statistical analysis was performed using R (v3.5.2) and Bioconductor.
Results
Baseline patient characteristics
A total of 90 patients treated at four sites in three different countries (USA, Canada, Spain) with PD1/L1 agents were included. Patients were followed for a median of 13.5 months. Pertinent baseline demographic information is reported in Table 1. Mean age was 66 (range 17–92), 27.8% of patients were female. 48.9% of patients had a smoking history. ECOG was 0 or 1 in 85% of patients. 42 of 44 of patients with Stage I–III disease at diagnosis underwent partial or total nephrectomy within 6 months of diagnosis. 42 (46.7%) patients presented with metastatic disease at diagnosis and 27 of 42 (64%) of patients with Stage IV disease at diagnosis underwent nephrectomy.
Table 1.
Baseline clinical and demographic characteristics
| Characteristic | |
|---|---|
| Median age (range)—year | 66 (17–92) |
| Female gender—no. (%) | 25 (27.8%) |
| Ethnicity—no. (%) | |
| Caucasian | 59 (65%) |
| African American | 8 (9%) |
| Hispanic | 5 (6%) |
| Asian/Pacific Islander | 3 (3%) |
| Other/unknown | 15 (17%) |
| Smoking history—no. (%) | |
| No | 46 (51%) |
| BMI status—no. (%) | |
| Underweight | 2 (2%) |
| Normal | 29 (32%) |
| Overweight | 38 (42%) |
| Obese | 21 (23%) |
| IMDC risk scorea—no. (%) | |
| Favorable | 18 (20%) |
| Intermediate | 59 (65%) |
| Poor | 6 (6%) |
| No. of organs with metastasis—no. (%) | |
| 1 | 8 (9%) |
| > 2 | 73 (81%) |
| Most common sites of metastasis—no. (%) | |
| Lung | 66 (73%) |
| Spine | 31 (34%) |
| Liver | 23 (25%) |
| Brain | 7 (8%) |
| Nephrectomy—no. (%) | 74 (82%) |
| Previous radiotherapy—no. (%) | 52 (58%) |
| ICI line of treatment—no. (%) | |
| First line | 8 (9%) |
| Second line | 43 (48%) |
| Third line | 28 (31%) |
| Fourth or more | 11 (12%) |
aFavorable risk responds to an International Renal Cell Carcinoma Database Consortium (IMDC) score of 0, intermediate risk to a score of 1 or 2, poor risk to a score of 3 to 6
The majority of patients were treated off of any investigative protocol except for ten, including three who were treated with pembrolizumab monotherapy, five with pembrolizumab plus indolamine-dioxygenase inhibitor, one with nivolumab plus ipilimumab and one with nivolumab plus an anti-colony stimulating factor receptor agent. ICI as line of therapy included 8.9%, 47.8% or 43% for first, second or third line and beyond, respectively. Prior treatment for metastatic disease for more than 6 months was present in 60% of patients.
Characteristics of response and post-progression course
Characteristics of response and post-progression course are reported in Table 2. At progression, 31% of patients had new lesions, 29% had growth of existing, 2% had growth of new and existing lesions, and 31% were not recorded. 53 (55%) had additional treatment recorded. Of those patients, 3 pursued hospice. Thirty-one patients (58%) received VEGFR2 TKI monotherapy of which cabozantinib and axitinib were the most commonly used therapies. Eight patients (15%) were placed on an investigative agent in a clinical trial.
Table 2.
Characteristics of response and progression in all patients
| N (%) | |
|---|---|
| Primary resistance | |
| Yes | 38 (42%) |
| No | 52 (58%) |
| New or existing lesion at progression | |
| New | 31 (34%) |
| Existing | 29 (32%) |
| Additional treatment post ICI (n = 53, 58%) | 53 (58%) |
| VEGFR2 TKI containing therapy (n = 39, 74%) | 39 (74%) |
| Cabozantinib | 17 (32%) |
| Axitinib | 9 (17%) |
| VEGFR2 TKI + ICI | 6 (11%) |
| Lenvatinib + everolimus | 2 (5%) |
| Sunitinib | 2 (4%) |
| Lenvatinib | 1 (2%) |
| Pazopanib | 1 (2%) |
| Sorafenib | 1 (2%) |
| Clinical trial, other | 8 (15%) |
| Other (radiation only, hospice) | 3 (6%) |
| Everolimus | 2 (4%) |
| Nivolumab + ipilimumab | 1 (2%) |
| Immune-related adverse events (irAE) | |
| No | 66 (73%) |
| Type of irAEs | |
| Colitis | 8 (33%) |
| Pneumonitis | 5 (21%) |
| Hepatitis | 3 (13%) |
| Dermatitis | 3 (12%) |
| irAEs causing treatment discontinuation | |
| Yes | 13 (54%) |
Immune-related adverse events (irAE) occurred in 24 (27%) patients. Of those patients, the irAE caused treatment discontinuation in 13 (54%). Colitis was the most common irAE occurring in 8 patients (33%). Pneumonitis and hepatitis occurred in 5 (21%) and 3 (13%) of patients respectively. Pyrexia and fatigue were not routinely recorded. irAE grades were not collected. No deaths were reported related to irAEs.
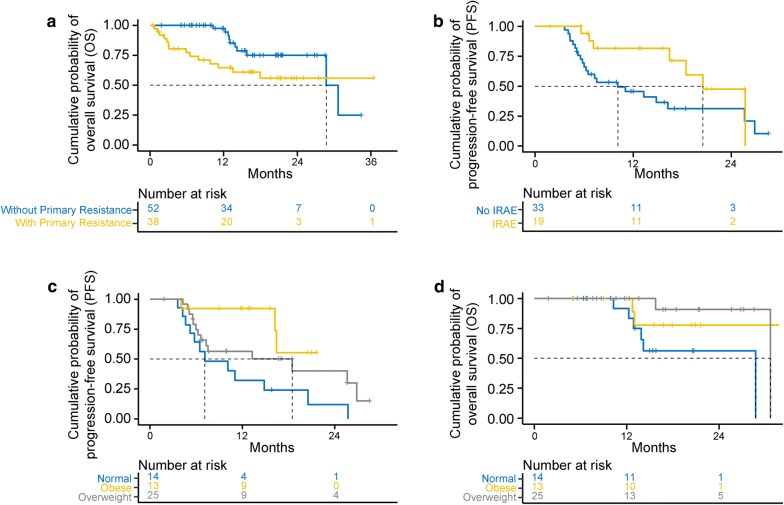
Characteristics of patients more likely to experience primary resistance
Of 90 patients studied, 38 (42%) patients had primary resistance and 52 (58%) of patients did not. By t-test and Chi squared tests, patients with primary resistance were more likely to have a worse ECOG performance status at the start of immunotherapy (p = 0.03), have an earlier stage at diagnosis (p = 0.04), have not undergone nephrectomy (p = 0.04) and not experience an immune-related adverse event (p = 0.02). We failed to observe any other significant difference between two patient cohorts with respect to other demographic, histologic, prior treatment or biochemical characteristics. Patients who experienced primary resistance had worse OS than those with clinical benefit (Fig. 1a).
Fig. 1.
Kaplan-Meier curves depicting survival outcomes. a OS in patients by primary resistance status. b PFS in patients by irAE occurrence. c PFS in patients by BMI status. d OS in patients by BMI status
Survival outcomes in patients with clinical benefit
Multivariable analysis of variables associated with improved outcomes in patients who experienced clinical benefit is presented in Table 3. Factors associated with improved PFS were an occurrence of an irAE (p = 0.02) and increased BMI (p = 0.007) (Fig. 1b, c). No association was observed between PFS and the type of irAE experienced. Improved OS was correlated with overweight BMI (p = 0.03), defined as BMI 25–30, and the absence of brain metastasis (p = 0.005) (Table 4). There was a trend towards improved OS in obese patients, but this did not reach statistical significance (p = 0.07), perhaps due to small sample size. In these patients, ECOG PS, IMDC Risk Score, laboratory parameters such as albumin and NLR did not show correlation with PFS or OS. Higher BMI did not show correlation with the likelihood of experiencing an irAE.
Table 3.
Variables associated with PFS in patients with clinical benefit
| N | Median PFS (in months) | Univariable Analysis | Multivariable Analysis | |||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |||
| Age | 52 | 16.24 | 0.95 (0.91, 1.00) | 0.06 | ||
| BMI | 52 | 16.24 | 0.90 (0.82, 0.98) | 0.02 | 0.87 (0.79, 0.96) | 0.007 |
| Smoking history | ||||||
| No | 27 | 13.28 | 1.00 | Ref | ||
| Yes | 25 | 18.48 | 0.80 (0.39, 1.67) | 0.55 | ||
| Nephrectomy | ||||||
| Total | 44 | 16.24 | Ref | Ref | ||
| Partial | 3 | – | 0.31 (0.04, 2.45) | 0.27 | ||
| None | 5 | 18.48 | 0.83 (0.25, 2.78) | 0.76 | ||
| ICI line of treatment | ||||||
| First line | 5 | – | 1.00 | Ref | ||
| Second line | 23 | 18.48 | 1.73 (0.37, 8.08) | 0.49 | ||
| Third line | 17 | 13.28 | 2.65 (0.54, 13.04) | 0.23 | ||
| Fourth line | 5 | 20.52 | 2.08 (0.32, 13.56) | 0.44 | ||
| > 4 prior treatments | 2 | 25.71 | 0.83 (0.07, 9.45) | 0.88 | ||
| ECOG PS at start of immunotherapy | ||||||
| 0 | 19 | 16.24 | 1.00 | Ref | ||
| 1 or 2 or 3 | 32 | 18.48 | 0.83 (0.38, 1.79) | 0.63 | ||
| Missing | 1 | – | – | – | ||
| IMDC risk score | ||||||
| Favorable | 13 | 16.44 | 1.00 | Ref | ||
| Intermediate | 32 | 14.83 | 1.43 (0.58, 3.53) | 0.44 | ||
| Poor | 3 | 26.86 | 0.29 (0.04, 2.38) | 0.25 | ||
| Occurrence of irAE | ||||||
| No | 33 | 10.13 | 1.00 | Ref | 1.00 | Ref |
| Yes | 19 | 20.52 | 0.42 (0.17, 0.99) | 0.04 | 0.33 (0.13, 0.82) | 0.02 |
Table 4.
Variables associated with OS in patients with clinical benefit
| IMDC risk score | N | Median OS (in months) | Univariable analysis | Multivariable analysis | ||
|---|---|---|---|---|---|---|
| HR (95% CI) | p-value | HR (95% CI) | p-value | |||
| Age | 52 | 28.73 | 1.00 (0.93, 1.08) | 0.94 | ||
| BMI group | ||||||
| Normal | 14 | 28.73 | 1.00 | Ref | 1.00 | Ref |
| Overweight | 25 | 30.67 | 0.19 (0.04, 1.01) | 0.05 | 0.15 (0.03, 0.86) | 0.03 |
| Obese | 13 | – | 0.25 (0.04, 1.41) | 0.12 | 0.19 (0.03, 1.11) | 0.07 |
| Smoking history | ||||||
| No | 27 | 30.67 | 1.00 | Ref | ||
| Yes | 25 | 28.73 | 0.51 (0.14, 1.82) | 0.30 | ||
| Nephrectomy | ||||||
| Total | 44 | 28.73 | Ref | Ref | ||
| Partial | 3 | – | – | 0.99 | ||
| None | 5 | – | 1.25 (0.15, 10.16) | 0.84 | ||
| ICI line of treatment | ||||||
| First line | 5 | – | – | 0.99 | ||
| Second line | 23 | 30.67 | 1.00 | Ref | ||
| Third line | 17 | – | 0.86 (0.21, 3.64) | 0.84 | ||
| Fourth line | 5 | – | 0.88 (0.10, 7.67) | 0.91 | ||
| > 4 prior treatments | 2 | 28.73 | 1.55 (0.15, 15.97) | 0.71 | ||
| ECOG PS at start of immunotherapy | ||||||
| 0 | 19 | 30.67 | 1.00 | Ref | ||
| 1 or 2 or 3 | 32 | 28.73 | 5.96 (0.72, 49.62) | 0.10 | ||
| Missing | 1 | – | – | – | ||
| IMDC risk score | ||||||
| Favorable | 13 | 30.67 | 1.00 | Ref | ||
| Intermediate | 32 | 28.73 | 1.02 (0.25, 4.13) | 0.97 | ||
| Poor | 3 | – | – | 0.99 | ||
| Occurrence of irAE | ||||||
| No | 33 | 30.67 | 1.00 | Ref | ||
| Yes | 19 | 28.73 | 0.80 (0.20, 3.19) | 0.75 | ||
| Prior brain mets | ||||||
| No | 47 | 30.67 | 1.00 | Ref | 1.00 | Ref |
| Yes | 5 | 15.75 | 6.49 (1.53, 27.56) | 0.01 | 9.41 (1.94, 45.71) | 0.005 |
Survival outcomes in patients with primary resistance
Variables associated with overall survival in patients with primary resistance is represented in Table 5. Patients with intermediate IMDC risk score [1, 2] had improved OS compared with those with poor IMDC risk score (> 3) (p = 0.02). Patients with higher pre-treatment NLR had decreased OS (p = 0.04). BMI, smoking history or ECOG performance status did not correlate with survival in these patients.
Table 5.
Variables associated with OS in patients with primary resistance
| Variable | N | Median OS (in months) | Hazard ratio (95% CI) | p-value |
|---|---|---|---|---|
| IMDC score | ||||
| Favorable | 5 | – | – | – |
| Intermediate | 27 | – | 0.14 (0.03, 0.73) | 0.02 |
| Poor | 3 | 2.99 | 1.00 | Ref |
| N/A | 3 | 6.51 | 0.51 (0.06, 4.50) | 0.54 |
| Pre-treatment NLR | 27 | 13.51 | 1.17 (1.00, 1.36) | 0.04 |
Survival outcomes in all patients
In all 90 patients in the cohort, we observed significant correlation between PFS and experiencing clinical benefit and BMI status (Additional file 1: Table S1). OS was correlated with primary resistance status, BMI (or BMI group), ECOG PS at start of immunotherapy and albumin (Additional file 1: Table S2).
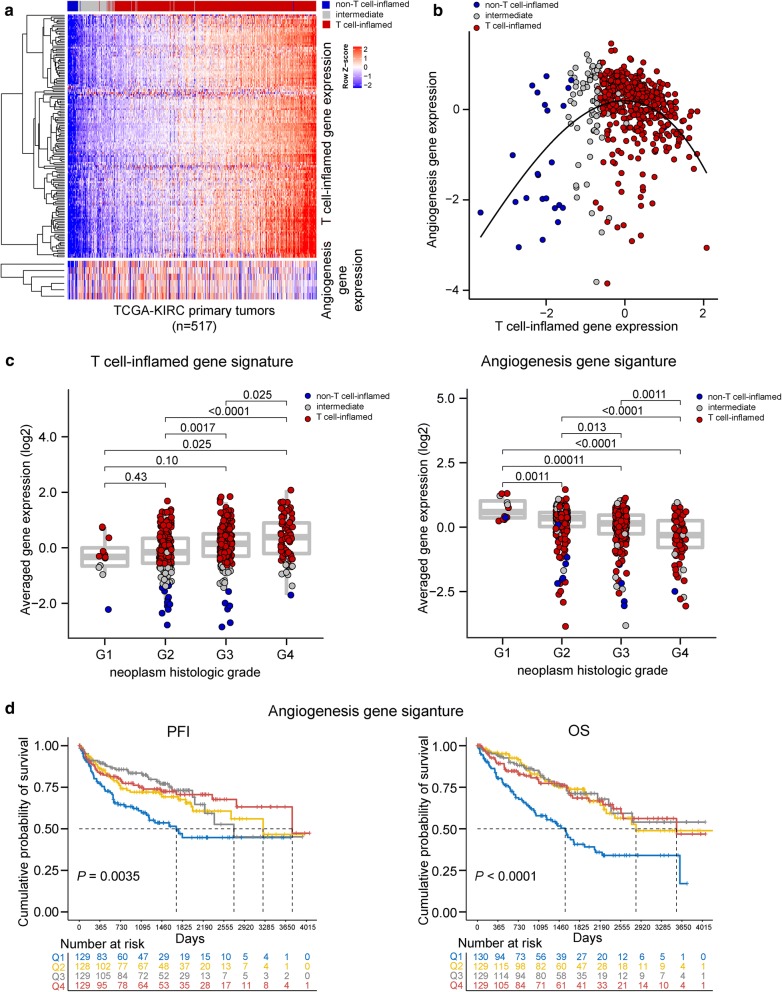
TCGA ccRCC Dataset Analysis
Using a defined T cell-inflamed gene expression signature (Tinfl [40]), we categorized primary tumors of 517 patients from the TCGA-ccRCC database into non-T cell-inflamed (n = 24), T cell-inflamed (n = 419), and intermediate (n = 74) groups following previously described strategies [40]. For each patient, we calculated expression level of the Tinfl signature and an angiogenesis gene signature (Angio [17]) and correlated the two signatures across all tumor samples (Fig. 2a). Within tumors of lower T cell-inflamed gene expression (Fig. 2b, non-T cell-inflamed and intermediate), Tinfl and Angio signatures are positively correlated (Spearman’s ρ = 0.28, p = 0.006) however at higher levels of T cell-inflammation, tumors demonstrate anti-correlation between the two signatures (Spearman’s ρ = − 0.35, p = 1.28e−13) (Fig. 2b). Among the demographic and clinical variables investigated in this study, histologic grade of tumors showed an increase of T cell-inflammation and decrease of angiogenesis signature from grade I to IV (FDR-adjusted p < 0.05, two-sided Student’s t-test) (Fig. 2c). There was a trend to increasing T-cell inflammation signature in later stage disease and more dramatic differences were observed in stage IV relative to stage I (FDR-adjusted p < 0.001). Race showed marginally significant differences for Tinfl (p = 0.034, two-sided Student’s t-test) and Angio (p = 0.069) expression with medium effect size [41, 42] (Cohen’s d = 0.50 for both signatures). Other variables were not significant for either signature.
Fig. 2.
Landscape of T cell-inflamed and angiogenesis gene signature expression and association with survival in TCGA-ccRCC cohort (n = 517). a Primary tumor samples were categorized into non-T cell-inflamed (blue), T cell-inflamed (red), and intermediate (grey) group based on the expression of T cell-inflamed gene signature. Tumors are shown on the column, and sorted from low to high T cell-inflamed gene expression (left to right). Upper heatmap: T cell-inflamed gene expression; bottom heatmap: angiogenesis gene expression. Gene clusters are shown as dendrogram to the left of each heatmap. b Correlation of T cell-inflamed and angiogenesis gene signature expression in tumor groups. c Expression of T cell-inflamed and angiogenesis gene signatures in neoplasm histologic grade I to IV. Grade X samples were excluded (n = 4). e Comparison of survival distributions between patient groups split by quartiles of angiogenesis gene signature expression. PFI = progression-free interval event. OS = overall survival. Q1 to Q4 = expression quartile 1 to 4. Student’s t-test was used in c, followed by BH-FDR correction for multiple testing. Log-rank test was used in d
We also investigated the association between the gene signatures and patients’ survival by splitting patients into four groups based on quartiles of each gene signature. Angio-Q1 patients showed significantly lower PFI and OS compared to Angio-Q2/3/4 (Fig. 2d), and remained significant after adjusting for age and gender. No significant differences in PFI or OS were observed between Tinfl-Q1/2/3/4 patients. Gender is significantly associated with PFI but not OS, with females showing better PFI compared to males (p = 0.012, log-rank test). Age at diagnosis was significantly associated with OS but not PFI, with patients of ≤ 65 years old showing improved OS compared to those of > 65 years old (p = 0.0088, log-rank test). Significant prognostic clinical variables included pathologic stage (PFI, OS), neoplasm histologic grade (PFI, OS), white cell count (PFI), platelet quality (PFI, OS), hemoglobin (PFI, OS), consistent with previously known clinical reports. BMI was not investigated for TCGA-ccRCC cohort due to lack of record in height and weight per patient for the calculation of BMI.
Discussion
Treatment with immune-checkpoint inhibition (ICI) has changed the treatment paradigm in ccRCC however many do not respond to these treatments and no reliable molecular biomarker exists to predict response to ICI in individual patients. PD-L1 immunohistochemistry and TMB have emerged as relevant biomarkers for ICI across many tumors however have not been relevant in ccRCC. Data across tumor types however suggests that some clinical features associate strongly with clinical outcomes to ICI. This study reviewed the course of 90 patients with ccRCC treated with anti-PD1/L1 and identified factors associated with primary resistance including a worse ECOG performance status at the start of ICI, an earlier stage at diagnosis, no prior nephrectomy and no occurrence of an irAE. Overall survival in these patients was correlated with IMDC Risk Score and pre-treatment NLR. In patients with initial benefit, increased BMI and overweight BMI status correlated with improved progression free and overall survival, respectively. Occurrence of an irAE correlated with longer time to progression while brain metastasis correlated decreased OS.
Higher BMI has correlated with a survival advantage to ICI in melanoma and other cancers [24–26, 43]. A recent study demonstrated a survival benefit in patients with higher BMI in ccRCC treated with ICI [44]. The mechanisms by which BMI impact clinical outcomes remain poorly understood. Lalani et al. did not find differences in genomic alteration frequency or tumor mutational burden by BMI status. Hyperadiposity may drive a tumorigenic immune-dysfunction that is more effectively reversed by ICI [45, 46]. However, BMI may not adequately reflect the complexities of body composition. Computerized tomography-based body composition (CTBC) and bioelectrical impedance analysis have defined phenotypes which correlate with outcomes such as high visceral adipose tissue, skeletal muscle density, and sarcopenia [47–49]. Further studies are needed to characterize mechanisms by which these phenotypes overlay with known biomarkers.
Our study demonstrated increased likelihood of response to ICI and improved PFS in patients who experienced and irAE, consistent observations in multiple solid tumors [50, 51]. Studies have demonstrated association between outcomes and incidence of vitiligo and dermatitis in patients with melanoma as well as thyroiditis in NSCLC [52–55]. No specific irAE were associated with improved outcomes in this study. Mechanisms by which irAEs correlate to tumor regression need to be further clarified. One proposed mechanism is cross reactivity of activated T-cells against antigens specific to both tumors and normal tissue, known as antigen sharing [56].
Tissue based biomarkers for ICI across tumor types and especially in ccRCC are evolving. Exploratory biomarkers, such as gene expression profiling suggest that it may be possible to identify sub-populations of patients most likely to benefit to particular treatments. Angiogenesis, T-effector gene (similar to T cell-inflamed) expression signatures associated with outcomes in a recent clinical trial in ccRCC [18, 29]. The Angiolow and T-effhigh GEP subgroups had improved outcomes to ICI whereas the Angiohigh subgroup had worse outcomes to ICI but improved outcomes to VEGFR2 TKI. Our analysis of the TCGA revealed an inverse correlation between angiogenesis and T-cell inflammation signatures in tumors of high T cell-inflamed gene expression, a pattern not observed in non-T cell-inflamed tumors. An inverse association between the angiogenesis signature and histologic grade was demonstrated and a positive association between the T-cell inflammation signature and pathologic stage. This data suggests a suppressive role of angiogenesis on T cell-inflammation and may support further development of VEGFR2-TKI in combination or sequential therapy with ICI in earlier stage ccRCC. In clinical trials in non-metastatic ccRCC, perioperative systemic treatment with VEGFR2-TKI was not shown to increase overall survival versus surgery alone [57–59]. Benefit from ICI in the adjuvant and neoadjuvant setting has been observed in multiple cancers including NSCLC, breast cancer and melanoma and multiple phase III clinical trials evaluating ICI in ccRCC in both adjuvant and neoadjuvant settings are ongoing [60–64] (NCT03024996, NCT03142334, NCT03055013).
Our analysis of the TCGA revealed a positive correlation between T-cell inflammation signature and pathologic stage and in our ICI cohort, patients diagnosed at earlier stage were more likely to experience primary resistance to ICI. It should be noted that patients diagnosed at an earlier stage likely received ICI at time of metastatic recurrence in which there was indeed a longer time from initial diagnosis to treatment than those diagnosed at Stage IV disease (60 mo vs. 3 mo, p < 0.0001). This latency may account for the increased likelihood of resistance. Perhaps metastatic recurrences progress predominately from tumors diagnosed de-novo and recur in non-inflamed, immunosuppressed or immune-exhausted environments. Investigation of primary ccRCC and ccRCC lung metastases demonstrated differential expressions of immunosuppressive molecules between primary and metastatic tumors [65]. Further work to define the immune microenvironment of metastatic recurrences is warranted.
Patients who did not undergo nephrectomy were also more likely to suffer primary resistance. Pre-clinical work has suggested the primary tumor may produce T-cell inhibitory cytokines that divert antitumor immune response away from metastasis [66]. Correlation between the morphologic immune character of the resected primary tumor, such as Teff/Treg ratio, with outcomes to ICI in ccRCC has previously been demonstrated [67]. A recent study found increased response rate in patients who underwent cytoreductive nephrectomy or metastasectomy while receiving ICI [68]. These conclusions highlight the need to further investigate the correlation between the immune character of the resected tumor and treatment outcomes.
While our study sheds light on factors associated with treatment response to immunotherapy and survival in ccRCC, we acknowledge limitations. This is a retrospective study and while we included all identified patients at each institution, a selection bias cannot be excluded. While we aggregated data across 5 centers internationally, we acknowledge that the sample size could be larger which could expand our potential findings. While our report predominately focused on response, we note that our follow-up time potentially did not fully assess long-term survival outcomes in patients receiving immunotherapy. Finally, the TCGA dataset did not record BMI and these patients were not treated with immunotherapy. We alternatively employed gene expression signatures which have been strongly associated with treatment outcomes however this narrows the conclusions that could be reached.
Conclusions
This international, multi-institutional effort supports conclusions that clinical factors, notably BMI and occurrence of an irAE, strongly associate with treatment outcomes in patients with ccRCC treated with ICI. We have identified novel predictors as well as variables that support previous studies, all of which may help guide clinical selection criteria for immunotherapy treatment. On the gene expression level we identified biologically relevant gene signatures including the T-cell inflammation and angiogenesis signatures that associate with histologic grade, pathologic stage and survival. Given the suppressive role of angiogenesis on T cell-inflammation, these data may support further development of VEGFR2-TKI in combination or sequential therapy with ICI in earlier stage ccRCC emphasizing the importance of adjuvant and neo-adjuvant strategies.
Supplementary information
Additional file 1: Table S1. Variables associated with PFS in all patients (N = 90). Table S2. Variables associated with OS in all patients (N = 90).
Acknowledgements
Not applicable.
Disclosures
BWL: none; JJL: Data and Safety Monitoring Board: TTC Oncology, Scientific Advisory Board: 7 Hills, Actym, Akrevia, Alphamab Oncology, Mavu, Pyxis, Springbank, Tempest, Consultancy: Abbvie, Array, Astellas, AstraZeneca, Bayer, Bristol-Myers Squibb, Compugen, EMD Serono, IDEAYA, Immunocore, Incyte, Janssen, Jounce, Leap, Merck, Mersana, Novartis, RefleXion, Spring Bank, Tempest, Vividion, Research Support: (all to institution for clinical trials unless noted) AbbVie, Array (Scientific Research Agreement; SRA), Boston Biomedical, Bristol-Myers Squibb, Celldex, CheckMate (SRA), Compugen, Corvus, EMD Serono, Evelo (SRA), Delcath, Five Prime, FLX Bio, Genentech, Immunocore, Incyte, Leap, MedImmune, Macrogenics, Novartis, Pharmacyclics, Palleon (SRA), Merck, Tesaro, Xencor, Travel: Array, AstraZeneca, Bayer, BeneVir, Bristol-Myers Squibb, Castle, CheckMate, EMD Serono, IDEAYA, Immunocore, Incyte, Janssen, Jounce, Merck, Mersana, NewLink, Novartis, RefleXion, Patents: (both provisional) Serial #15/612,657 (Cancer Immunotherapy), PCT/US18/36052 (Microbiome Biomarkers for Anti-PD-1/PD-L1 Responsiveness: Diagnostic, Prognostic and Therapeutic Uses Thereof).
Authors’ contributions
All authors identified and collected patient data for analysis. PL, RB performed all major statistical analysis of the data. BWL, JJL, PL and RB interpreted data and contributed in writing the manuscript. All authors read and approved the final manuscript.
Funding
JJL: Department of Defense Career Development Award (W81XWH-17-1-0265), the Arthur J Schreiner Family Melanoma Research Fund, the J. Edward Mahoney Foundation Research Fund, Brush Family Immunotherapy Research Fund and Buffet Fund for Cancer Immunotherapy.
Availability of data and materials
The datasets generated and/or analyzed during the current study are not publicly available due to personal health information protection standards but are available from the corresponding author on reasonable request. TCGA datasets are publicly available on Broad Institute’s GDAC Firehose website, GDC data portal, and relevant publications as described in “Methods”.
Ethics approval and consent to participate
Local institutional review board approval, including waiver of consent where appropriate, was obtained at all participating sites using a master data collection protocol.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary information accompanies this paper at 10.1186/s12967-019-02144-7.
References
- 1.Cancer Survival Statistics, 2008–2014, Surveillance, Epidemiology, and End Results (SEER) Program, National Cancer Institute, Bethesda, MD [Internet]; 2008–2014. http://www.seer.cancer.gov.
- 2.Leibovich BC, Lohse CM, Crispen PL, Boorjian SA, Thompson RH, Blute ML, et al. Histological subtype is an independent predictor of outcome for patients with renal cell carcinoma. J Urol. 2010;183(4):1309–1315. doi: 10.1016/j.juro.2009.12.035. [DOI] [PubMed] [Google Scholar]
- 3.Gnarra JR, Tory K, Weng Y, Schmidt L, Wei MH, Li H, et al. Mutations of the VHL tumour suppressor gene in renal carcinoma. Nat Genet. 2019;7(1):85. doi: 10.1038/ng0594-85. [DOI] [PubMed] [Google Scholar]
- 4.McDermott DF, Regan MM, Clark JI, Flaherty LE, Weiss GR, Logan TF, et al. Randomized phase III trial of high-dose interleukin-2 versus subcutaneous interleukin-2 and interferon in patients with metastatic renal cell carcinoma. J Clin Oncol. 2005;23(1):133–141. doi: 10.1200/JCO.2005.03.206. [DOI] [PubMed] [Google Scholar]
- 5.Itsumi M, Tatsugami K. Immunotherapy for renal cell carcinoma. Clin Dev Immunol. 2010 doi: 10.1155/2010/284581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Motzer RJ, Hutson TE, Tomczak P, Michaelson MD, Bukowski RM, Rixe O, et al. Sunitinib versus interferon alfa in metastatic renal-cell carcinoma. N Engl J Med. 2009 doi: 10.1056/NEJMoa065044. [DOI] [PubMed] [Google Scholar]
- 7.Motzer RJ, Tannir NM, McDermott DF, Aren Frontera O, Melichar B, Choueiri TK, et al. Nivolumab plus ipilimumab versus sunitinib in advanced renal-cell carcinoma. N Engl J Med. 2018;378(14):1277–1290. doi: 10.1056/NEJMoa1712126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rini BI, Plimack ER, Stus V, Gafanov R, Hawkins R, Nosov D, et al. Pembrolizumab plus axitinib versus sunitinib for advanced renal-cell carcinoma. N Engl J Med. 2019;380(12):1116–1127. doi: 10.1056/NEJMoa1816714. [DOI] [PubMed] [Google Scholar]
- 9.Pignon J-C, Jegede O, Mahoney KM, Moreira RB, Novak J, Conen H, et al. Impact of immune checkpoint protein expression in tumor cells and tumor infiltrating CD8+ T cells on clinical benefit from PD-1 blockade in metastatic clear cell renal cell carcinoma (mccRCC) J Clin Oncol. 2017;35(6_suppl):477. doi: 10.1200/JCO.2017.35.6_suppl.477. [DOI] [Google Scholar]
- 10.Zhu J, Armstrong AJ, Friedlander TW, Kim W, Pal SK, George DJ, et al. Biomarkers of immunotherapy in urothelial and renal cell carcinoma: PD-L1, tumor mutational burden, and beyond. J ImmunoTher Cancer. 2018;6(1):4. doi: 10.1186/s40425-018-0314-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Herbst RS, Soria JC, Kowanetz M, Fine GD, Hamid O, Gordon MS, et al. Predictive correlates of response to the anti-PD-L1 antibody MPDL3280A in cancer patients. Nature. 2014;515(7528):563–567. doi: 10.1038/nature14011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maia MC, Almeida L, Bergerot PG, Dizman N, Pal SK. Relationship of tumor mutational burden (TMB) to immunotherapy response in metastatic renal cell carcinoma (mRCC) J Clin Oncol. 2018;36(6_suppl):662. doi: 10.1200/JCO.2018.36.6_suppl.662. [DOI] [Google Scholar]
- 13.Yarchoan M, Hopkins A, Jaffee EM. Tumor mutational burden and response rate to PD-1 inhibition. N Engl J Med. 2017;377(25):2500–2501. doi: 10.1056/NEJMc1713444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Harlin H, Meng Y, Peterson AC, Zha Y, Tretiakova M, Slingluff C, et al. Chemokine expression in melanoma metastases associated with CD8+ T-cell recruitment. Cancer Res. 2009;69(7):3077–3085. doi: 10.1158/0008-5472.CAN-08-2281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ribas A, Robert C, Hodi FS, Wolchok JD, Joshua AM, Hwu W-J, et al. Association of response to programmed death receptor 1 (PD-1) blockade with pembrolizumab (MK-3475) with an interferon-inflammatory immune gene signature. J Clin Oncol. 2015;33(15_suppl):3001. doi: 10.1200/jco.2015.33.15_suppl.3001. [DOI] [Google Scholar]
- 16.Ayers M, Lunceford J, Nebozhyn M, Murphy E, Loboda A, Kaufman DR, et al. IFN-gamma-related mRNA profile predicts clinical response to PD-1 blockade. J Clin Invest. 2017;127(8):2930–2940. doi: 10.1172/JCI91190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Brauer MJ, Zhuang G, Schmidt M, Yao J, Wu X, Kaminker JS, et al. Identification and analysis of in vivo VEGF downstream markers link VEGF pathway activity with efficacy of anti-VEGF therapies. Clin Cancer Res. 2013;19(13):3681–3692. doi: 10.1158/1078-0432.CCR-12-3635. [DOI] [PubMed] [Google Scholar]
- 18.McDermott DF, Huseni MA, Atkins MB, Motzer RJ, Rini BI, Escudier B, et al. Clinical activity and molecular correlates of response to atezolizumab alone or in combination with bevacizumab versus sunitinib in renal cell carcinoma. Nat Med. 2018;24(6):749–757. doi: 10.1038/s41591-018-0053-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Oken MM, Creech RH, Tormey DC, Horton J, Davis TE, McFadden ET, et al. Toxicity and response criteria of the Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5(6):649–655. doi: 10.1097/00000421-198212000-00014. [DOI] [PubMed] [Google Scholar]
- 20.Buccheri G, Ferrigno D, Tamburini M. Karnofsky and ECOG performance status scoring in lung cancer: a prospective, longitudinal study of 536 patients from a single institution. Eur J Cancer. 1996;32a(7):1135–1141. doi: 10.1016/0959-8049(95)00664-8. [DOI] [PubMed] [Google Scholar]
- 21.Heng DY, Xie W, Regan MM, Warren MA, Golshayan AR, Sahi C, et al. Prognostic factors for overall survival in patients with metastatic renal cell carcinoma treated with vascular endothelial growth factor-targeted agents: results from a large, multicenter study. J Clin Oncol. 2009;27(34):5794–5799. doi: 10.1200/JCO.2008.21.4809. [DOI] [PubMed] [Google Scholar]
- 22.Ko JJ, Xie W, Kroeger N, Lee JL, Rini BI, Knox JJ, et al. The International Metastatic Renal Cell Carcinoma Database Consortium model as a prognostic tool in patients with metastatic renal cell carcinoma previously treated with first-line targeted therapy: a population-based study. Lancet Oncol. 2015;16(3):293–300. doi: 10.1016/S1470-2045(14)71222-7. [DOI] [PubMed] [Google Scholar]
- 23.Shah S, Wood K, Labadie B, Won B, Brisson R, Karrison T, et al. Clinical and molecular features of innate and acquired resistance to anti-PD-1/PD-L1 therapy in lung cancer. Oncotarget. 2018;9:4375–4384. doi: 10.18632/oncotarget.23315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.McQuade JL, Daniel CR, Hess KR, Mak C, Wang DY, Rai RR, et al. Association of body-mass index and outcomes in patients with metastatic melanoma treated with targeted therapy, immunotherapy, or chemotherapy: a retrospective, multicohort analysis. Lancet Oncol. 2018;19(3):310–322. doi: 10.1016/S1470-2045(18)30078-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Richtig G, Hoeller C, Wolf M, Wolf I, Rainer BM, Schulter G, et al. Body mass index may predict the response to ipilimumab in metastatic melanoma: an observational multi-centre study. PLoS ONE. 2018;13(10):e0204729. doi: 10.1371/journal.pone.0204729. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cortellini A, Bersanelli M, Buti S, Cannita K, Santini D, Perrone F, et al. A multicenter study of body mass index in cancer patients treated with anti-PD-1/PD-L1 immune checkpoint inhibitors: when overweight becomes favorable. J Immunother Cancer. 2019;7(1):57. doi: 10.1186/s40425-019-0527-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Fan C, Prat A, Parker JS, Liu Y, Carey LA, Troester MA, et al. Building prognostic models for breast cancer patients using clinical variables and hundreds of gene expression signatures. BMC Med Genomics. 2011;4(1):3. doi: 10.1186/1755-8794-4-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Jeyakumar G, Kim S, Bumma N, Landry C, Silski C, Suisham S, et al. Neutrophil lymphocyte ratio and duration of prior anti-angiogenic therapy as biomarkers in metastatic RCC receiving immune checkpoint inhibitor therapy. J Immunother Cancer. 2017;5(1):82. doi: 10.1186/s40425-017-0287-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Choueiri TK, Albiges L, Haanen JBAG, Larkin JMG, Uemura M, Pal SK, et al. Biomarker analyses from JAVELIN Renal 101: avelumab + axitinib (A + Ax) versus sunitinib (S) in advanced renal cell carcinoma (aRCC) J Clin Oncol. 2019 doi: 10.1200/JCO.2019.37.15_suppl.101. [DOI] [Google Scholar]
- 30.Gabrilovich DI, Chen HL, Girgis KR, Cunningham HT, Meny GM, Nadaf S, et al. Production of vascular endothelial growth factor by human tumors inhibits the functional maturation of dendritic cells. Nat Med. 1996;2(10):1096–1103. doi: 10.1038/nm1096-1096. [DOI] [PubMed] [Google Scholar]
- 31.Bergers G, Benjamin LE. Tumorigenesis and the angiogenic switch. Nat Rev Cancer. 2003;3(6):401–410. doi: 10.1038/nrc1093. [DOI] [PubMed] [Google Scholar]
- 32.Hicklin DJ, Ellis LM. Role of the vascular endothelial growth factor pathway in tumor growth and angiogenesis. J Clin Oncol. 2005;23(5):1011–1027. doi: 10.1200/JCO.2005.06.081. [DOI] [PubMed] [Google Scholar]
- 33.Kusmartsev S, Eruslanov E, Kübler H, Tseng T, Sakai Y, Su Z, et al. Oxidative stress regulates expression of VEGFR1 in myeloid cells: link to tumor-induced immune suppression in renal cell carcinoma. J Immunol. 2008 doi: 10.4049/jimmunol.181.1.346. [DOI] [PubMed] [Google Scholar]
- 34.Wallin JJ, Bendell JC, Funke R, Sznol M, Korski K, Jones S, et al. Atezolizumab in combination with bevacizumab enhances antigen-specific T-cell migration in metastatic renal cell carcinoma. Nat Commun. 2016;7:12624. doi: 10.1038/ncomms12624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Broad GDAC Firehose. Broad GDAC Firehose, Broad Institute of MIT & Harvard. 2016. https://gdac.broadinstitute.org/.
- 36.Liu J, Lichtenberg T, Hoadley KA, Poisson LM, Lazar AJ, Cherniack AD, et al. An integrated TCGA pan-cancer clinical data resource to drive high-quality survival outcome analytics. Cell. 2018;173(2):400–16 e11. doi: 10.1016/j.cell.2018.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Genomic Data Commons data portal (GDC). https://portal.gdc.cancer.gov.
- 38.Li B, Dewey CN. RSEM: accurate transcript quantification from RNA-Seq data with or without a reference genome. BMC Bioinformatics. 2011;12(1):323. doi: 10.1186/1471-2105-12-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Benjamini Y, Drai D, Elmer G, Kafkafi N, Golani I. Controlling the false discovery rate in behavior genetics research. Behav Brain Res. 2001;125(1–2):279–284. doi: 10.1016/S0166-4328(01)00297-2. [DOI] [PubMed] [Google Scholar]
- 40.Spranger S, Luke JJ, Bao R, Zha YY, Hernandez KM, Li Y, et al. Density of immunogenic antigens does not explain the presence or absence of the T-cell-inflamed tumor microenvironment in melanoma. Proc Natl Acad Sci USA. 2016;113(48):E7759–E7768. doi: 10.1073/pnas.1609376113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York: Routledge Academic; 1988. [Google Scholar]
- 42.Lakens D. Calculating and reporting effect sizes to facilitate cumulative science: a practical primer for t-tests and ANOVAs. Front Psychol. 2013;4:863. doi: 10.3389/fpsyg.2013.00863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Albiges L, Hakimi AA, Xie W, McKay RR, Simantov R, Lin X, et al. Body mass index and metastatic renal cell carcinoma: clinical and biological correlations. J Clin Oncol. 2016;34:3655–3663. doi: 10.1200/JCO.2016.66.7311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lalani AA, Bakouny Z, Farah S, et al. 976P Efficacy of immune checkpoint inhibitors (ICI) and genomic alterations by body mass index (BMI) in advanced renal cell carcinoma (RCC) Ann Oncol. 2019;30(5):mdz249-072. doi: 10.1093/annonc/mdz249.072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Iyengar NM, Gucalp A, Dannenberg AJ, Hudis CA. Obesity and cancer mechanisms: tumor microenvironment and inflammation. J Clin Oncol. 2016;34:4270–4276. doi: 10.1200/JCO.2016.67.4283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee JY, Sohn KH, Rhee SH, Hwang D. Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem. 2001;276(20):16683–16689. doi: 10.1074/jbc.M011695200. [DOI] [PubMed] [Google Scholar]
- 47.Malietzis G, Aziz O, Bagnall NM, Johns N, Fearon KC, Jenkins JT. The role of body composition evaluation by computerized tomography in determining colorectal cancer treatment outcomes: a systematic review. Eur J Surg Oncol. 2015;41(2):186–196. doi: 10.1016/j.ejso.2014.10.056. [DOI] [PubMed] [Google Scholar]
- 48.Young A, Quach HT, Davis EJ, Moslehi J, Williams GR, Johnson DB. Impact of body composition on outcomes from anti-programmed death-1 (PD-1) treatment. J Clin Oncol. 2019 doi: 10.1200/JCO.2019.37.15_suppl.9516. [DOI] [Google Scholar]
- 49.Naik GS, Waikar SS, Johnson AEW, Buchbinder EI, Haq R, Hodi FS, et al. Complex inter-relationship of body mass index, gender and serum creatinine on survival: exploring the obesity paradox in melanoma patients treated with checkpoint inhibition. J ImmunoTher Cancer. 2019;7(1):89. doi: 10.1186/s40425-019-0512-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Elias R, Yan F, Singla N, Levonyack N, Formella J, Christie A, et al. Immune-related adverse events are associated with improved outcomes in ICI-treated renal cell carcinoma patients. J Clin Oncol. 2019 doi: 10.1200/JCO.2019.37.7_suppl.645. [DOI] [Google Scholar]
- 51.Morehouse C, Abdullah SE, Gao C, Dar MM, Ranade K, Higgs BW. Early incidence of immune-related adverse events (irAEs) predicts efficacy in patients (pts) with solid tumors treated with immune-checkpoint inhibitors (ICIs) J Clin Oncol. 2019 doi: 10.1200/JCO.2019.37.15_suppl.2563. [DOI] [Google Scholar]
- 52.Freeman-Keller M, Kim Y, Cronin H, Richards A, Gibney G, Weber JS. Nivolumab in resected and unresectable metastatic melanoma: characteristics of immune-related adverse events and association with outcomes. Clin Cancer Res. 2016;22(4):886–894. doi: 10.1158/1078-0432.CCR-15-1136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Haratani K, Hayashi H, Chiba Y, Kudo K, Yonesaka K, Kato R, et al. Association of immune-related adverse events with nivolumab efficacy in non–small-cell lung cancer. JAMA Oncol. 2018;4(3):374–378. doi: 10.1001/jamaoncol.2017.2925. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ishihara H, Takagi T, Kondo T, Homma C, Tachibana H, Fukuda H, et al. Association between immune-related adverse events and prognosis in patients with metastatic renal cell carcinoma treated with nivolumab. Urol Oncol. 2019 doi: 10.1016/j.urolonc.2019.03.003. [DOI] [PubMed] [Google Scholar]
- 55.Osorio JC, Ni A, Chaft JE, Pollina R, Kasler MK, Stephens D, et al. Antibody-mediated thyroid dysfunction during T-cell checkpoint blockade in patients with non-small-cell lung cancer. Ann Oncol. 2017;28(3):583–589. doi: 10.1093/annonc/mdw640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Ali OH, Diem S, Markert E, Jochum W, Kerl K, French LE, et al. Characterization of nivolumab-associated skin reactions in patients with metastatic non-small cell lung cancer. Oncoimmunology. 2016 doi: 10.1080/2162402X.2016.1231292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ravaud A, Motzer RJ, Pandha HS, George DJ, Pantuck AJ, Patel A, et al. Adjuvant sunitinib in high-risk renal-cell carcinoma after nephrectomy. N Engl J Med. 2016 doi: 10.1056/NEJMoa1611406. [DOI] [PubMed] [Google Scholar]
- 58.Haas NB, Manola J, Uzzo RG, Atkins MB, Wilding G, Pins M, et al. Initial results from ASSURE (E2805): adjuvant sorafenib or sunitinib for unfavorable renal carcinoma, an ECOG-ACRIN-led, NCTN phase III trial. J Clin Oncol. 2017 doi: 10.1200/jco.2015.33.7_suppl.403. [DOI] [Google Scholar]
- 59.Harshman LC, Xie W, Moreira RB, Bosse D, Ruiz Ares GJ, Sweeney CJ, et al. Evaluation of disease-free survival as an intermediate metric of overall survival in patients with localized renal cell carcinoma: a trial-level meta-analysis. Cancer. 2018;124(5):925–933. doi: 10.1002/cncr.31154. [DOI] [PubMed] [Google Scholar]
- 60.Forde PM, Smith KN, Chaft JE, Hellmann M, Merghoub T, Wolchok JD, et al. NSCLC, early stage neoadjuvant anti-PD1, nivolumab, in early stage resectable non-small-cell lung cancer. Ann Oncol. 2019 doi: 10.1093/annonc/mdw435.38. [DOI] [Google Scholar]
- 61.Nanda R, Liu MC, Yau C, Asare S, Hylton N, Veer LVt, et al. Pembrolizumab plus standard neoadjuvant therapy for high-risk breast cancer (BC): results from I-SPY 2. J Clin Oncol. 2017 doi: 10.1200/JCO.2017.35.15_suppl.506. [DOI] [Google Scholar]
- 62.Blank CU, Rozeman EA, Fanchi LF, Sikorska K, Wiel Bvd, Kvistborg P, et al. Neoadjuvant versus adjuvant ipilimumab plus nivolumab in macroscopic stage III melanoma. Nat Med. 2018;24(11):1655. doi: 10.1038/s41591-018-0198-0. [DOI] [PubMed] [Google Scholar]
- 63.Amaria RN, Reddy SM, Tawbi HA, Davies MA, Ross MI, Glitza IC, et al. Neoadjuvant immune checkpoint blockade in high-risk resectable melanoma. Nat Med. 2018;24(11):1649. doi: 10.1038/s41591-018-0197-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Harshman LC, Puligandla M, Haas NB, Allaf M, Drake CG, McDermott DF, et al. PROSPER: a phase III randomized study comparing perioperative nivolumab (nivo) versus observation in patients with renal cell carcinoma (RCC) undergoing nephrectomy (ECOG-ACRIN 8143) J Clin Oncol. 2019 doi: 10.1200/JCO.2019.37.15_suppl.TPS4597. [DOI] [Google Scholar]
- 65.Giraldo NA, Becht E, Pagès F, Skliris G, Verkarre V, Vano Y, et al. Orchestration and prognostic significance of immune checkpoints in the microenvironment of primary and metastatic renal cell cancer. Clin Cancer Res. 2015 doi: 10.1158/1078-0432.CCR-14-2926. [DOI] [PubMed] [Google Scholar]
- 66.Rosenberg SA, Yang JC, White DE, Steinberg SM. Durability of complete responses in patients with metastatic cancer treated with high-dose interleukin-2: identification of the antigens mediating response. Ann Surg. 1998;228(3):307–319. doi: 10.1097/00000658-199809000-00004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Ghatalia P, Gordetsky J, Kuo F, Dulaimi E, Cai KQ, Devarajan K, et al. Prognostic impact of immune gene expression signature and tumor infiltrating immune cells in localized clear cell renal cell carcinoma. J ImmunoTher Cancer. 2019;7(1):139. doi: 10.1186/s40425-019-0621-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gao J, Karam JA, Tannir NM, Slack R, Ahrar K, Rao P, et al. A pilot randomized study evaluating nivolumab (nivo) or nivo + bevacizumab (bev) or nivo + ipilimumab (ipi) in patients with metastatic renal cell carcinoma (MRCC) eligible for cytoreductive nephrectomy (CN), metastasectomy (MS) or post-treatment biopsy (Bx) J Clin Oncol. 2018 doi: 10.1200/JCO.2018.36.15_suppl.4520. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Additional file 1: Table S1. Variables associated with PFS in all patients (N = 90). Table S2. Variables associated with OS in all patients (N = 90).
Data Availability Statement
The datasets generated and/or analyzed during the current study are not publicly available due to personal health information protection standards but are available from the corresponding author on reasonable request. TCGA datasets are publicly available on Broad Institute’s GDAC Firehose website, GDC data portal, and relevant publications as described in “Methods”.