Abstract
Purpose
to report the presence of a new structural optical coherence tomography (OCT) finding, namely subretinal pseudocysts, in a patient affected by diabetic retinopathy (DR).
Observations
A 52-year-old man affected by type 2 diabetes from 10 years was referred to our department complaining of a visual decline in both eyes. Best corrected visual acuity was 20/100 and 20/80 in the right and left eye, respectively. Fundus examination, fluorescein angiography, and structural OCT revealed the presence of a proliferative DR with diabetic macular edema in both eyes. Interestingly, structural OCT showed subretinal pseudocystic spaces inside the subretinal fluid of the macular neuroretinal detachment.
Conclusions and importance
Subretinal pseudocysts are a new structural OCT entity. We reported for the first time the evidence that pseudocysts may develop in the subretinal space in a case of diabetic macular edema.
Keywords: Diabetic macular edema, Diabetic retinopathy, Optical coherence tomography, Optical coherence tomography angiography, Subretinal pseudocysts
1. Introduction
Retinal cystoid spaces were previously described as intraretinal spaces, usually located in the inner nuclear layer and Henle's fiber layer but also in the ganglion cell layer.1 The anatomic location of cystoid spaces in regard to the Müller cells, if intracellular or extracellular, is still controversy. In this study, we reported the presence of a new structural optical coherence tomography (OCT) finding, namely subretinal pseudocysts, in a patient affected by treatment-naïve proliferative diabetic retinopathy with diabetic macular edema (DME).
The study protocol complied with the tenets of the Declaration of Helsinki. Written informed consent was obtained from the individual participant to publish the collected data, and it was approved by the Local Institutional Review Board (IRB of San Raffaele Hospital, Milan, Italy). In this case, we followed the EQUATOR network CARE guidelines2 for case reports.
The clinical records of the patient were reviewed, including patients' demographic data, ocular clinical findings, structural spectral-domain OCT (Spectralis & HRA; Heidelberg Engineering, Heidelberg, Germany) and Swept-Source OCT-Angiography (OCT-A; PLEX® Elite 9000, Carl Zeiss Meditec Inc.,Dublin, CA, USA) examinations.
2. Case report
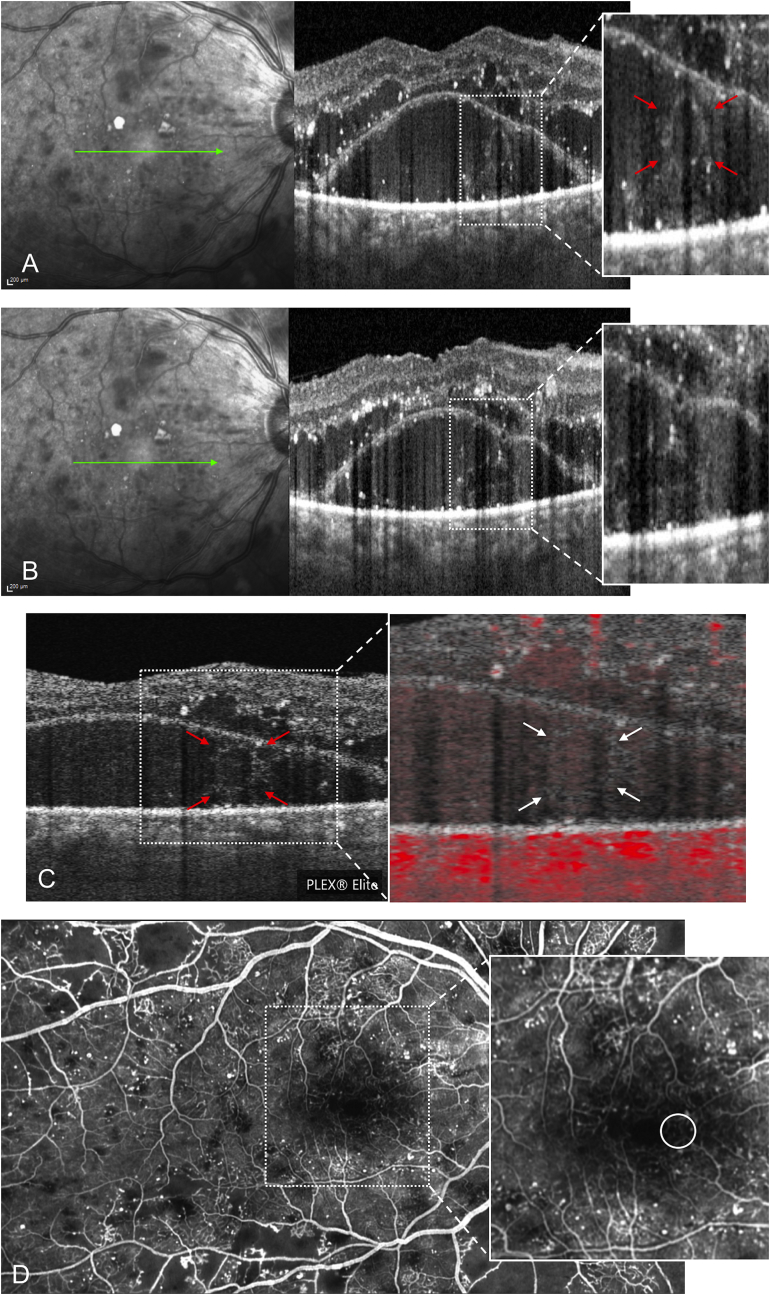
A 52-year-old man affected by type 2 diabetes from 10 years was referred to our department complaining of a visual decline in both eyes from several months. He was affected by hypertension controlled by medications. He had no other relevant past conditions and/or past ocular impairment. Best corrected visual acuity was 20/100 in the right eye (RE) (refraction +1.50 diopters) and 20/80 in the left eye (LE) (refraction +1.00 diopters). Intraocular pressure was 17 mmHg in both eyes, and he was phakic. The patient was not affected by rubeosis iridis, and the anterior segment evaluation was unremarkable. Fundus examination, fluorescein angiography (FA), and structural OCT revealed the presence of a proliferative DR with DME in both eyes. Interestingly, structural OCT showed the appearance of cystoid spaces inside the subretinal fluid of the macular neuroretinal detachment of the right eye (Fig. 1A–B). Swept-Source OCT-A demonstrated the presence of weak flow signal inside the pseudocystic space, attributable to a Suspended Scattering Particles in Motion (SSPiM) effect (Fig. 1C).3 FA revealed no specific finding in the correspondence of subretinal pseudocyst (Fig. 1D).
Fig. 1.
(A) Combined infrared reflectance and structural optical coherence tomography (OCT) B-scans passing through the fovea showing the presence of a cystoid spaces inside the subretinal fluid of the macular neuroretinal detachment of the right eye (red arrows). The subretinal pseudocysts appear surrounded by a hyperreflective edge with a grey material inside (A) and seem to imprint the retinal pigment epithelium (B). (C) OCT-angiography b-scan without and with flow showing the presence of a weak flow signal inside the cystoid space (white arrows), attributable to a Suspended Scattering Particles in Motion (SSPiM) effect. (D) Fluorescein angiography (FA) showing leakage due to the breaking of the blood-retinal barrier, retinal ischemia, microaneurysms and vascular abnormalities; no specific finding was shown by FA in the correspondence of subretinal pseudocyst (white circle). (For interpretation of the references to colour in this figure legend, the reader is referred to the Web version of this article.)
3. Discussion
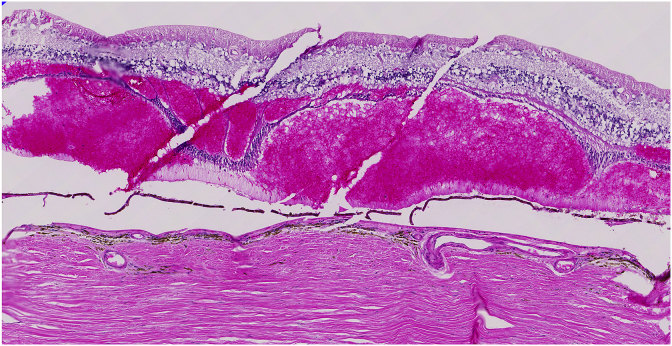
The new structural OCT finding here reported, namely “subretinal pseudocysts”, in a DME patient, suggests that cystoid spaces may develop not only inside the neuroretina but also in the subretinal space. Whether the cysts are intracellular or extracellular in regard to the Müller cells is still debated, but it is well known that Müller cells play a fundamental role in controlling homeostasis of water and ionic concentrations in the interstitial area.1 Edwards et al.4 has shown that Müller cells could migrate into the subretinal space in geographic atrophy and this finding was observed also in retinal detachment.5 All these findings support that Müller cells are very mobile when stimulated by a “trauma”. For this reason, we hypothesize that in the presented diabetic patient, Müller cells have migrated into the subretinal space and have caused subretinal pseudocysts. On the other hand, we disclosed the presence of pooling of blood compressing the outer nuclear layer in the histological examination of another patient affected by diabetic retinopathy (Fig. 2). For this reason, we could not exclude that subretinal pseudocyst detected by structural OCT may represent a pooling of blood that is compressing the outer nuclear layer, although blood is usually characterized by a more hyperreflective appearance at structural OCT. Similar findings were also detected by our group in a patient affected by exudative age-related macular degeneration.6
Fig. 2.
Histological macular appearance in another eye affected by diabetic retinopathy (an 83 yo subject). Tissue was fixed in 4% paraformaldehyde solution within 7 hours of death. An 8 mm diameter punch including neural retina, choroid and sclera was collected, centered on the fovea centralis. The punch underwent cryopreservation through a series of sucrose solutions followed by embedding in optimal cutting temperature compound (Ted Pella) and freezing in liquid nitrogen. Cryostat sections were collected at a thickness of 7 μm onto Superfrost plus slides (Fisher) and were stained with hematoxylin/eosin stain.
Multiple cysts are present within the outer plexiform layer, as observed in classical DME. However, below these cysts are pseudocysts between the photoreceptors and the RPE monolayer, which is artifactually noncontinuous. Wherever the pseudocyst is present, the outer nuclear layer is compressed and degenerated to as little as one nucleus thick, suggesting compression on and toxicity to the photoreceptor cells. The ONL is present with inner and outer segments in the center where the pseudocysts are not present.
4. Conclusions
This case describes for the first time the occurrence of cystoid spaces inside the subretinal fluid on structural OCT, namely subretinal pseudocysts.
Patient consent
The patient provided written informed consent for publication of this case report and any accompanying images.
Funding
No funding or grant support.
Authorship
All authors attest that they meet the current ICMJE criteria for Authorship.
Declaration of competing interest
Riccardo Sacconi: none.
Gerard A. Lutty: none.
Robert F. Mullins: none.
Enrico Borrelli: none.
Francesco Bandello consultant for: Alcon (Fort Worth, Texas,USA), Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc (Irvine, California,USA), Farmila-Thea (Clermont-Ferrand, France), Bayer Shering-Pharma (Berlin, Germany), Bausch And Lomb (Rochester, New York, USA), Genentech (San Francisco, California, USA), Hoffmann-La-Roche (Basel, Switzerland), NovagaliPharma (Évry, France), Novartis (Basel, Switzerland), Sanofi-Aventis (Paris, France), Thrombogenics (Heverlee, Belgium), Zeiss (Dublin, USA).
Giuseppe Querques consultant for: Alimera Sciences (Alpharetta, Georgia, USA), Allergan Inc (Irvine, California,USA), Bayer Shering-Pharma (Berlin, Germany), Heidelberg (Germany), Novartis (Basel, Switzerland), Sandoz (Berlin, Germany), Zeiss (Dublin, USA).
References
- 1.Spaide R.F. Retinal vascular cystoid macular edema: review and new theory. Retina. 2016;36(10):1823–1842. doi: 10.1097/IAE.0000000000001158. [DOI] [PubMed] [Google Scholar]
- 2.Gagnier J.J., Kienle G., Altman D.G. The CARE guidelines: consensus-based clinical case report guideline development. J Clin Epidemiol. 2014;67(1):46–51. doi: 10.1016/j.jclinepi.2013.08.003. [DOI] [PubMed] [Google Scholar]
- 3.Kashani A.H., Green K.M., Kwon J. Suspended scattering Particles in motion: a novel feature of OCT angiography in exudative maculopathies. Ophthalmol. Retina. 2018;2(7):694–702. doi: 10.1016/j.oret.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Edwards M.M., mcleod D.S., Bhutto I.A., Grebe R., Duffy M., Lutty G.A. Subretinal glial membranes in eyes with geographic atrophy. Investig Ophthalmol Vis Sci. 2017;58(3):1352–1367. doi: 10.1167/iovs.16-21229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis G.P., Chapin E.A., Luna G., Linberg K.A., Fisher S.K. The fate of Müller's glia following experimental retinal detachment: nuclear migration, cell division, and subretinal glial scar formation. Mol Vis. 2010;16:1361–1372. [PMC free article] [PubMed] [Google Scholar]
- 6.Sacconi R., Mullins R.F., Lutty G.A., Borrelli E., Bandello F., Querques G. Subretinal pseudocyst: a novel optical coherence tomography finding in age-related macular degeneration. Eur J Ophthalmol. 2019 doi: 10.1177/1120672119846437. [DOI] [PubMed] [Google Scholar]