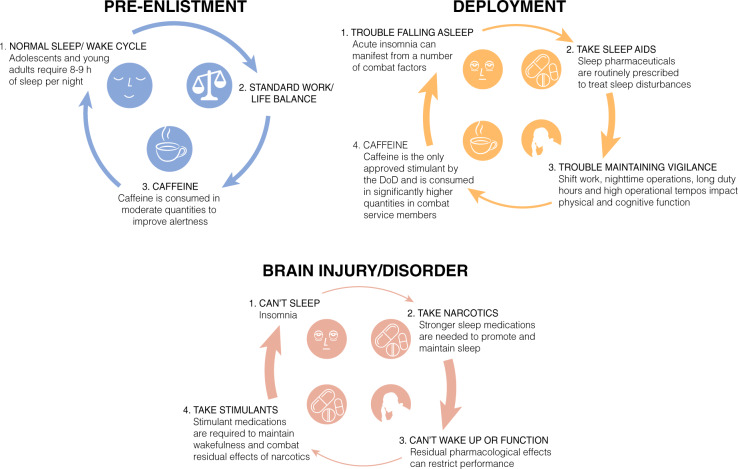
Fig. 1.
Three sleep/wake scenarios are represented based on discussion throughout the manuscript. 1. As illustrated in blue, enlistees generally join the military with normal sleep/wake habits that must rapidly transition to an environment where restricted and fragmented sleep is the norm. 2. Upon deployment, as shown in orange, a number of precipitating factors can cause acute insomnia that require prescription sleep aids to help service members fall asleep. Residual pharmaceutical effects, combined with long duty hours and irregular sleep schedules, result in statistically higher amounts of caffeine intake to maintain alertness and performance. If taken at the wrong time, the awake-promoting effects of caffeine can cause further sleep disruptions and prevent restorative sleep during an already limited sleep window. This feed-forward cycle can necessitate service members being prescribed an increasingly potent sleep aid to overcome the stimulant effects, further necessitating stimulants to transition to wakefulness and maintain vigilance throughout subsequent duty hours, as illustrated by the increasing thickness of the arrows in the cycle. 3. Following injury or diagnosis of neurological disorder, as shown in red, persistent insomnia occurs in a large number of service members. Stronger narcotic sleep aids are routinely prescribed to overcome insomnia, creating a stronger dependence on pharmacology to drive sleep/wake states, as depicted by the even thicker red arrows within the cycle