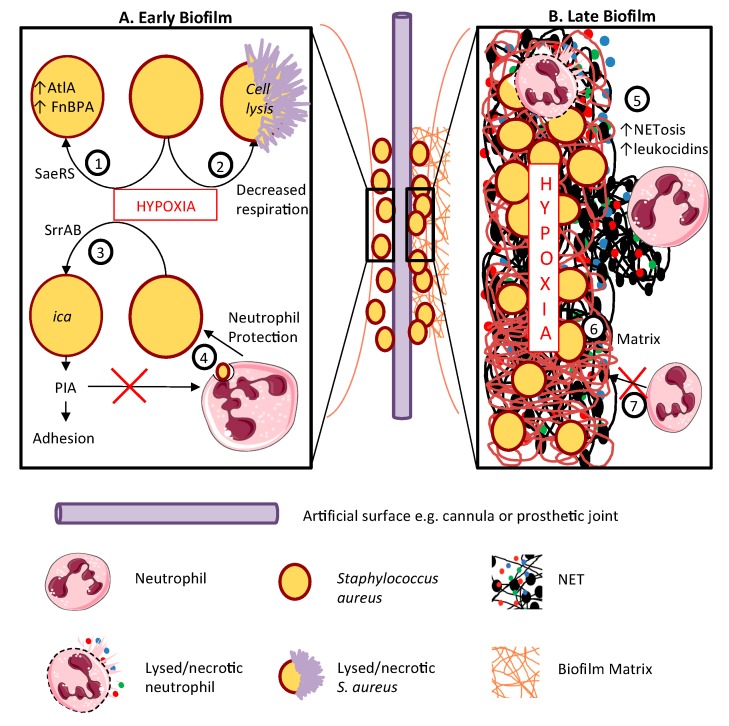
Figure 3.
Hypoxia enhances staphylococcal biofilm development. Biofilms are most likely to form on prosthetic surfaces such as intravenous cannulae or replacement joints or heart valves. The host and pathogen processes contributing to biofilm formation are depicted in the left-hand panel A. Panel B (right) depicts the role of hypoxia in biofilm maintenance and progression. A. In early biofilm development, hypoxia activates the SaeRS 2- component system, increasing AtlA and FnBPA production (1); decreases staphylococcal respiration, potentially resulting in cell death and lysis (2); and activates the PIA (polysaccharide intercellular adhesion encoding operon (ica) via the SrrAB regulator (3), increasing biofilm adhesion. PIA accumulation also impairs neutrophil non-oxidative killing (4). B. Mature biofilms are profoundly hypoxic, promoting NETosis and leukocidin production (5) adding to the polymeric biofilm matrix of polysaccharides, proteins and lipids, entangling multiplying staphylococci (6). This matrix blocks the entry of neutrophils into the biofilm (7). This figure was created using Servier Medical Art templates, which are licensed under a Creative Commons Attribution 3.0 Unported License; https://smart.servier.com.