Abstract
Introduction
Between 40,000 and 50,000 divers and swimmers are envenomated each year and diving as a hobby is becoming increasingly popular. In the Mediterranean, envenomation is most often by Weever fish, Scorpion fish and jellyfish but coral and sea urchins may also be venomous.
Envenomation
Most stings cause local inflammation, oedema and pain. The severity of pain varies with the venom and the amount injected. In severe cases, stings may be life-threatening due to cardiogenic or anaphylactic shock or penetration of vital structures.
Management
Most cases of envenomation are preventable with a combination of measures including the avoidance of contact through good buoyancy control, the wearing of body-suits, and by maintaining visual awareness. Immediate management is to return to the surface, elevate and wash the site of injury. Immersion in hot water followed by simple analgesics for pain relief has been shown to be more effective than other methods. More severe cases should be identified by symptoms including confusion and heavy bleeding and referred to qualified medical care.
Conclusion
Envenomation by subaquatic species is common and preventable yet the dissemination of the appropriate knowledge is limited. This knowledge summary provides pertinent information aimed at divers in preventing and managing such injuries.
Keywords: Marine animals, Diving, Treatment, First aid, Flow chart
Introduction
It is estimated that greater than 1,200 species of fish may be venomous[ 1] and many other marine species are known to also produce venom. These mostly inhabit tropical waters and several of these species are found in the Mediterranean. Symptoms of envenomation are typically pain, swelling and erythema but are wide ranging, from an innocuous and temporary burning sensation to shock, haemorrhage and rarely death depending on the type of venom, dose, individual patient and site of envenomation. Diving is rapidly growing in popularity and there are now estimated to be up to six million recreational divers globally.[ 2] Each year, between 40,000 and 50,000 divers and swimmers are envenomated,[ 3] some of which are fatal. In the Mediterranean, envenomation is most often by Weever fish, Scorpion fish and jellyfish but coral and sea urchins may also be venomous.[ 4]
'Venomous species' are defined as those which possess toxin-secreting glands and a mechanism capable of delivering this, such as a spine or tooth. This is distinct from 'poisonous species', where the toxin is present in the skin or flesh of the species and there is a lack of a delivery mechanism, meaning that ingestion of the poisonous species is the only means of transferring the toxin.
Venomous species are not aggressive but defensive, and only sting when threatened. Diving as a passive observer of subaquatic life rather than attempting to touch it is an effective avoidance measure. Awareness of the risk and the adoption of simple measures can also help prevent envenomation.
A literature review and liaison with the British Royal Navy’s Institute of Naval Medicine identified a lack of concise resources available to the diver on the prevention and management of envenomation injury and on the quick identification of high-risk venomous subaquatic species. This work is intended to provide an overview of prehospital management of envenomation by subaquatic species with special reference to species endemic to the Mediterranean Sea.
Envenomation
The delivery of venom is by the insertion of a hypodermic delivery mechanism.[ 5] In most cases, this takes the form of a sharp barb, spine, or tooth which serves as a defence to an aggressor species. Jellyfish are distinct as they have tentacles used to entrap and envenomate prey (all described further below). Once the hypodermic mechanism is inserted, a toxin-producing gland at its base secretes toxins which are transferred through the mechanism and into the aggressor. From here the toxin enters the circulation and lymphatic system causing localised and sometimes systemic effects.
The means of delivery are various. Stingrays have a whip-like barbed tail that stabs a victim with force causing a deep wound. This causes traumatic injury as well as envenomation.[ 6] Stingrays are bottom dwellers and so envenomation in humans often follows accidental treading on the ray in shallow water. This means wounds are often to the legs but can be to the thorax and abdomen. Deaths have occurred when wounds to the chest have resulted in heart penetration.
Fish possess sharp spines which cause minor penetrative injury to the site and local pain. Once inserted, the spine sheath ruptures and the venom is released into the wound. Like stingrays, many venomous fish (e.g., Weever fish), are bottom feeders and may cause envenomation when stepped on. Minor lacerations from penetrative trauma are concomitant. A notable exception and newcomer to the Mediterranean is the Lionfish, which swims above the seabed and has a very noticeable fan-like appearance and dangerous sting.
Jellyfish have a complex venom containing various enzymes and proteins which cause pain and sometimes systemic effects. They do not cause puncture wounds but discharge venom into the skin through thousands of tiny hypodermic spines called ‘nematocysts’. Patients often have multiple stings from long tentacles which can mean delivery of a large dose of venom.[ 4] Jellyfish are slow, translucent and inhabit much of the water column. This makes them pervasive and difficult to spot, meaning divers may be stung by swimming into the jellyfish by accident. Most stings are mild, however potent stingers include the Portuguese man o’ war and Mediterranean box jellyfish, both of which cause extremely painful stings. It should be noted that the Mediterranean box jellyfish is distinct from other species of box jellyfish found elsewhere in the world which possess potentially fatal stings.
Finally, sea urchins reside on the seabed and have extremely sharp barbs which snap off on penetration and cause multiple wounds. They easily puncture body suits and injury is often local to the lower leg and foot due to being trodden on.[ 7]
Symptoms
LOCAL EFFECTS
Most stings cause local inflammation, swelling and pain. The severity of pain varies with the venom and the amount injected and may last from one hour to more than a day, and often resolves spontaneously. The severity of the sting is determinant on the envenomating species, the dose, site of envenomation and the individual physiology of the victim. The puncture site may contain a foreign body remnant from a stingray barb or sea urchin which may cause infection if left in situ. In the case of barbs, these are difficult to remove and attempts to do so may cause further damage unless removed by a medical professional.
SYSTEMIC EFFECTS
Some species are particularly venomous, including the Portuguese man o’ war jellyfish. Stings to the trunk and multiple stings may cause a systemic effect which may be life-threatening. Systemic symptoms include nausea, vomiting, headache, dizziness and low blood pressure. Allergic reactions may present on envenomation and in extreme cases this may develop to anaphylaxis (extreme allergic response) and shock.[ 8] However, it should be noted that this is rare, and even rarer in the Mediterranean.
Prevention
Many cases of envenomation occur in divers who were not wearing the appropriate protective clothing or inadvertently came in to contact with a venomous species. This may be through intentional touching on the part of the diver or by poor buoyancy control leading to contact with the sea bed and thus bottom dwelling species.
PROTECTION
Covering of bare skin and wearing of footwear is effective in preventing contact with many venomous spines and filaments. Full-body suits should always be worn, even in warmer waters. These can either be neoprene wetsuit, dry suit or lycra skin suit in warm water and include hood and gloves.[ 9] Exposure of the face is hard to avoid and it is therefore vulnerable to stinging, especially in the space between mask and regulator. This makes environmental awareness especially important.
BUOYANCY
Many species of venomous fish inhabit the sea bed in sand or rock and are often difficult to spot. For this reason, touching the seabed is unwise and avoided through good buoyancy control. Good buoyancy also minimises kicking of fins which also agitates the seabed and may also instigate defensive behaviour by any species making the area their home.
AWARENESS
Many stings, especially from jellyfish, occur due to inadvertently swimming into the venomous species. Divers should take special care to look in the direction they are headed, including during ascent, in order to maintain visual awareness.[ 10]
TOUCHING
Do not touch. This is a general rule for divers to avoid damage to subaquatic life but is especially important in the avoidance of stings. Most fish are naturally shy and avoid an approaching diver by swimming to a safer distance. However, if a fish does not retreat from you or adopts a defensive posture, it may be that it has an alternative defensive mechanism such as venom. In this situation it is best for the diver to move away.
Immediate management
If stung during a dive, immediate action should be taken to return to the surface (Figure 1).[ 5] This is for several reasons. Firstly, to reduce the risk of further envenomation. Secondly, the physiological effects of the toxin are unlikely to be known and it is therefore safest to return to the surface where the air supply is not dependent on the user being conscious and on delivery by breathing apparatus. Finally, medical treatment will be located ashore or aboard.
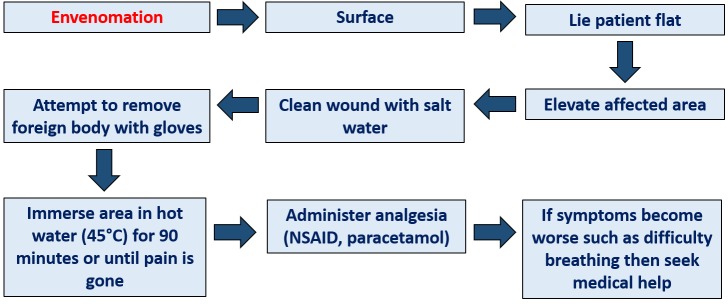
Figure 1.
Schematic of pre-hospital care of a patient with envenomation injury
On surfacing, the affected area should be elevated to reduce blood flow to the area and thereby reduce inflammation and swelling.[ 5] The area should be rinsed with sea water to remove any toxin which may still be at the surface and any foreign body carefully removed if possible. A caveat to this is stingray wounds where any barb remnant should be removed only by a medical professional due to the risk of bleeding. Jelly fish stings should not be rubbed to avoid stimulating injection of further toxin. The affected area plus some contiguous unaffected skin (or another unaffected part of the body) should be immersed in hot water of not more than 45°C for up to 2 hours or until the pain subsides. Hot water immersion has proved more effective at pain reduction than both vinegar and cold water in multiple studies.[ 4] Most toxins are heat labile and will be denatured in heat. The insertion of unaffected skin is to avoid inadvertent scolding if the effect of the toxin is to numb the affected area to sensation.
Pain relief may be given. This should initially be paracetamol or non-steroidal anti-inflammatory drugs (NSAIDs) such as aspirin and ibuprofen.[ 11] The wound should be cleaned with salt water to prevent infection. Further medical attention should considered if the pain cannot be controlled.
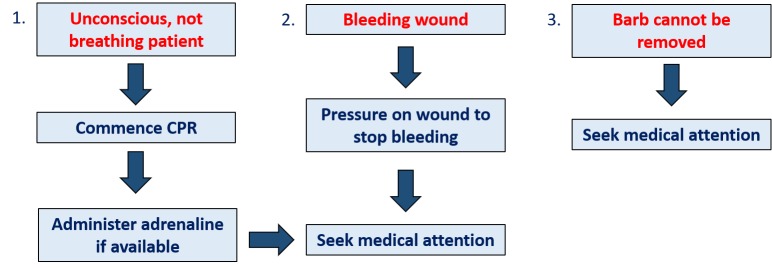
In rarer cases further management is needed (Figure 2). Where the wound is deep, such as with stingray, copious bleeding may occur. This should be stopped by applying pressure to the wound and dressing with bandages, and medical attention sought. Even where there is minimal bleeding, stingray wounds should always be reviewed by a medical practitioner as there is a risk of subsequent infection.
Figure 2.
Schematic of pre-hospital care of a patient with serious envenomation injury
If the patient displays confusion, drowsiness or any other worsening of symptoms medical attention should be sought immediately. These are systemic symptoms and may be a sign of anaphylaxis or shock. Under these circumstances cardiopulmonary resuscitation may be required if the patient becomes unconscious and stops breathing. Adrenaline should be administered if available for cardiac arrest or anaphylaxis.
Conclusion
Envenomation by subaquatic species is common and preventable yet the dissemination of the appropriate knowledge is limited. This is compounded by the non-availability of a concise and usable resource for divers to be used before and while diving. This knowledge summary provides pertinent information aimed at the layman and is a document of intent for a portable publication on prevention, identification and prehospital management of subaquatic envenomation in the Mediterranean.
Footnotes
Acknowledgements
Thanks are due to the Royal Navy Institute of Naval Medicine for collaborating on the project.
Conflicts of interest and funding: nil
Contributor Information
James Todd, St George’s University of London, Tooting, London, UK.
Mark Edsell, Department of Anaesthetics, St George’s Hospital, London, UK.
References
- Smith WL, Wheeler WC. Venom evolution widespread in fishes: a phylogenetic road map for the bioprospecting piscine venoms . J Hered. 2006;97:206–17. doi: 10.1093/jhered/esj034. [DOI] [PubMed] [Google Scholar]
- Diving Equipment and Marketing Association . Fast Facts: Recreational scuba diving and snorkelling. [Internet]. 2018 . [cited 2018 Nov 01]. Available from: https://www.dema.org/store/download.aspx?id=7811B097-8882-4707-A160-F999B49614B6.
- Auerbach PS. Trauma and envenomations from marine fauna In: Tintinalli JE, Kelen GD, Stapczynski JS. . Emergency Medicine: A Comprehensive Study Guide. 5th ed. New York: American College of Emergency Physicians; 1999. p. 1256- 61. [Google Scholar]
- Atkinson PR, Boyle A, Hartin D, McAuley D. Is hot water immersion an effective treatment for marine envenomation? . Emerg Med J. 2006;23:503–8. doi: 10.1136/emj.2005.028456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edwards C, Lowry C, Pennefather J, Walker R. Diving and Subaquatic Medicine. 4th ed. Boca Raton (FL): CRC Press; 2005. [Google Scholar]
- Clark RF, Girard RH, Rao D, Ly BT, Davis DP. Stingray envenomation: a retrospective review of clinical presentation and treatment in 119 cases . J Emerg Med. 2007;33:33–7. doi: 10.1016/j.jemermed.2007.03.043. [DOI] [PubMed] [Google Scholar]
- Morocco A. Sea urchin envenomation . Clin Toxicol (Phila). 2005;43:119–20. [PubMed] [Google Scholar]
- Stein MR, Marraccini JV, Rothschild NE, Burnett JW. Fatal Portuguese man-o’-war (Physalia physalis) envenomation . Ann Emerg Med. 1989;18:312–5. doi: 10.1016/s0196-0644(89)80421-4. [DOI] [PubMed] [Google Scholar]
- Diaz JH. Marine scorpaenidae envenomation in travelers: epidemiology, management, and prevention . J Trav Med. 2015;22:251–8. doi: 10.1111/jtm.12206. [DOI] [PubMed] [Google Scholar]
- Montgomery L, Seyes J, Mees J. To pee, or not to pee: A review on envenomation and treatment in European jellyfish species . Mar Drugs. 2016;14:pii:E127. doi: 10.3390/md14070127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weinstein S, Dart R, Staples A, White J. Envenomations: an overview of clinical toxinology for the primary care physician . Am Fam Physician. 2009;80:793–802. [PubMed] [Google Scholar]