Figure.
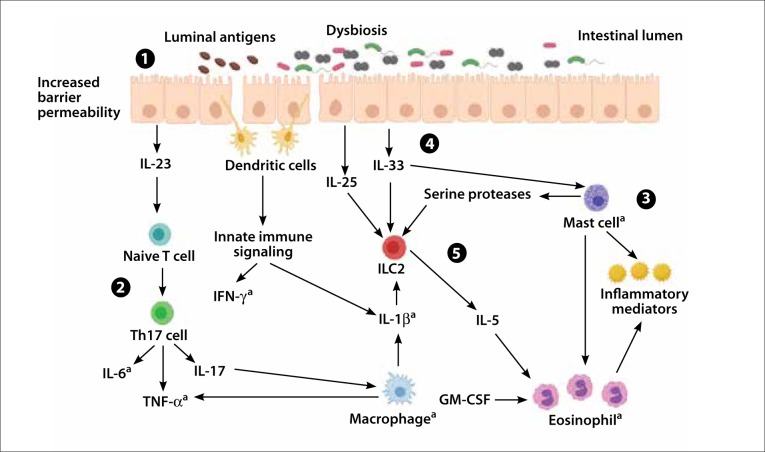
Hypothesized immune responses and links to FGIDs. The hypothesis of FGIDs as disorders of gastrointestinal homeostatic imbalance suggests that Th17 and ILC2 pathways warrant investigation as mediators of underlying immune activation. In homeostasis, Th17 cells exist in a balance with regulatory T cells, and ILC3s are involved in suppression of immune responses. Stimulation of the immune system by antigens or alterations in the microbiota (1) contributes to increased barrier permeability. This interruption drives the maturation of Th17 cells (2), which produce IL-6, TNF-α, and IL-17. IL-17 has been shown to induce macrophages in patients with asthma and is capable of secreting IL-1β. IL-33 facilitates increased mast cell activity, which is capable of driving eosinophil recruitment (3). Additionally, IL-25, IL-33, IL-1β, and serine proteases influence the expansion of ILC2 populations (4), disrupting ILC3 homeostasis. ILC2 populations drive further eosinophil recruitment through activity of IL-5 (5). This inflammatory environment, driven by cytokine activity and release of inflammatory mediators, may contribute to the symptoms reported by FGID patients.
aDenotes factor identified in the literature as altered in FGID cohorts.
FGID, functional gastrointestinal disorder; GM-CSF, granulocyte-macrophage colony-stimulating factor; IFN, interferon; IL, interleukin; ILC, innate lymphoid cell; Th, T helper type; TNF, tumor necrosis factor.